Management of the Treatment-Experienced Patient
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

HPTN 083 – Injectable Cabotegravir (CAB) for Prep
CROI 2021 Update: Evaluating Options for Long-Acting PreP 4/15/2021 Nicholas Yared, M.D. Infectious Disease Senior Staff Henry Ford Health System HPTN 083 – Injectable Cabotegravir (CAB) for PrEP • HPTN 083 showed 66% reduction in HIV incidence in men who have sex with men (MSM) and transgender women (TGW) randomized to CAB 600mg every 8 weeks vs. daily oral tenofovir disoproxil fumarate/emtricitabine (TDF/FTC) • 58 incident infections among 4566 participants • 13 in CAB group, annual incidence 0.41% • 39 in TDF/FTC group, annual incidence 1.22% • Marzinke et al. used data from HPTN 083 to characterize the 58 cases where infection occurred Marzinke M, et al. Laboratory analysis of HIV infections in HPTN 083: Injectable CAB for PrEP Lab Analysis of HPTN 083 – Methods • Plasma concentrations of CAB and TFV-diphosphate • Concentrations from dried blood spots (DBS) using liquid chromatography-tandem mass spectrometry • HIV Ag/Ab test, HIV discriminatory test, and RNA assays for HIV status and timing • Resistance testing to look for resistance-associated mutations (RAMs) if HIV-1 RNA level > 500 copies/mL Marzinke M, et al. Laboratory analysis of HIV infections in HPTN 083: Injectable CAB for PrEP Results of Lab Analysis of Incident HIV Cases in HPTN 083 – Cabotegravir Arm • 12 incident infections • 5 with no recent CAB dosing • 4 occurred despite on-time CAB injections & targeted CAB concentrations • 3 occurred in oral lead-in phase (1 had no CAB detected) • RAMs • 5 had INSTI-related mutations (Q148 or R263K) • 1 had NNRTI mutations only • 1 had NRTI & NNRTI mutations Marzinke M, et al. -

Enfermedades Infecciosas Y Microbiología Clínica Enfermedades Infecciosas Y
ISSN: 0213-005X Factor de impacto 2016: 1.714 Enfermedades Infecciosas y Microbiología Clínica Enfermedades Infecciosas y Microbiología Clínica Volumen 37, Especial Congreso 3, Diciembre 2019 Publicación mensual PUBLICACIÓN OFICIAL DE LA SOCIEDAD ESPAÑOLA DE ENFERMEDADES INFECCIOSAS Y MICROBIOLOGÍA CLÍNICA XI Congreso Nacional GeSIDA Diciembre 2019. Volumen 37. Especial Congreso 3. Páginas 1-146 y XIII Reunión Docente de la Red de Investigación de Sida (RIS) Toledo, 10-13 de diciembre de 2019 Incluida en: Index Medicus/MEDLINE Excerpta Medica/EMBASE Current Contents/Clinical Medicine ISI Alerting Services Science Citation Index-Expanded Journal Citation Reports Scopus/MEDES www.elsevier.es/eimc 00 PORTADA_GESIDA 2019.indd 1 26/11/19 14:07 PUBLICACIÓN OFICIAL DE LA SOCIEDAD ESPAÑOLA DE ENFERMEDADES INFECCIOSAS Y MICROBIOLOGÍA CLÍNICA Fundadores Editor Editores Asociados Agustí Pumarola Busquets † Benito Almirante Gragera (Barcelona) Juan Ignacio Alós Cortés (Madrid) Juan García San Miguel † José Ramón Arribas López (Madrid) Emilia Cercenado Mansilla (Madrid) Consejo Editorial Echevarria Mayo, José Manuel (Madrid) Navas Elorza, Enrique (Madrid) Aguado García, José Ma (Madrid) Ena Muñoz, Javier (Alicante) Ortiz de Lejarazu Leona, Raúl (Valladolid) Aguirrebengoa Iranguren, Koldo (Bilbao) Ezpeleta Baquedano, Ma Carmen (Bilbao) Oteo Revuelta, José Antonio (Logroño) Alarcón Cavero, Teresa (Madrid) Falguera Sacrest, Miguel (Lleida) Pachón Díaz, Jerónimo (Sevilla) Alarcón González, Arístides de (Sevilla) Fariñas Álvarez, Carmen (Santander) Pascual -

