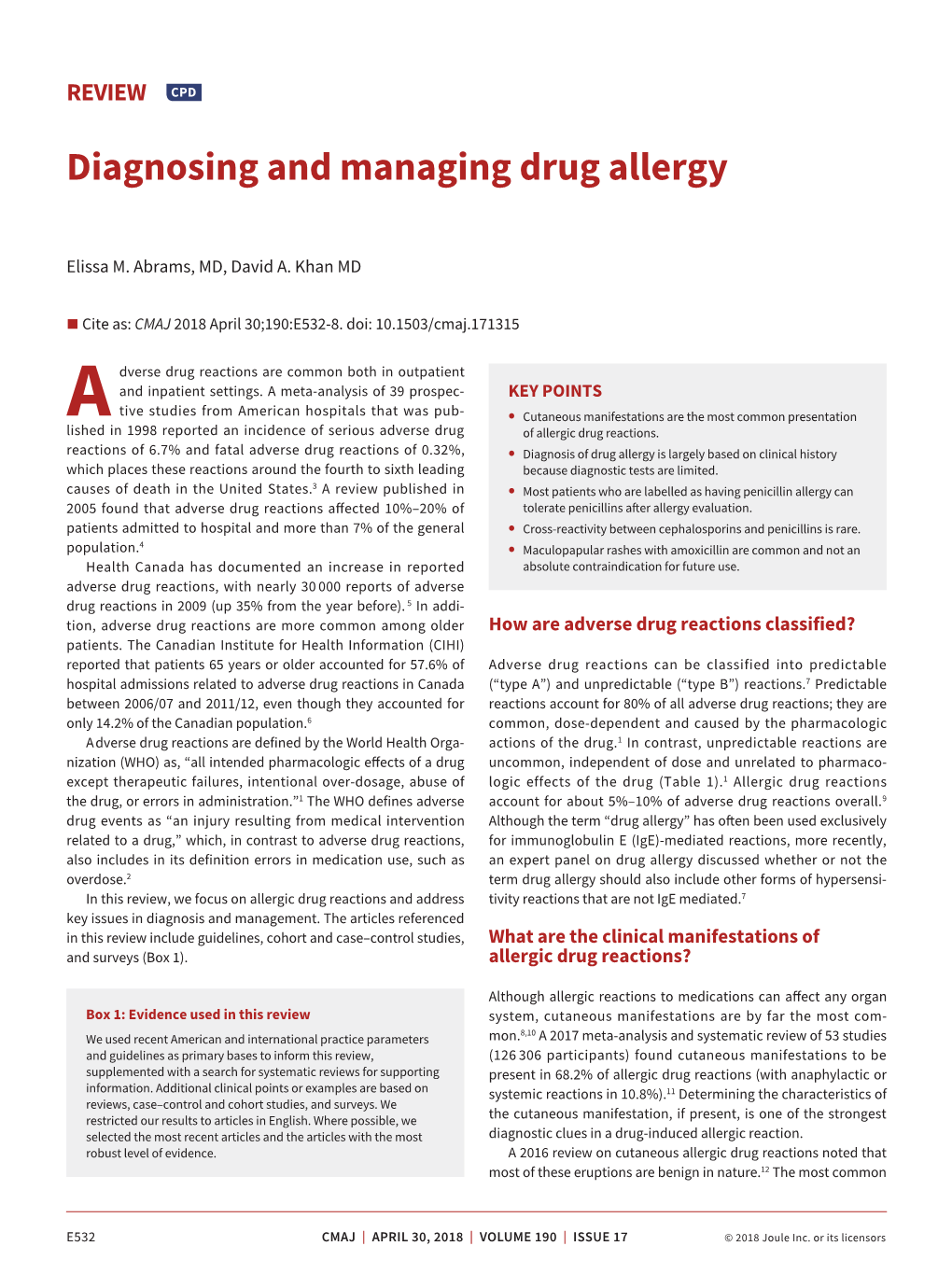
Diagnosing and Managing Drug Allergy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Rash During Procedural Sedation for Trimalleolar Fracture
Rash during Procedural Sedation for Trimalleolar Fracture Saint John, Emergency Medicine Case Rounds – 10 October, 2017 Dr. Jacqueline Hiob, BScPharm MD PGY1, FRCP Emergency Medicine Learning points for discussion around… • Response to possible drug reaction during procedural sedation • Options for avoiding or mitigating histamine release reactions to opioids Case 14 y/o M, healthy Fall from bicycle ~ 1 hour prior to presentation to ED No head injury, no LOC c/o pain and swelling R. ankle Unable to ambulate Transport by EMS – pt splinted on route, extremity NVI, Entonox for analgesia Case In the ED…. - Entonox Acetaminophen, Fentanyl - closed R. ankle injury, remains NVI - BP 145/72, P 90, S 96% RA, T 36.8 - off to xray he goes…. Imaging - Comminuted fractures, distal tibia + fibula - Apex medial and posterior angulation - Ankle and growth plate intact Case - Ortho consulted - Ortho R3 arrives in ED to assist with reduction - Full team: ED attending, ED resident, Emerg CC3, Ortho resident, RN, RN (training), RT, RT (student), LPN, X-Ray Tech Case Balanced Procedural Sedation with…. - Fentanyl - Ketamine - Propofol Case - ~ 20 minutes into procedure, macular rash noted over patients chest, progressing over abdomen - - no airway involvement, no hypotension or tachycardia - - decision made to treat with IV diphenhydramine and have epinephrine on hand ** smaller area of involvement than pictured - meds for anaphylaxis not immediately available and nurse sent to retrieve Case - Reduction completed within few minutes of rash presentation - Rash -
Blood Cell Changes in Complement Activation- Related Pseudoallergy
Eur. J. Nanomed. 2015; 7(3): 233–244 Mini Review Zsófia Patkó* and János Szebeni Blood cell changes in complement activation- related pseudoallergy DOI 10.1515/ejnm-2015-0021 Introduction Received April 13, 2015; accepted May 19, 2015 Complement activation-related pseudoallergy (CARPA), as the name implies, is a non-Ig-E-mediated (pseudo- Abstract: The characteristic physiological changes allergic) hypersensitivity reaction (HSR) that is triggered in complement (C) activation-related pseudoallergy by C activation, or C activation plays a major contributing (CARPA) include thrombocytopenia, leukocytosis and role. CARPA is best known in the context of nanotoxicity, leukopenia with or without compensatory leukocytosis. since nanomedicines, i.e. particulate drugs and agents in In the background of these phenomena it is known that the nano (10−9–10 −6 m) size range often cause such reac- anaphylatoxins, the triggers of CARPA, can activate white tions. As reviewed earlier (1–8), and also discussed in blood cells (WBCs) and platelets, and that this activation other papers of this issue, the phenomenon represents can lead to the binding of these cells to each other and an immune barrier to the clinical use of many promising also to capillary endothelial cells, entailing microthrom- nanomedicines. In essence, CARPA may be perceived as bus formation and circulatory blockage mainly in the pul- a biological stress on blood that arises as a consequence monary and coronary microcirculation. These changes of the similarity of nanomedicines to viruses, between are key contributors to the hemodynamic alterations in which the immune system cannot make difference (8). CARPA, and can lead to anaphylactic shock. -

Penicillin Allergy Guidance Document
