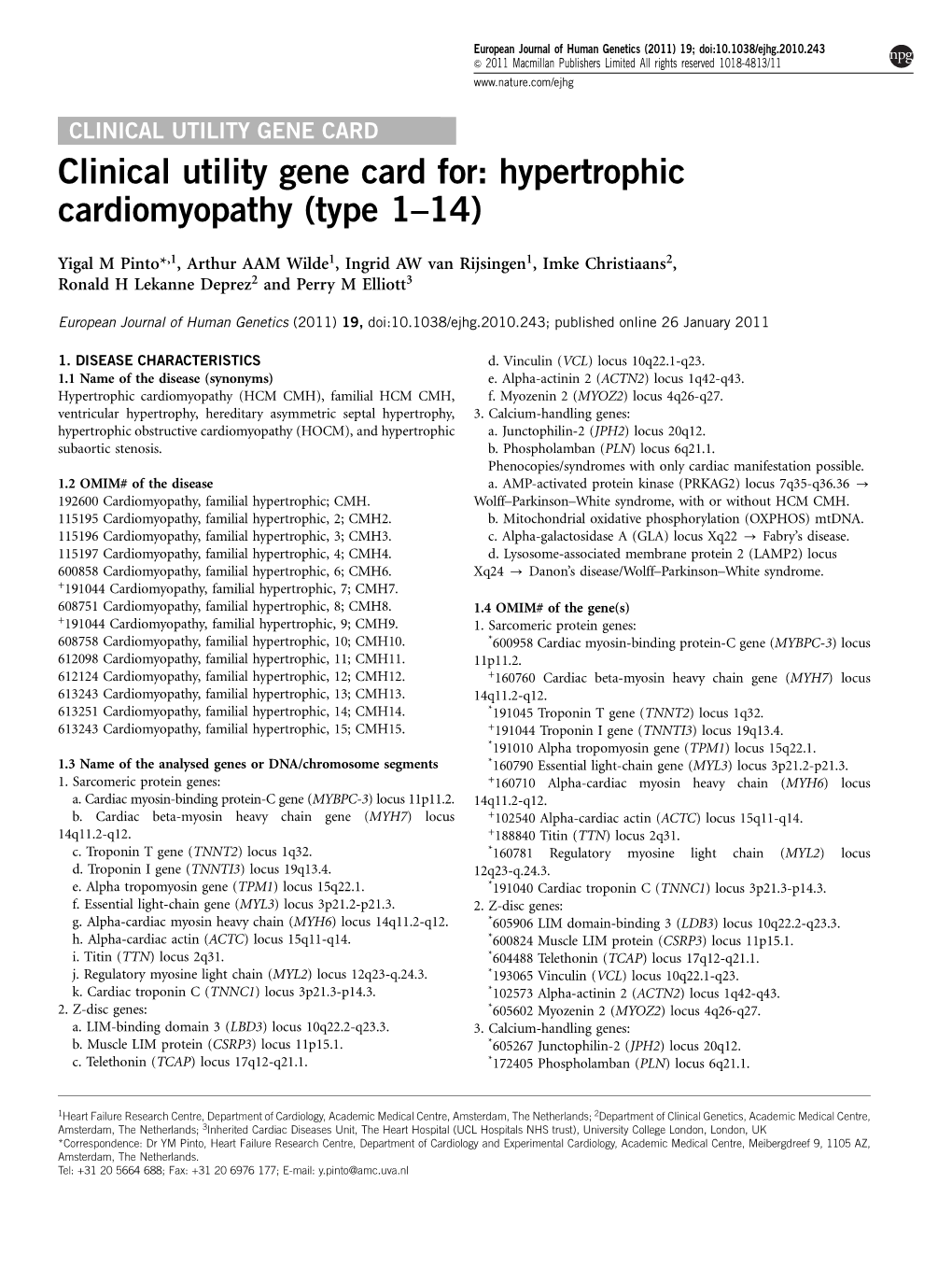
Hypertrophic Cardiomyopathy (Type 1–14)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Identification of the Binding Partners for Hspb2 and Cryab Reveals
Brigham Young University BYU ScholarsArchive Theses and Dissertations 2013-12-12 Identification of the Binding arP tners for HspB2 and CryAB Reveals Myofibril and Mitochondrial Protein Interactions and Non- Redundant Roles for Small Heat Shock Proteins Kelsey Murphey Langston Brigham Young University - Provo Follow this and additional works at: https://scholarsarchive.byu.edu/etd Part of the Microbiology Commons BYU ScholarsArchive Citation Langston, Kelsey Murphey, "Identification of the Binding Partners for HspB2 and CryAB Reveals Myofibril and Mitochondrial Protein Interactions and Non-Redundant Roles for Small Heat Shock Proteins" (2013). Theses and Dissertations. 3822. https://scholarsarchive.byu.edu/etd/3822 This Thesis is brought to you for free and open access by BYU ScholarsArchive. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of BYU ScholarsArchive. For more information, please contact [email protected], [email protected]. Identification of the Binding Partners for HspB2 and CryAB Reveals Myofibril and Mitochondrial Protein Interactions and Non-Redundant Roles for Small Heat Shock Proteins Kelsey Langston A thesis submitted to the faculty of Brigham Young University in partial fulfillment of the requirements for the degree of Master of Science Julianne H. Grose, Chair William R. McCleary Brian Poole Department of Microbiology and Molecular Biology Brigham Young University December 2013 Copyright © 2013 Kelsey Langston All Rights Reserved ABSTRACT Identification of the Binding Partners for HspB2 and CryAB Reveals Myofibril and Mitochondrial Protein Interactors and Non-Redundant Roles for Small Heat Shock Proteins Kelsey Langston Department of Microbiology and Molecular Biology, BYU Master of Science Small Heat Shock Proteins (sHSP) are molecular chaperones that play protective roles in cell survival and have been shown to possess chaperone activity. -

The Role of Z-Disc Proteins in Myopathy and Cardiomyopathy
International Journal of Molecular Sciences Review The Role of Z-disc Proteins in Myopathy and Cardiomyopathy Kirsty Wadmore 1,†, Amar J. Azad 1,† and Katja Gehmlich 1,2,* 1 Institute of Cardiovascular Sciences, College of Medical and Dental Sciences, University of Birmingham, Birmingham B15 2TT, UK; [email protected] (K.W.); [email protected] (A.J.A.) 2 Division of Cardiovascular Medicine, Radcliffe Department of Medicine and British Heart Foundation Centre of Research Excellence Oxford, University of Oxford, Oxford OX3 9DU, UK * Correspondence: [email protected]; Tel.: +44-121-414-8259 † These authors contributed equally. Abstract: The Z-disc acts as a protein-rich structure to tether thin filament in the contractile units, the sarcomeres, of striated muscle cells. Proteins found in the Z-disc are integral for maintaining the architecture of the sarcomere. They also enable it to function as a (bio-mechanical) signalling hub. Numerous proteins interact in the Z-disc to facilitate force transduction and intracellular signalling in both cardiac and skeletal muscle. This review will focus on six key Z-disc