Merck & Co., Inc
As filed with the Securities and Exchange Commission on February 25, 2021 UNITED STATES SECURITIES AND EXCHANGE COMMISSION WASHINGTON, D. C. 20549 _________________________________ FORM 10-K (MARK ONE) ☒ Annual Report Pursuant to Section 13 or 15(d) of the Securities Exchange Act of 1934 For the Fiscal Year Ended December 31, 2020 OR ☐ Transition Report Pursuant to Section 13 or 15(d) of the Securities Exchange Act of 1934 For the transition period from to Commission File No. 1-6571 _________________________________ Merck & Co., Inc. 2000 Galloping Hill Road Kenilworth New Jersey 07033 (908) 740-4000 New Jersey 22-1918501 (State or other jurisdiction of incorporation) (I.R.S Employer Identification No.) Securities Registered pursuant to Section 12(b) of the Act: Title of Each Class Trading Symbol(s) Name of Each Exchange on which Registered Common Stock ($0.50 par value) MRK New York Stock Exchange 1.125% Notes due 2021 MRK/21 New York Stock Exchange 0.500% Notes due 2024 MRK 24 New York Stock Exchange 1.875% Notes due 2026 MRK/26 New York Stock Exchange 2.500% Notes due 2034 MRK/34 New York Stock Exchange 1.375% Notes due 2036 MRK 36A New York Stock Exchange Number of shares of Common Stock ($0.50 par value) outstanding as of January 31, 2021: 2,530,315,668. Aggregate market value of Common Stock ($0.50 par value) held by non-affiliates on June 30, 2020 based on closing price on June 30, 2020: $195,461,000,000. Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act. -

(51) International Patent Classification: Declarations Under Rule 4.17
) ( (51) International Patent Classification: Declarations under Rule 4.17: A61K9/00 (2006.01) A61K 31/675 (2006.01) — as to applicant's entitlement to apply for and be granted a A61K9/14 (2006.01) A61K 31/683 (2006.01) patent (Rule 4.17(H)) A61K9/16 (2006.01) — as to the applicant's entitlement to claim the priority of the (21) International Application Number: earlier application (Rule 4.17(iii)) PCT/US2020/046758 Published: (22) International Filing Date: — with international search report (Art. 21(3)) 18 August 2020 (18.08.2020) (25) Filing Language: English (26) Publication Language: English (30) Priority Data: 62/888,959 19 August 2019 (19.08.2019) US (71) Applicant: GILEAD SCIENCES, INC. [US/US]; 333 Lakeside Drive, Foster City, California 94404 (US). (72) Inventors: BANE, Jessica M.; c/o Gilead Sciences, Inc., 333 Lakeside Drive, Foster City, California 94404 (US). NEJATI, Elham; c/o Gilead Sciences, Inc., 333 Lakeside Drive, Foster City, California 94404 (US). STEFANIDIS, Dimitrios; c/o Gilead Sciences, Inc., 333 Lakeside Drive, Foster City, California 94404 (US). (74) Agent: BAJPAI, Reena et al.; Gilead Sciences, Inc., 333 Lakeside Drive, Foster City, California 94404 (US). (81) Designated States (unless otherwise indicated, for every kind of national protection available) : AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DJ, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, HR, HU, ID, IL, IN, IR, IS, IT, JO, JP, KE, KG, KH, KN, KP, KR, KW, KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, SD, SE, SG, SK, SL, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, WS, ZA, ZM, ZW. -