Penicillin Allergy Guidance Document Key Points Background Careful evaluation of antibiotic allergy and prior tolerance history is essential to providing optimal treatment The true incidence of penicillin hypersensitivity amongst patients in the United States is less than 1% Alterations in antibiotic prescribing due to reported penicillin allergy has been shown to result in higher costs, increased risk of antibiotic resistance, and worse patient outcomes Cross-reactivity between truly penicillin allergic patients and later generation cephalosporins and/or carbapenems is rare Evaluation of Penicillin Allergy Obtain a detailed history of allergic reaction Classify the type and severity of the reaction paying particular attention to any IgE-mediated reactions (e.g., anaphylaxis, hives, angioedema, etc.) (Table 1) Evaluate prior tolerance of beta-lactam antibiotics utilizing patient interview or the electronic medical record Recommendations for Challenging Penicillin Allergic Patients See Figure 1 Follow-Up Document tolerance or intolerance in the patient’s allergy history Consider referring to allergy clinic for skin testing Created July 2017 by Macey Wolfe, PharmD; John Schoen, PharmD, BCPS; Scott Bergman, PharmD, BCPS; Sara May, MD; and Trevor Van Schooneveld, MD, FACP Disclaimer: This resource is intended for non-commercial educational and quality improvement purposes. Outside entities may utilize for these purposes, but must acknowledge the source. The guidance is intended to assist practitioners in managing a clinical situation but is not mandatory. The interprofessional group of authors have made considerable efforts to ensure the information upon which they are based is accurate and up to date. Any treatments have some inherent risk. Recommendations are meant to improve quality of patient care yet should not replace clinical judgment. -

UNASYN® (Ampicillin Sodium/Sulbactam Sodium)
NDA 50-608/S-029 Page 3 UNASYN® (ampicillin sodium/sulbactam sodium) PHARMACY BULK PACKAGE NOT FOR DIRECT INFUSION To reduce the development of drug-resistant bacteria and maintain the effectiveness of UNASYN® and other antibacterial drugs, UNASYN should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria. DESCRIPTION UNASYN is an injectable antibacterial combination consisting of the semisynthetic antibiotic ampicillin sodium and the beta-lactamase inhibitor sulbactam sodium for intravenous and intramuscular administration. Ampicillin sodium is derived from the penicillin nucleus, 6-aminopenicillanic acid. Chemically, it is monosodium (2S, 5R, 6R)-6-[(R)-2-amino-2-phenylacetamido]- 3,3-dimethyl-7-oxo-4-thia-1-azabicyclo[3.2.0]heptane-2-carboxylate and has a molecular weight of 371.39. Its chemical formula is C16H18N3NaO4S. The structural formula is: COONa O CH3 N CH O 3 NH S NH2 Sulbactam sodium is a derivative of the basic penicillin nucleus. Chemically, sulbactam sodium is sodium penicillinate sulfone; sodium (2S, 5R)-3,3-dimethyl-7-oxo-4-thia 1-azabicyclo [3.2.0] heptane-2-carboxylate 4,4-dioxide. Its chemical formula is C8H10NNaO5S with a molecular weight of 255.22. The structural formula is: NDA 50-608/S-029 Page 4 COONa CH3 O N CH3 S O O UNASYN, ampicillin sodium/sulbactam sodium parenteral combination, is available as a white to off-white dry powder for reconstitution. UNASYN dry powder is freely soluble in aqueous diluents to yield pale yellow to yellow solutions containing ampicillin sodium and sulbactam sodium equivalent to 250 mg ampicillin per mL and 125 mg sulbactam per mL. -

I BOOK REVIEWS