proteins: α-actinin 2, filamin C, myopalladin, myotilin, telethonin and Z-disc alternatively spliced PDZ-motif (ZASP), which have all been linked to myopathies and cardiomyopathies. We will summarise pathogenic variants identified in the six genes coding for these proteins and look at their involvement in myopathy and cardiomyopathy. Listing the Minor Allele Frequency (MAF) of these variants in the Genome Aggregation Database (GnomAD) version 3.1 will help to critically re-evaluate pathogenicity based on variant frequency in normal population cohorts. -

Genetic Mutations and Mechanisms in Dilated Cardiomyopathy
Genetic mutations and mechanisms in dilated cardiomyopathy Elizabeth M. McNally, … , Jessica R. Golbus, Megan J. Puckelwartz J Clin Invest. 2013;123(1):19-26. https://doi.org/10.1172/JCI62862. Review Series Genetic mutations account for a significant percentage of cardiomyopathies, which are a leading cause of congestive heart failure. In hypertrophic cardiomyopathy (HCM), cardiac output is limited by the thickened myocardium through impaired filling and outflow. Mutations in the genes encoding the thick filament components myosin heavy chain and myosin binding protein C (MYH7 and MYBPC3) together explain 75% of inherited HCMs, leading to the observation that HCM is a disease of the sarcomere. Many mutations are “private” or rare variants, often unique to families. In contrast, dilated cardiomyopathy (DCM) is far more genetically heterogeneous, with mutations in genes encoding cytoskeletal, nucleoskeletal, mitochondrial, and calcium-handling proteins. DCM is characterized by enlarged ventricular dimensions and impaired systolic and diastolic function. Private mutations account for most DCMs, with few hotspots or recurring mutations. More than 50 single genes are linked to inherited DCM, including many genes that also link to HCM. Relatively few clinical clues guide the diagnosis of inherited DCM, but emerging evidence supports the use of genetic testing to identify those patients at risk for faster disease progression, congestive heart failure, and arrhythmia. Find the latest version: https://jci.me/62862/pdf Review series Genetic mutations and mechanisms in dilated cardiomyopathy Elizabeth M. McNally, Jessica R. Golbus, and Megan J. Puckelwartz Department of Human Genetics, University of Chicago, Chicago, Illinois, USA. Genetic mutations account for a significant percentage of cardiomyopathies, which are a leading cause of conges- tive heart failure. -

Anti-MYOZ2 (GW22350F)
3050 Spruce Street, Saint Louis, MO 63103 USA Tel: (800) 521-8956 (314) 771-5765 Fax: (800) 325-5052 (314) 771-5757 email: [email protected] Product Information Anti-MYOZ2 antibody produced in chicken, affinity isolated antibody Catalog Number GW22350F Formerly listed as GenWay Catalog Number 15-288-22350F, Myozenin-2 Antibody. – Storage Temperature Store at 20 °C The product is a clear, colorless solution in phosphate buffered saline, pH 7.2, containing 0.02% sodium azide. Synonyms: Myozenin 2, Calsarcin-1; FATZ-related protein 2 Species Reactivity: Human Product Description Myozenins may serve as intracellular binding proteins Tested Applications: WB involved in linking Z-disk proteins such as alpha-actinin. Recommended Dilutions: Recommended starting