Long-Acting Subcutaneous Lenacapavir Dosed Every 6 Months
Long-acting Subcutaneous Lenacapavir Dosed Every 6 Months as part of a Combination Regimen in Treatment-Naïve People with HIV: Interim 16-week Results of a Randomized, Open-label, Phase 2 Induction-Maintenance Study (CALIBRATE) Samir K. Gupta,1 Mezgebe Berhe,2 Gordon Crofoot,3 James Sims,4 Paul Benson,5 Moti Ramgopal,6 William E. Sanchez,7 Peter Ruane,8 Cheryl McDonald,9 Anita Scribner,10 Hui Wang,11 Laurie VanderVeen,11 Hadas Dvory-Sobol,11 Robert H. Hyland,11 Martin S. Rhee,11 Jared M. Baeten,11 Diana M. Brainard,11 Ellen Koenig12 1Indiana University School of Medicine, Indianapolis, USA; 2North Texas Infectious Diseases Consultants, Dallas, USA; 3The Crofoot Research Center, Inc., Houston, USA; 4St. Hope Foundation, Bellaire, USA; 5Be Well Medical Center, Berkley, USA; 6Midway Specialty Care Center, Fort Pierce, USA; 7Floridian Clinical Research, Hialeah, USA; 8Ruane Clinical Research Group, Los Angeles, USA; 9Texas Centers for Infectious Disease Associates, Fort Worth, USA; 10Diagnostic Clinic of Longview Center for Clinical Research, Longview, USA; 11Gilead Sciences Inc., Foster City, USA; 12Instituto Dominicano de Estudios Virológicos, Santo Domingo, Dominican Republic Disclosures SKG receives unrestricted research grant support from the NIH, Indiana University School of Medicine, and GSK/ViiV and receives advisory board fees from Gilead Sciences, Inc., and GSK/ViiV. 2 Acknowledgments We extend our thanks to: The study participants and their families Participating study investigators and staff: Dominican Republic: E Koenig United States: P Benson; DS Berger; M Berhe; C Brinson; P Cook; DR Coulston; GE Crofoot; FA Cruickshank; D Cunningham; E DeJesus; C Dietz; V Drelichman; E Gardner; A Gaur; D Goldstein; SK Gupta; D Hagins; R Hengel; T Hodge; C-B Hsiao; A Khalsa; CA Kinder; P Kumar; C McDonald; A Mills; JO Morales-Ramirez; C Newman; G Oguchi; O Osiyemi; MN Ramgopal; PJ Ruane; W Sanchez; JL Santana-Bagur; L Santiago; A Scribner; J Sims; GI Sinclair; JL Stephens; M Wohlfeiler; AK Wurapa This study was funded by Gilead Sciences, Inc. -

What's New in Hiv? Highlights & New Data on Hiv Treatment a Presentation for Healthtrust Members June 18, 2021
WHAT'S NEW IN HIV? HIGHLIGHTS & NEW DATA ON HIV TREATMENT A PRESENTATION FOR HEALTHTRUST MEMBERS JUNE 18, 2021 SHIVANI PATEL, PHARMD PGY-1 PHARMACY RESIDENT ROBERT WOOD JOHNSON UNIVERSITY HOSPITAL NAVANEETH NARAYANAN, PHARMD, MPH, BCIDP CLINICAL ASSOCIATE PROFESSOR RUTGERS UNIVERSITY ERNEST MARIO SCHOOL OF PHARMACY CONFLICT OF INTEREST DISCLOSURE There are no relevant financial interest to disclose for myself or my spouse/partner within the last 12 months. The preceptor has a financial interest/arrangement, affiliation or relationship with Astellas and