1 INTRODUCTION to HISTOPATHOLOGY Paul C
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Candidate Handbook
American College of Veterinary Pathologists Certifying Examination Candidate Handbook Updated January 16, 2018 Table of Contents INTRODUCTION ............................................................................................................................. 3 CONTACT INFORMATION ............................................................................................................ 3 CERTIFYING EXAMINATION ..................................................................................................... 3 PHASE I EXAMINATION ................................................................................................................ 4 ADMINISTRATION OF THE PH ASE I EXAMINATION ........................................................................ 4 PHASE II EXAMINATION .............................................................................................................. 5 ADMINISTRATION OF THE PH ASE II EXAMINATION ....................................................................... 5 ANATO MIC PATHOLOG Y RESOURCES: .............................................................................................. 5 CLIN IC AL PATHOLOG Y RESOURCES: ................................................................................................ 6 SPONSOR AND TRAINING ROUTE REQUIREMENTS AND DEFINITIONS ............... 6 ELIGIBILITY .................................................................................................................................... 8 CREDENTIALING REQUIREMENTS FOR ALL EXAMINATIONS -
Chapter 15 VETERINARY PATHOLOGY
Veterinary Pathology Chapter 15 VETERINARY PATHOLOGY ERIC DESOMBRE LOMBARDINI, VMD, MSc, DACVPM, DACVP*; SHANNON HAROLD LACY, DVM, DACVPM, DACVP†; TODD MICHAEL BELL, DVM, DACVP‡; JENNIFER LYNN CHAPMAN, DVM, DACVP§; DARRON A. ALVES, DVM, DACVP¥; and JAMES SCOTT ESTEP, DVM, DACVP¶ INTRODUCTION DIAGNOSTICS BIODEFENSE AND BIOMEDICAL RESEARCH CHEMICAL DEFENSE RADIATION DEFENSE COMBAT CASUALTY CARE FIELD OPERATIONS SUMMARY *Lieutenant Colonel, Veterinary Corps, US Army, Chief, Divisions of Comparative Pathology and Veterinary Medical Research, Armed Forces Research Institute of Medical Sciences, 315/6 Rajavithi Road, Bangkok 10400, Thailand †Major (P), Veterinary Corps, US Army, Chief, Education Operations, Joint Pathology Center, 2460 Linden Lane, Building 161, Room 102, Silver Spring, Maryland 20910 ‡Major (P), Veterinary Corps, US Army, Biodefense Research Pathologist, US Army Medical Research Institute of Infectious Diseases, 1425 Porter Street, Room 901B, Frederick, Maryland 21702 §Lieutenant Colonel, Veterinary Corps, US Army, Director, Overseas Operations, Walter Reed Army Institute of Research, 503 Robert Grant Avenue, Room 1W43, Silver Spring, Maryland 20910 ¥Lieutenant Colonel, Veterinary Corps, US Army, Chief, Operations, US Army Office of the Surgeon General, 7700 Arlington Boulevard, Arlington, Virginia 22042 ¶Lieutenant Colonel, Veterinary Corps, US Army (Retired); formerly, Chief of Comparative Pathology, Triservice Research Laboratory, US Army Institute of Surgical Research, 1210 Stanley Road, Joint Base San Antonio-Fort Sam -

Veterinary Pathobiology (V PBIO) 1
Veterinary Pathobiology (V_PBIO) 1 focus of lectures will be on the biology and epidemiology of parasitic Veterinary Pathobiology diseases and on the parasite-host association. Graded on A-F basis only. Credit Hours: 3 (V_PBIO) Prerequisites: BIO_SC 1030 or BIO_SC 1500 or consent of instructor V_PBIO 1500: The Microbial World V_PBIO 3345W: Fundamentals of Parasitology - Writing Intensive This is a course for students who are not science majors. It is designed This course will provide a basic understanding of protozoan and to acquaint students with some microbial activities which affect their metazoan parasites as well as the vectors that transmit these parasites. lives. It includes the historical development of microbiology, structures Special emphasis will be placed on those parasites and vectors of major of bacteria, viruses, and fungi, the basic principles of microbial growth, medical/veterinary consequence throughout the world. Because parasites disinfection and sterilization, antibiotics and antibiotic resistance, cause significant morbidity and mortality throughout the world, the main infection, and immunity, probiotics and microbiomes, public health, and focus of lectures will be on the biology and epidemiology of parasitic commercial, agricultural, and industrial uses of microorganisms. The diseases and on the parasite-host association. Graded on A-F basis only. lab covers basics of microscopy, culture and identification of bacteria, microbial ecology, and antibiotic resistance. Not open to students with Credit Hours: 3 any credit in microbiology. Prerequisites: BIO_SC 1030 or BIO_SC 1500 or consent of instructor Credit Hours: 5 Recommended: High School biology V_PBIO 3500: Issues in Vector-borne and Emerging Infectious Diseases This writing intensive course will focus on vector-borne and emerging V_PBIO 2001: Fundamentals of Microbiology infectious diseases, with an emphasis on recent infectious diseases in This course, which is designed for microbiology or life sciences majors, the news and current issues related to this subject area. -