Indian Inst. Sci. 63 (d), Mar. I983„ Pp. 4-.31 ic Indian Institute of science, Printed in India. BOOK REVIEWS The enchanted ring : The untold story of penicillin by John C. Sheehan. The Mb' press, Cambridge, Massachusetts 02142, USA, 1982, pp. xvi + 224, $ 15 (Asia $ 17.25). Despite the large number of monographs, review articles and popular literature avail. , able on penicillins and 13-lactum antibiotics, many facets of the development of the wonder drug are not known to the lay scientists. The readers of literature on penicillin gene- rally consider penicillin as a triumph of British science as the great names associated with the isolation and structure elucidation of penicillin were British stalwarts such as Alexander Fleming, Florey, Chain, Abraham Heatley and even Sir Robert Robinson. It was English crystallographer Dorothy Hodgkin who elucidated the correct structure. It is also generally accepted that the superior microbial techniques, the dynamic and innovative methodology of the American fermentation industry which made the drug available to millions at the end of the Second World War. in 1957, when John Sheehan reported the first acceptable total synthesis of penicillin he created a great sensation. The Enchanted Ring tells the story of Sheehan's involvement in the process. It is a story of indomitable faith and courage as well as superhuman perseverence which finally led to the success. The most amazing event in the history of penicillin is the confusion regarding its exact composition and structure. No other compound of a molecular weight of about 300 has baffled so many brilliant chemists. Even after the structure of penicillin was una equivocally established, Sir Robert Robinson held on. -

Cephalosporin Administration to Patients with a History of Penicillin Allergy Adverse Reactions to Drugs, Biologicals and Latex Committee
Work group report May, 2009 Cephalosporin Administration to Patients with a History of Penicillin Allergy Adverse Reactions to Drugs, Biologicals and Latex Committee Work Group Members : Roland Solensky, MD FAAAAI, Chair Aleena Banerji, MD Gordon R. Bloomberg, MD FAAAAI Marianna C. Castells, MD PhD FAAAAI Paul J. Dowling, MD George R. Green, MD FAAAAI Eric M. Macy, MD FAAAAI Myngoc T. Nguyen, MD FAAAAI Antonino G. Romano, MD PhD Fanny Silviu-Dan, MD FAAAAI Clifford M. Tepper, MD FAAAAI INTRODUCTION Penicillins and cephalosporins share a common beta-lactam ring structure, and hence the potential for IgE-mediated allergic cross-reactivity. Allergic cross-reactivity between penicillins and cephalosporins potentially may also occur due to presence of identical or similar R-group side chains, in which case IgE is directed against the side chain, rather the core beta-lactam structure. This work group report will address the administration of cephalosporins in patients with a history of penicillin allergy. First, published data will be reviewed regarding 1) cephalosporin challenges of patients with a history of penicillin allergy (without preceding skin testing or in vitro testing), and 2) cephalosporin challenges of patients proven to have a type I allergy to penicillins (via positive penicillin skin test, in vitro test or challenge). Secondly, 1 2/9/2011 recommendations on cephalosporin administration to patients with a history of penicillin allergy will be presented. Unless specifically noted, the term ‘penicillin allergy’ will be used to indicate an allergy to one or more of the penicillin-class antibiotics, not just to penicillin itself. The following discussion includes references, in certain clinical situations, to performing cephalosporin graded challenges in patients with a history of penicillin allergy. -

Cephalosporins Can Be Prescribed Safely for Penicillin-Allergic Patients ▲