Merck that could be perceived as a real or apparent conflict of interest in the context of the subject of this activity. Note: This program may contain the mention of suppliers, brand products, services, or drugs presented in a case study or comparative format using evidence-based research. Such examples are intended for educational and informational purposes only and should not be perceived as an endorsement of any particular supplier, brand, product, service or drug. 1 2 3 LEARNING Identify new antiretroviral Describe a two-drug regimen Outline key counseling points agents and their role in the for treatment-naïve to a patient receiving new OBJECTIVES management of HIV/AIDS individuals and factors to antiretroviral agents related consider when selecting an to drug administration, initial regimen for an potential side effects, and individual. drug-drug interactions DRUG NAME ABBREVIATIONS Abbreviation Full Name Abbreviation Full Name Abbreviation Full Name 3TC Lamivudine DTG Dolutegravir -
To View the CAHR 2020 Abstract Book
29th Annual Canadian 29e Congrès annuel Conference on canadien de recherche HIV/AIDS Research sur le VIH/sida Hope, Victories and Perseverance beyond 2020 Hope, Victoires et Persévérance au-delà de 2020 ABSTRACTS ABRÉGÉS www.cahr-acrv.ca CAHR 2020 VIRTUAL CAHR 2020 Hope, Victories and Perseverance beyond 2020 ACRV 2020 Espoir, Victoires et Persévérance au-delà de 2020 Abstracts / Abrégés May 1 - 2, 2020 / 1 au 2 mai 2020 Virtual Conference Due to COVID-19, the 29th Annual Canadian Conference on HIV/AIDS Research -- which was scheduled to take place in Quebec City -- became CAHR 2020 Virtual. This compendium of abstracts represents those that were approved for the face to face program as developed by the 2020 Conference Scientific Committee. The 29th Annual Canadian Conference on HIV/AIDS Research April 2020 29e Congrès annuel canadien de recherche sur le VIH/sida avril 2020 CAHR Committees / Comités de l’ACRV CAHR Executive Committee / Conseil de direction de l’ACRV President / Président Dr. Carol Strike President Elect / Président désigné Dr. Keith Fowke Past President / Ancien président Dr. Curtis Cooper Treasurer / Trésorière Dr. Marissa Becker Secretary / Secrétaire Dr. Shariq Haider CAHR Board of Directors / Conseil d’administration de l’ACRV Track A: Basic Sciences / Volet A : Sciences fondamentales Dr. Lyle McKinnon Track B: Clinical Sciences / Volet B : Sciences cliniques Dr. Alexandra King Track C: Epidemiology and Public Health Sciences / Volet C : Épidémiologie et sciences de la santé publique Dr. Angela Kaida Track D: Social Sciences / Volet D : Sciences sociales Dr. Ciann Wilson Community Representative / Représentant communautaire Kerrigan Johnson CAHR Staff Members / Personnel de l’ACRV Executive Director / Directeur général Andrew Matejcic Sponsorship, Accreditation, Education Erin Love Gestionnaire, Commandites, agrément et formation Finance, Communications Shelley Mineault Gestionnaire Finances et communications Scientific Program Committee / Comité du programme scientifique Conference Co-Chairs / Coprésidents du congrès Dr. -