dilution gamma-filamin. TCAP/telethonin. LDB3/ZASP and localizing for Western blot analysis is 1:500, for tissue or cell staining calcineurin signaling to the sarcomere. Plays an important 1:200. role in the modulation of calcineurin signaling. May play a role in myofibrillogenesis. Note: Optimal concentrations and conditions for each application should be determined by the user. NCBI Accession number: NP_057683.1 Swiss Prot Accession number: Q9NPC6 Precautions and Disclaimer This product is for R&D use only, not for drug, household, or Gene Information: Human .. MYOZ2 (51778) other uses. Due to the sodium azide content a material Immunogen: Recombinant protein Myozenin 2 safety data sheet (MSDS) for this product has been sent to the attention of the safety officer of your institution. Please Immunogen Sequence: GI # 7706595, sequence 1 - 264 consult the Material Safety Data Sheet for information regarding hazards and safe handling practices. -

Novel Pathogenic Variants in Filamin C Identified in Pediatric Restrictive Cardiomyopathy
Novel pathogenic variants in filamin C identified in pediatric restrictive cardiomyopathy Jeffrey Schubert1, 2, Muhammad Tariq3, Gabrielle Geddes4, Steven Kindel4, Erin M. Miller5, and Stephanie M. Ware2. 1 Department of Molecular Genetics, Microbiology, and Biochemistry, University of Cincinnati College of Medicine, Cincinnati, OH; 2 Departments of Pediatrics and Medical and Molecular Genetics, Indiana University School of Medicine, Indianapolis, IN; 3 Faculty of Applied Medical Science, University of Tabuk, Tabuk, Kingdom of Saudi Arabia; 4Department of Pediatrics, Medical College of Wisconsin, Milwaukee, WI; 5Cincinnati Children’s Hospital Medical Center, Cincinnati, OH. Correspondence: Stephanie M. Ware, MD, PhD Department of Pediatrics Indiana University School of Medicine 1044 W. Walnut Street Indianapolis, IN 46202 Telephone: 317 274-8939 Email: [email protected] Grant Sponsor: The project was supported by the Children’s Cardiomyopathy Foundation (S.M.W.), an American Heart Association Established Investigator Award 13EIA13460001 (S.M.W.) and an AHA Postdoctoral Fellowship Award 12POST10370002 (M.T.). ___________________________________________________________________ This is the author's manuscript of the article published in final edited form as: Schubert, J., Tariq, M., Geddes, G., Kindel, S., Miller, E. M., & Ware, S. M. (2018). Novel pathogenic variants in filamin C identified in pediatric restrictive cardiomyopathy. Human Mutation, 0(ja). https://doi.org/10.1002/humu.23661 Abstract Restrictive cardiomyopathy (RCM) is a rare and distinct form of cardiomyopathy characterized by normal ventricular chamber dimensions, normal myocardial wall thickness, and preserved systolic function. The abnormal myocardium, however, demonstrates impaired relaxation. To date, dominant variants causing RCM have been reported in a small number of sarcomeric or cytoskeletal genes, but the genetic causes in a majority of cases remain unexplained especially in early childhood. -
Disrupted Mechanobiology Links the Molecular and Cellular Phenotypes