JFP_0206_AE_Pichichero.Final 1/23/06 1:26 PM Page 106 APPLIED EVIDENCE New research findings that are changing clinical practice Michael E. Pichichero, MD University of Rochester Cephalosporins can be Medical Center, Rochester, NY prescribed safely for penicillin-allergic patients Practice recommendations an allergic reaction to cephalosporins, ■ The widely quoted cross-allergy risk compared with the incidence of a primary of 10% between penicillin and (and unrelated) cephalosporin allergy. cephalosporins is a myth (A). Most people produce IgG and IgM antibodies in response to exposure to ■ Cephalothin, cephalexin, cefadroxil, penicillin1 that may cross-react with and cefazolin confer an increased risk cephalosporin antigens.2 The presence of of allergic reaction among patients these antibodies does not predict allergic, with penicillin allergy (B). IgE cross-sensitivity to a cephalosporin. ■ Cefprozil, cefuroxime, cefpodoxime, Even penicillin skin testing is generally not ceftazidime, and ceftriaxone do not predictive of cephalosporin allergy.3 increase risk of an allergic reaction (B). Reliably predicting cross-reactivity ndoubtedly you have patients who A comprehensive review of the evidence say they are allergic to penicillin shows that the attributable risk of a cross- U but have difficulty recalling details reactive allergic reaction varies and is of the reactions they experienced. To be strongest when the chemical side chain of safe, we often label these patients as peni- the specific cephalosporin is similar to that cillin-allergic without further questioning of penicillin or amoxicillin. and withhold not only penicillins but Administration of cephalothin, cepha- cephalosporins due to concerns about lexin, cefadroxil, and cefazolin in penicillin- potential cross-reactivity and resultant IgE- allergic patients is associated with a mediated, type I reactions. -

5 Allergic Diseases (And Differential Diagnoses)
Chapter 5 5 Allergic Diseases (and Differential Diagnoses) 5.1 Diseases with Possible IgE Involve- tions (combination of type I and type IVb reac- ment (“Immediate-Type Allergies”) tions). Atopic eczema will be discussed in a separate section (see Sect. 5.5.3). There are many allergic diseases manifesting in The maximal manifestation of IgE-mediated different organs and on the basis of different immediate-type allergic reaction is anaphylax- pathomechanisms (see Sect. 1.3). The most is. In the development of clinical symptoms, common allergies develop via IgE antibodies different organs may be involved and symp- and manifest within minutes to hours after al- toms of well-known allergic diseases of skin lergen contact (“immediate-type reactions”). and mucous membranes [also called “shock Not infrequently, there are biphasic (dual) re- fragments” (Karl Hansen)] may occur accord- action patterns when after a strong immediate ing to the severity (see Sect. 5.1.4). reactioninthecourseof6–12harenewedhy- persensitivity reaction (late-phase reaction, LPR) occurs which is triggered by IgE, but am- 5.1.1 Allergic Rhinitis plified by recruitment of additional cells and 5.1.1.1 Introduction mediators.TheseLPRshavetobedistin- guished from classic delayed-type hypersensi- Apart from being an aesthetic organ, the nose tivity (DTH) reactions (type IV reactions) (see has several very interesting functions (Ta- Sect. 5.5). ble 5.1). It is true that people can live without What may be confusing for the inexperi- breathing through the nose, but disturbance of enced physician is familiar to the allergist: The this function can lead to disease. Here we are same symptoms of immediate-type reactions interested mostly in defense functions against are observed without immune phenomena particles and irritants (physical or chemical) (skin tests or IgE antibodies) being detectable. -

Ampicillin for Injection