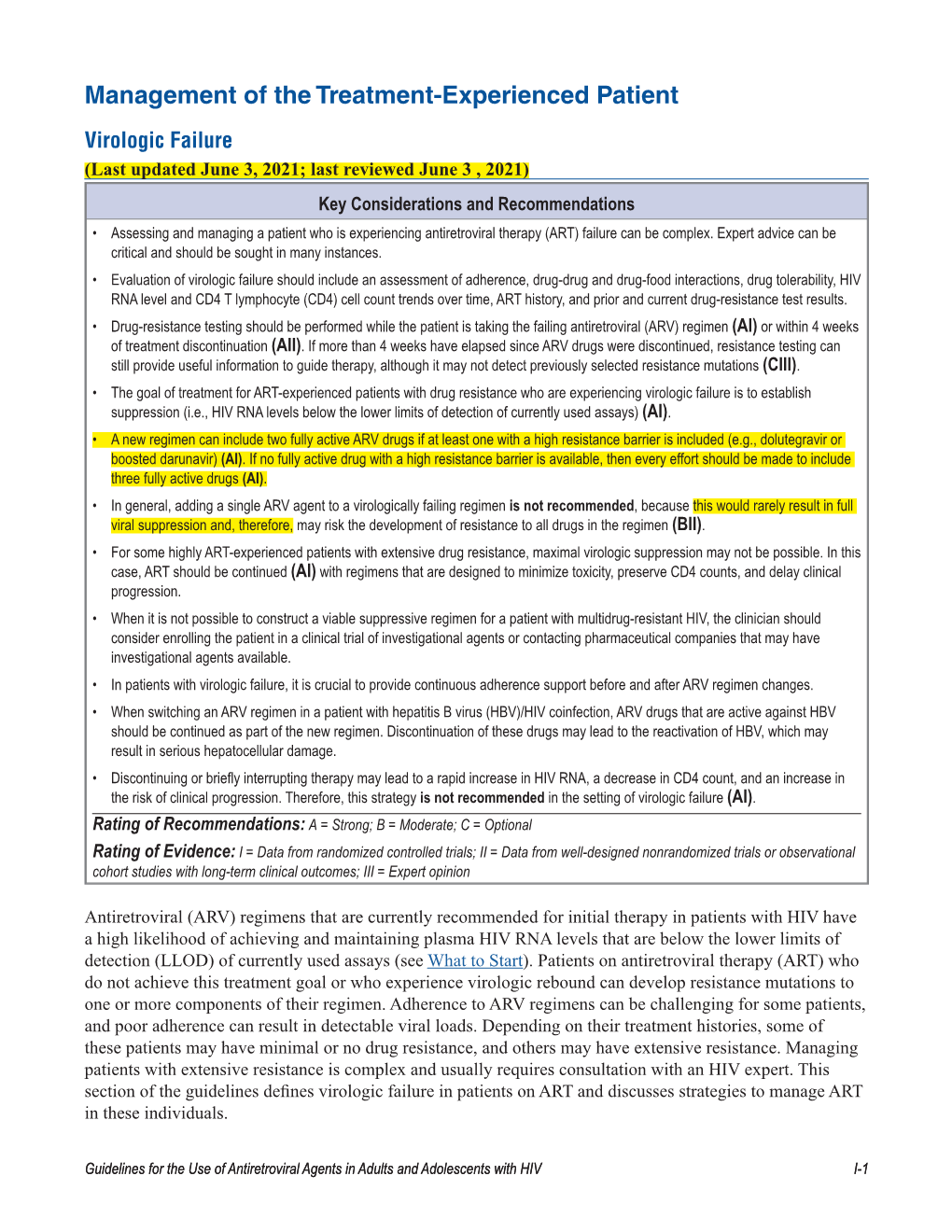
Guidelines for the Use of Antiretroviral Agents in Adults and Adolescent Living With
Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents with HIV Developed by the DHHS Panel on Antiretroviral Guidelines for Adults and Adolescents – A Working Group of the Office of AIDS Research Advisory Council (OARAC) How to Cite the Adult and Adolescent Guidelines: Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents with HIV. Department of Health and Human Services. Available at https://clinicalinfo.hiv.gov/sites/default/files/guidelines/documents/ AdultandAdolescentGL.pdf. Accessed [insert date] [insert page number, table number, etc. if applicable] It is emphasized that concepts relevant to HIV management evolve rapidly. The Panel has a mechanism to update recommendations on a regular basis, and the most recent information is available on the HIVinfo Web site (http://hivinfo.nih.gov). What’s New in the Guidelines? August 16, 2021 Hepatitis C Virus/HIV Coinfection • Table 18 of this section has been updated to include recommendations regarding concomitant use of fostemsavir or long acting cabotegravir plus rilpivirine with different hepatitis C treatment regimens. June 3, 2021 What to Start • Since the release of the last guidelines, updated data from the Botswana Tsepamo study have shown that the prevalence of neural tube defects (NTD) associated with dolutegravir (DTG) use during conception is much lower than previously reported. Based on these new data, the Panel now recommends that a DTG-based regimen can be prescribed for most people with HIV who are of childbearing potential. Before initiating a DTG-based regimen, clinicians should discuss the risks and benefits of using DTG with persons of childbearing potential, to allow them to make an informed decision. -

Prep and Microbicides PIPELINE REPORT 2021
Pipeline Report » 2021 PrEP and Microbicides PIPELINE REPORT 2021 The PrEP and Microbicides Pipeline By Richard Jefferys The scientific development of medical interventions can sometimes become fixated on potential one-size-fits-all “home run” solutions. In the realm of biomedical HIV prevention research, community advocates have helped push back against this model, emphasizing the critical importance of creating an array of effective options that people can choose based on their individual situation. The PrEP and microbicide pipelines reflect the pursuit of diverse approaches, including oral, injectable, and topical candidates. Despite the COVID-19 pandemic, 2020 was a year of exceptional progress in HIV prevention research. The most significant news in microbicide development is that, in July 2020, the dapivirine vaginal ring received a positive opinion from the European Medicines Agency (EMA) for use by cisgender women aged 18 and over in high-burden developing countries “when oral pre-exposure prophylaxis (PrEP) is not used, cannot be used or is not available.” This was followed by the addition of the dapivirine vaginal ring to the World Health Organization (WHO) list of prequalified medicines, and in January 2021, the WHO issued a recommendation for the ring as “a new choice for HIV prevention for women at substantial risk of HIV infection.” The International Partnership for Microbicides (IPM) is now seeking regulatory approval for the ring in Kenya, Malawi, Rwanda, South Africa, Tanzania, Uganda, Zambia, and Zimbabwe. For Eswatini and Lesotho, IPM is taking steps to make the ring available under national import license processes. An application to the U.S. Food and Drug Administration (FDA) was submitted in December 2020. -
Croi 2021 Program Committee
General Information CONTENTS WELCOME . 2 General Information General Information OVERVIEW . 2 CONTINUING MEDICAL EDUCATION . 3 CONFERENCE SUPPORT . 4 VIRTUAL PLATFORM . 5 ON-DEMAND CONTENT AND WEBCASTS . 5 CONFERENCE SCHEDULE AT A GLANCE . 6 PRECONFERENCE SESSIONS . 9 LIVE PLENARY, ORAL, AND INTERACTIVE SESSIONS, AND ON-DEMAND SYMPOSIA BY DAY . 11 SCIENCE SPOTLIGHTS™ . 47 SCIENCE SPOTLIGHT™ SESSIONS BY CATEGORY . 109 CROI FOUNDATION . 112 IAS–USA . 112 CROI 2021 PROGRAM COMMITTEE . 113 Scientific Program Committee . 113 Community Liaison Subcommittee . 113 Former Members . 113 EXTERNAL REVIEWERS . .114 SCHOLARSHIP AWARDEES . 114 AFFILIATED OR PROXIMATE ACTIVITIES . 114 EMBARGO POLICIES AND SOCIAL MEDIA . 115 CONFERENCE ETIQUETTE . 115 ABSTRACT PROCESS Scientific Categories . 116 Abstract Content . 117 Presenter Responsibilities . 117 Abstract Review Process . 117 Statistics for Abstracts . 117 Abstracts Related to SARS-CoV-2 and Special Study Populations . 117. INDEX OF SPECIAL STUDY POPULATIONS . 118 INDEX OF PRESENTING AUTHORS . .122 . Version 9 .0 | Last Update on March 8, 2021 Printed in the United States of America . © Copyright 2021 CROI Foundation/IAS–USA . All rights reserved . ISBN #978-1-7320053-4-1 vCROI 2021 1 General Information WELCOME TO vCROI 2021 Welcome to vCROI 2021! The COVID-19 pandemic has changed the world for all of us in so many ways . Over the past year, we have had to put some of our HIV research on hold, learned to do our research in different ways using different tools, to communicate with each other in virtual formats, and to apply the many lessons in HIV research, care, and community advocacy to addressing the COVID-19 pandemic . Scientists and community stakeholders who have long been engaged in the endeavor to end the epidemic of HIV have pivoted to support and inform the unprecedented progress made in battle against SARS-CoV-2 . -

Merck Announces Week 96 Data from Phase 2B Study Evaluating Islatravir in Combination with Doravirine in Adults with HIV-1 Infection
NEWS RELEASE Merck Announces Week 96 Data from Phase 2b Study Evaluating Islatravir in Combination With Doravirine in Adults With HIV-1 Infection 10/8/2020 Treatment With Islatravir and Doravirine Maintained Viral Suppression and No Viral Resistance was Identied Company Also Presenting Phase 1/1b Results for MK-8507, a New Investigational Once- Weekly Oral HIV Agent; Company Advances MK-8507 to Phase 2 KENILWORTH, N.J.