bioRxiv preprint doi: https://doi.org/10.1101/555391; this version posted February 21, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 1 Disrupted Mechanobiology Links the Molecular and Cellular 2 Phenotypes in Familial Dilated Cardiomyopathy 3 4 Sarah R. Clippinger1,2, Paige E. Cloonan1,2, Lina Greenberg1, Melanie Ernst1, W. Tom 5 Stump1, Michael J. Greenberg1,* 6 7 1 Department of Biochemistry and Molecular Biophysics, Washington University School 8 of Medicine, St. Louis, MO, 63110, USA 9 10 2 These authors contributed equally to this work 11 12 *Corresponding author: 13 Michael J. Greenberg 14 Department of Biochemistry and Molecular Biophysics 15 Washington University School of Medicine 16 660 S. Euclid Ave., Campus Box 8231 17 St. Louis, MO 63110 18 Phone: (314) 362-8670 19 Email: [email protected] 20 21 22 Running title: A DCM mutation disrupts mechanosensing 23 24 25 Keywords: Mechanosensing, stem cell derived cardiomyocytes, muscle regulation, 26 troponin, myosin, traction force microscopy 1 bioRxiv preprint doi: https://doi.org/10.1101/555391; this version posted February 21, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 27 Abstract 28 Familial dilated cardiomyopathy (DCM) is a leading cause of sudden cardiac death and a 29 major indicator for heart transplant. The disease is frequently caused by mutations of 30 sarcomeric proteins; however, it is not well understood how these molecular mutations 31 lead to alterations in cellular organization and contractility. -

Profiling of the Muscle-Specific Dystroglycan Interactome Reveals the Role of Hippo Signaling in Muscular Dystrophy and Age-Dependent Muscle Atrophy Andriy S
Yatsenko et al. BMC Medicine (2020) 18:8 https://doi.org/10.1186/s12916-019-1478-3 RESEARCH ARTICLE Open Access Profiling of the muscle-specific dystroglycan interactome reveals the role of Hippo signaling in muscular dystrophy and age-dependent muscle atrophy Andriy S. Yatsenko1†, Mariya M. Kucherenko2,3,4†, Yuanbin Xie2,5†, Dina Aweida6, Henning Urlaub7,8, Renate J. Scheibe1, Shenhav Cohen6 and Halyna R. Shcherbata1,2* Abstract Background: Dystroglycanopathies are a group of inherited disorders characterized by vast clinical and genetic heterogeneity and caused by abnormal functioning of the ECM receptor dystroglycan (Dg). Remarkably, among many cases of diagnosed dystroglycanopathies, only a small fraction can be linked directly to mutations in Dg or its regulatory enzymes, implying the involvement of other, not-yet-characterized, Dg-regulating factors. To advance disease diagnostics and develop new treatment strategies, new approaches to find dystroglycanopathy-related factors should be considered. The Dg complex is highly evolutionarily conserved; therefore, model genetic organisms provide excellent systems to address this challenge. In particular, Drosophila is amenable to experiments not feasible in any other system, allowing original insights about the functional interactors of the Dg complex. Methods: To identify new players contributing to dystroglycanopathies, we used Drosophila as a genetic muscular dystrophy model. Using mass spectrometry, we searched for muscle-specific Dg interactors. Next, in silico analyses allowed us to determine their association with diseases and pathological conditions in humans. Using immunohistochemical, biochemical, and genetic interaction approaches followed by the detailed analysis of the muscle tissue architecture, we verified Dg interaction with some of the discovered factors. -