AMPICILLIN - ampicillin sodium injection, powder, for solution C.O. Truxton, Inc. ---------- Ampicillin for Injection, USP For Intramuscular or Intravenous Injection To reduce the development of drug-resistant bacteria and maintain the effectiveness of Ampicillin for Injection, USP and other antibacterial drugs, Ampicillin for Injection, USP should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria. DESCRIPTION Ampicillin for Injection, USP the monosodium salt of [2S-[2α,5α,6β(S*)]]-6- [(aminophenylacetyl)amino]-3,3-dimethyl-7-oxo-4-thia-1-azabicyclo[3.2.0]heptane-2-carboxylic acid, is a synthetic penicillin. It is an antibacterial agent with a broad spectrum of bactericidal activity against both penicillin-susceptible Gram-positive organisms and many common Gram-negative pathogens. It has the following chemical structure: Ampicillin sodium is a white to off-white crystalline powder with the molecular formula of C16H18N3NaO4S, and the molecular weight of 371.39. Each vial of Ampicillin for Injection contains ampicillin sodium equivalent to 1 gram ampicillin. Ampicillin for Injection, USP contains 2.9 milliequivalents of sodium (66 mg of sodium) per 1 gram of drug. CLINICAL PHARMACOLOGY Ampicillin for Injection, USP diffuses readily into most body tissues and fluids. However, penetration into the cerebrospinal fluid and brain occurs only when the meninges are inflamed. Ampicillin is excreted largely unchanged in the urine and its excretion can be delayed by concurrent administration of probenecid. The active form appears in the bile in higher concentrations than those found in serum. Ampicillin is the least serum-bound of all the penicillins, averaging about 20% compared to approximately 60 to 90% for other penicillins. -
(Ampicillin Sodium) INJECTION, POWDER, for SOLUTION
Ampicillin for Injection, USP Rx Only PHARMACY BULK PACKAGE – NOT FOR DIRECT INFUSION To reduce the development of drug-resistant bacteria and maintain the effectiveness of ampicillin and other antibacterial drugs, ampicillin should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria. DESCRIPTION Ampicillin for injection, USP the monosodium salt of [2S-[2α,5α,6β(S*)]]-6- [(aminophenylacetyl)amino]-3,3-dimethyl-7-oxo-4-thia-1-azabicyclo[3.2.0]heptane-2-carboxylic acid, is a synthetic penicillin for intravenous use. The pharmacy bulk package contains sterile ampicillin sodium equivalent to 10 grams ampicillin. It is an antibacterial agent with a broad spectrum of bactericidal activity against both penicillin-susceptible Gram-positive organisms and many common Gram-negative pathogens. Ampicillin for injection, USP is a white to cream-tinged, crystalline powder. The solution after reconstitution is clear, colorless and free from visible particulates. Each Pharmacy Bulk Package bottle contains ampicillin sodium equivalent to 10 grams of ampicillin. The sodium content is 65.8 mg (2.9 mEq) per one gram ampicillin. A pharmacy bulk package is a container of a sterile preparation for parenteral use that contains many single doses. The contents of this pharmacy bulk package are intended for use by a pharmacy admixture service for addition to suitable parenteral fluids in the preparation of admixtures for intravenous infusion. (See DOSAGE AND ADMINISTRATION, Directions for Proper Use of Pharmacy Bulk Package). It has the following molecular structure: The molecular formula is C16H18N3NaO4S, and the molecular weight is 371.39. -

Drug Allergies & Cross-Sensitivities