--(BUSINESS WIRE)-- Merck (NYSE: MRK), known as MSD outside the United States and Canada, today announced Week 96 data from the Phase 2b trial (NCT03272347) evaluating the ecacy and safety of islatravir, the company’s investigational oral nucleoside reverse transcriptase translocation inhibitor (NRTTI), in combination with doravirine (PIFELTRO™), in treatment-naïve adults with HIV-1 infection. Week 96 ndings demonstrated that the combination of islatravir and doravirine maintained virologic suppression (as measured by the number of study participants achieving HIV-1 RNA levels <50 copies/mL, similar to DELSTRIGO™(doravirine/lamivudine/tenofovir disoproxil fumarate)), and the ndings were consistent with Week 48 results. Additional Week 96 data from the study show low rates of participants meeting the denition of protocol- dened virologic failure (PDVF) in both the islatravir plus doravirine and the DELSTRIGO treatment arms, and no participants in either arm met the criteria for resistance testing. Merck also announced results from Phase 1/1b studies for MK-8507, the company’s investigational once-weekly oral non-nucleoside reverse transcriptase inhibitor (NNRTI), which showed that the antiviral potency and pharmacokinetics of MK-8507 support further investigation for once-weekly oral administration as part of combination antiretroviral therapy. -

Interactions of HIV-1 Capsid with Host Factors and Their Implications for Developing Novel Therapeutics
viruses Review Interactions of HIV-1 Capsid with Host Factors and Their Implications for Developing Novel Therapeutics Shentian Zhuang 1,2 and Bruce E. Torbett 1,2,3,* 1 Department of Immunology and Microbiology, The Scripps Research Institute, La Jolla, CA 92037, USA; [email protected] 2 Center for Immunity and Immunotherapies, Seattle Children’s Research Institute, Seattle, WA 98101, USA 3 Department of Pediatrics, University of Washington School of Medicine, Seattle, WA 98105, USA * Correspondence: [email protected] Abstract: The Human Immunodeficiency Virus type 1 (HIV-1) virion contains a conical shell, termed capsid, encasing the viral RNA genome. After cellular entry of the virion, the capsid is released and ensures the protection and delivery of the HIV-1 genome to the host nucleus for integration. The capsid relies on many virus–host factor interactions which are regulated spatiotemporally throughout the course of infection. In this paper, we will review the current understanding of the highly dynamic HIV-1 capsid–host interplay during the early stages of viral replication, namely intracellular capsid trafficking after viral fusion, nuclear import, uncoating, and integration of the viral genome into host chromatin. Conventional anti-retroviral therapies primarily target HIV-1 enzymes. Insights of capsid structure have resulted in a first-in-class, long-acting capsid-targeting inhibitor, GS-6207 (Lenacapavir). This inhibitor binds at the interface between capsid protein subunits, a site known to bind host factors, interferes with capsid nuclear import, HIV particle assembly, and ordered assembly. Our review will highlight capsid structure, the host factors that interact with capsid, and high- throughput screening techniques, specifically genomic and proteomic approaches, that have been Citation: Zhuang, S.; Torbett, B.E.