MYL3 Monoclonal ANTIBODY Catalog Number:66286-1-Ig
For Research Use Only MYL3 Monoclonal ANTIBODY www.ptglab.com Catalog Number:66286-1-Ig Catalog Number: GenBank Accession Number: Purification Method: Basic Information 66286-1-Ig BC009790 Protein G purification Size: GeneID (NCBI): CloneNo.: 150UL , Concentration: 1000 μg/ml by 4634 2E4B2 Bradford method using BSA as the Full Name: Recommended Dilutions: standard; myosin, light chain 3, alkali; WB 1:5000-1:50000 Source: ventricular, skeletal, slow IHC 1:20-1:200 Mouse Calculated MW: Isotype: 22 kDa IgG1 Observed MW: Immunogen Catalog Number: 22-25 kDa AG24535 Applications Tested Applications: Positive Controls: IHC, WB, ELISA WB : human skeletal muscle tissue, mouse heart tissue Species Specificity: IHC : human heart tissue, human skeletal muscle human, rat, mouse, pig tissue Note-IHC: suggested antigen retrieval with TE buffer pH 9.0; (*) Alternatively, antigen retrieval may be performed with citrate buffer pH 6.0 MYL3, also named as MLC1v, is an essential light chain of myosin that is associated with muscle contraction. It is Background Information expressed in ventricular and slow skeletal muscle. MYL3 may serve as a target for caspase-3 in dying cardiomyocytes. Mutations of MYL3 gene cause hypertrophic cardiomyopathy. MYL3 has been identified as potential serum biomarker for drug induced myotoxicity. Great increase in MYL3 serum concentration has been observed in rats with cardiac and skeletal muscle injury. (PMID:21685905) Storage: Storage Store at -20°C. Stable for one year after shipment. Storage Buffer: PBS with 0.02% sodium azide and 50% glycerol pH 7.3. Aliquoting is unnecessary for -20ºC storage For technical support and original validation data for this product please contact: This product is exclusively available under Proteintech T: 1 (888) 4PTGLAB (1-888-478-4522) (toll free E: [email protected] Group brand and is not available to purchase from any in USA), or 1(312) 455-8498 (outside USA) W: ptglab.com other manufacturer. -

Mutations in MYOZ1 As Well As MYOZ2 Encoding the Calsarcins Are Not Associated with Idiopathic and Familial Dilated Cardiomyopathy
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by MDC Repository Repository of the Max Delbrück Center for Molecular Medicine (MDC) Berlin (Germany) http://edoc.mdc-berlin.de/8815/ Mutations in MYOZ1 as well as MYOZ2 encoding the calsarcins are not associated with idiopathic and familial dilated cardiomyopathy Maximilian G. Posch, Andreas Perrot, Rainer Dietz, Cemil Özcelik, Sabine Pankuweit, Volker Ruppert, Anette Richter, and Bernhard Maisch Published in final edited form as: Molecular Genetics and Metabolism. 2007 Jun; 91(2): 207-208 doi: 10.1016/j.ymgme.2007.02.014 Elsevier (The Netherlands) ► Letter to the editor Mutations in MYOZ1 as well as MYOZ2 encoding the calsarcins are not associated with idiopathic and familial dilated cardiomyopathy Maximilian G. Posch, Andreas Perrot, Rainer Dietz, Cemil Özcelik, Sabine Pankuweit, Volker Ruppert, Anette Richter, and Bernhard Maisch 1 Charité – Universitätsmedizin Berlin/Cardiology at Campus Buch & Virchow Klinikum, Helios-Kliniken and Max- Delbrück Center for Molecular