DRUG ALLERGIES & CROSS-SENSITIVITIES A Presentation for HealthTrust Members June 2, 2020 Vasyl Zbyrak, PharmD, PGY-1Pharmacy Resident Saint Barnabas Medical Center Kristine A. Sobolewski, PharmD, BCPS, Preceptor 2 Speaker & Preceptor Disclosures The presenter and his preceptor have no real or perceived conflicts of interest related to this presentation. Note: This program may contain the mention of suppliers, brands, products, services or drugs presented in a case study or comparative format using evidence-based research. Such examples are intended for educational and informational purposes and should not be perceived as an endorsement of any particular supplier, brand, product, service or drug. 3 Learning Objectives Pharmacists & Nurses: Distinguish the different drug class allergies and their mechanism of action Describe the most common drug allergies and characteristics of an allergic reaction Recommend alternative treatment options based on the drug allergy profile while evaluating the potential risk for the patient 4 Learning Objectives Pharmacy Technicians Identify the characteristics of an allergic reaction and common drug allergies Recognize the names of potentially inappropriate medications based on allergies and cross-sensitivities 5 Patient Case JG is 62 YO female presenting to the ED with pain 9/10. Patient was ordered morphine 4 mg IV push. Pain was relieved, but a rash appeared on her face with some flushing. Patient is not complaining of any other symptoms or shortness of breath. 6 Is the patient experiencing a drug allergy? 7 Adverse Drug Reactions A general term utilized to encompass any unwanted reaction to a medication and are broadly divided into Type A and B reactions Type A Type B • Reactions occurring in most • Drug hypersensitivity that is patients that are common relatively uncommon, rare and predictable and mostly unpredictable • Involves potential overdose, • Involves intolerances, side effects and drug idiosyncrasy, pseudoallergy interactions and drug allergies Source: Celik G, et al. -

Social Technology and Human Health
Social technology and human health David E. Bloom1, River Path Associates2 and Karen Fang3 July 2001 1 Harvard School of Public Health. Email: [email protected] 2 Table of Contents Abstract One Lessons from the past All to gain, nothing to lose Three themes: discovery, development and distribution Understanding technology Two “Standardized packages of treatment” The forgotten plague The first battle The second battle The third battle Knowledge, health and wealth Three The problems we face A challenge refused Knowledge is not enough The failure of science Public goods and private benefits A new model Four Social Technology Crucial questions Public and private Big tech/small tech Only connect Social Technology Abstract This paper sets out to explore the relationship between technology and health. Part One of the paper uses the history of penicillin to demonstrate how the complex processes involved in getting a new technology to market are at least as important as the technology itself. Penicillin went through three stages: discovery, development and distribution – each crucial to the drug’s success. The discovery of the technology would have been useless without effective systems for both turning it into a usable package and ensuring that doctors and their patients could gain access to it. Part Two expands the idea that technology alone has little impact on health. The 20th century struggle against tuberculosis (TB) highlights the part society can play in improving its health. Knowledge of the causes of TB helped people to mobilize against the disease, with impressive results. The discovery of a vaccine reinforced society’s efforts and was instrumental in driving the disease down to vanishingly small levels, but it also led to public complacency and the latter part of the century saw TB on the rise again.