Medicine, Wiltbergstrasse 50, 13125 Berlin, Germany 2 Department of Internal Medicine and Cardiology, Philipps University Marburg, Baldingerstrasse, 35043 Marburg, Germany a very weak mRNA expression of MYOZ1 [5]. Conversely, Dear Editor, MYOZ2 encoding calsarcin-1 is predominantly expressed We have read the article of Arola and colleagues [1] with in cardiomyocytes and to lesser extends in skeletal great interest. The authors report a candidate gene muscle [5,6]. Calsarcin-1 is located at the sarcomeric Z- approach in the MYOZ1 gene encoding calsarcin-2 in 185 disk and interacts with DCM disease genes like telethonin patients with idiopathic dilated cardiomyopathy (iDCM). -

Hypertrophic Cardiomyopathy- Associated Mutations in Genes That Encode Calcium-Handling Proteins
Current Molecular Medicine 2012, 12, 507-518 507 Beyond the Cardiac Myofilament: Hypertrophic Cardiomyopathy- Associated Mutations in Genes that Encode Calcium-Handling Proteins A.P. Landstrom and M.J. Ackerman* Departments of Medicine, Pediatrics, and Molecular Pharmacology & Experimental Therapeutics, Divisions of Cardiovascular Diseases and Pediatric Cardiology, and the Windland Smith Rice Sudden Death Genomics Laboratory, Mayo Clinic, Rochester, Minnesota, USA Abstract: Traditionally regarded as a genetic disease of the cardiac sarcomere, hypertrophic cardiomyopathy (HCM) is the most common inherited cardiovascular disease and a significant cause of sudden cardiac death. While the most common etiologies of this phenotypically diverse disease lie in a handful of genes encoding critical contractile myofilament proteins, approximately 50% of patients diagnosed with HCM worldwide do not host sarcomeric gene mutations. Recently, mutations in genes encoding calcium-sensitive and calcium- handling proteins have been implicated in the pathogenesis of HCM. Among these are mutations in TNNC1- encoded cardiac troponin C, PLN-encoded phospholamban, and JPH2-encoded junctophilin 2 which have each been associated with HCM in multiple studies. In addition, mutations in RYR2-encoded ryanodine receptor 2, CASQ2-encoded calsequestrin 2, CALR3-encoded calreticulin 3, and SRI-encoded sorcin have been associated with HCM, although more studies are required to validate initial findings. While a relatively uncommon cause of HCM, mutations in genes that encode calcium-handling proteins represent an emerging genetic subset of HCM. Furthermore, these naturally occurring disease-associated mutations have provided useful molecular tools for uncovering novel mechanisms of disease pathogenesis, increasing our understanding of basic cardiac physiology, and dissecting important structure-function relationships within these proteins. -

Myod Converts Primary Dermal Fibroblasts, Chondroblasts, Smooth
Proc. Natl. Acad. Sci. USA Vol. 87, pp. 7988-7992, October 1990 Developmental Biology MyoD converts primary dermal fibroblasts, chondroblasts, smooth muscle, and retinal pigmented epithelial cells into striated mononucleated myoblasts and multinucleated myotubes (myogenesis/myoflbrils/desmin/master switch genes) J. CHOI*, M. L. COSTAtt, C. S. MERMELSTEINtt, C. CHAGASt, S. HOLTZERt, AND H. HOLTZERt§ Departments of *Biochemistry and tAnatomy, University of Pennsylvania, Philadelphia, PA 19104; and tinstituto de Bioffsica Carlos Chagas Filho, Bloco G, Centro de Ciencias da Sadde, Universidade Federal do Rio de Janeiro, lbha do Funddo, 21941 Rio de Janeiro, Brazil Communicated by Harold Weintraub, June 29, 1990 (received for review June 15, 1990) ABSTRACT Shortly after their birth, postmitotic mono- L6, L8, L6E9, BC3H1, and other types of immortalized nucleated myoblasts in myotomes, limb buds, and conventional and/or mutagenized myogenic lines are induced to differen- muscle cultures elongate and assemble a cohort of myofibrillar tiate (9-13). proteins into definitively striated myofibrils. MyoD induces a MyoD induces a number of immortalized and/or trans- number of immortalized and/or transformed nonmuscle cells formed cell lines to express several myofibrillar genes and to to express desmin and several myofibrillar proteins and to fuse fuse into multinucleated myosacs (14-16). Other transformed into myosacs. We now report that MyoD converts normal lines such as kidney epithelial cells, HeLa cells, and some dermal fibroblasts, chondroblasts, gizzard smooth muscle, and hepatoma lines resist conversion. Judging from the published pigmented retinal epithelial cells into elongated postmitotic micrographs, MyoD-converted nonmuscle cells, like most mononucleated striated myoblasts. The sarcomeric localization myogenic cell lines, do not express the terminal myogenic of antibodies to desmin, a-actinin, titin, troponin-I, a-actin, program fully. -

Mini-Thin Filaments Regulated by Troponin–Tropomyosin
Mini-thin filaments regulated by troponin–tropomyosin Huiyu Gong*, Victoria Hatch†, Laith Ali‡, William Lehman†, Roger Craig§, and Larry S. Tobacman‡¶ *Department of Internal Medicine, University of Iowa, Iowa City, IA 52242; †Department of Physiology and Biophysics, Boston University, Boston, MA 02118; §Department of Cell Biology, University of Massachusetts, Worcester, MA 01655; and ‡Departments of Medicine and Physiology and Biophysics, University of Illinois at Chicago, Chicago, IL 60612 Edited by Edward D. Korn, National Institutes of Health, Bethesda, MD, and approved December 9, 2004 (received for review September 29, 2004) Striated muscle thin filaments contain hundreds of actin monomers normal-length thin filaments. They also would make possible and scores of troponins and tropomyosins. To study the coopera- approaches to thin-filament structural analysis. We report here tive mechanism of thin filaments, ‘‘mini-thin filaments’’ were the design and purification of mini-thin filaments with the generated by isolating particles nearly matching the minimal intended composition and compare their function to the function structural repeat of thin filaments: a double helix of actin subunits of conventional-length thin filaments. with each strand approximately seven actins long and spanned by Ca2ϩ regulates muscle contraction in the heart and in skeletal a troponin–tropomyosin complex. One end of the particles was muscle by binding to specific site(s) in the NH2 domain of the capped by a gelsolin (segment 1–3)–TnT fusion protein (substitut- troponin subunit, TnC. Significantly, Ca2ϩ activates tension very ing for normal TnT), and the other end was capped by tropomodu- cooperatively (3, 4) even in cardiac muscle, in which each TnC lin.