Cerebellar Disease in the Dog and Cat
CEREBELLAR DISEASE IN THE DOG AND CAT: A LITERATURE REVIEW AND CLINICAL CASE STUDY (1996-1998) b y Diane Dali-An Lu BVetMed A thesis submitted for the degree of Master of Veterinary Medicine (M.V.M.) In the Faculty of Veterinary Medicine University of Glasgow Department of Veterinary Clinical Studies Division of Small Animal Clinical Studies University of Glasgow Veterinary School A p ril 1 9 9 9 © Diane Dali-An Lu 1999 ProQuest Number: 13815577 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a com plete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. uest ProQuest 13815577 Published by ProQuest LLC(2018). Copyright of the Dissertation is held by the Author. All rights reserved. This work is protected against unauthorized copying under Title 17, United States C ode Microform Edition © ProQuest LLC. ProQuest LLC. 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, Ml 48106- 1346 GLASGOW UNIVERSITY lib ra ry ll5X C C ^ Summary SUMMARY________________________________ The aim of this thesis is to detail the history, clinical findings, ancillary investigations and, in some cases, pathological findings in 25 cases of cerebellar disease in dogs and cats which were presented to Glasgow University Veterinary School and Hospital during the period October 1996 to June 1998. Clinical findings were usually characteristic, although the signs could range from mild tremor and ataxia to severe generalised ataxia causing frequent falling over and difficulty in locomotion. -

Veterinary Pathology
Children’s Resources: Veterinary Pathology Veterinary Specialty of the Day: Pathology Some veterinarians and veterinary technicians undergo further training to specialize in a specific field of medicine. Veterinarians who specialize in Pathology are trained to perform diagnostic tests. These tests help the pathologist determine a disease or monitor a condition that a patient has. Anatomic pathologists diagnose diseases by examining and testing body tissue samples. Clinical pathologists diagnose diseases by analyzing laboratory tests, typically of bodily fluids. Discussion Question • Why might veterinarians need to collect samples (such as blood, urine, or body tissue) from their patients? Veterinary pathologists are trained to analyze... Biopsies Necropsies Bodily Fluids & Cells A biopsy is when a piece of If an animal dies due to Veterinary pathologists can body tissue is removed. The unknown circumstances, run tests on bodily fluids, tissue is then examined and trained pathologists can such as urine or blood. They analyzed in a laboratory. perform a surgical exam can also test and examine called a necropsy to figure cells, which are the building out the cause of death. In blocks that make up all of human medicine, this is our body's organs. called an "autopsy". 1 Children’s Resources: Veterinary Pathology Types of Diagnostic Tests Veterinary pathologists perform diagnostic tests to determine a disease or monitor a condition that a patient has. Below are examples of different types of diagnostic tests that can be performed in a laboratory. Veterinary pathologists perform many, but not all, of the tests listed below. Clinical Chemistry Cytology Clinical chemistry is used to Cytology is the study of cells. -

Elements of Good Training in Anatomic Pathology L
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Digital Repository @ Iowa State University Veterinary Pathology Publications and Papers Veterinary Pathology 9-2010 Elements of Good Training in Anatomic Pathology L. Munson University of California L. E. Craig University of Tennessee M. A. Miller Purdue University N. D. Kock Wake Forest University R. M. Simpson National Cancer Institute See next page for additional authors Follow this and additional works at: http://lib.dr.iastate.edu/vpath_pubs Part of the Veterinary Anatomy Commons, and the Veterinary Pathology and Pathobiology Commons The ompc lete bibliographic information for this item can be found at http://lib.dr.iastate.edu/ vpath_pubs/72. For information on how to cite this item, please visit http://lib.dr.iastate.edu/ howtocite.html. This Article is brought to you for free and open access by the Veterinary Pathology at Iowa State University Digital Repository. It has been accepted for inclusion in Veterinary Pathology Publications and Papers by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. Elements of Good Training in Anatomic Pathology Abstract The American College of Veterinary Pathologists’ (ACVP’s) 2007–2012 strategic plan recognized the crisis confronting academic training programs and formed a task force to address these concerns. One area of concern identified by the ACVP Training Program Development Task Force was the lack of guidelines to make training more consistent across all programs and provide justification for maintaining or increasing faculty numbers and training resources. Training guidelines for clinical pathology have been outlined in three publications.1,2,4 The current document addresses the need for training guidelines in veterinary anatomic pathology. -

Arnold Theiler and Colleagues: a Successful Cooperation Between Switzerland and South Africa1
Originalarbeiten | Original contributions Arnold Theiler and colleagues: a successful cooperation between Switzerland and South Africa1 A. Pospischil2 2Institut für Veterinärpathologie, Universität Zürich, Swiss Association of the History of Veterinary Medicine Arnold Theiler und Kollegen: eine Summary https://doi.org/ erfolgreiche Zusammenarbeit 10.17236/sat00286 zwischen der Schweiz und Südafrika The start of the Swiss-South African connection and Eingereicht: 21.06.2020 cooperation dates back to the late 19th century, when a Angenommen: 02.08.2020 Der Beginn der schweizerisch-südafrikanischen Bezie- shortage of veterinarians in Transvaal (South African 1 Extended version of hung und Zusammenarbeit geht auf das späte 19. Jahr- Republic, ZAR) motivated Arnold Theiler to seek his a presentation given at hundert zurück, als in Transvaal (Südafrikanische Re- chance there. He became successful and famous fighting the 44th International Congress of the World publik, ZAR) ein Mangel an Tierärzten, Arnold Theiler a smallpox epidemic and rinderpest after a difficult start Association for the His motivierte, dort seine Chance zu suchen. Nach einem as practicing veterinarian. Prior to the establishment of tory of Veterinary Medici ne in South Africa 2020 schwierigen Start als praktizierender Tierarzt wurde er the «Veterinary Bacteriological Laboratories of the durch seinen Kampf gegen eine Pocken- und Rinderpes- Transvaal» in 1908 Theiler as the head of the institution tepidemie erfolgreich und berühmt. Vor der Gründung could motivate some Swiss veterinarians to come and der «Veterinary Bacteriological Laboratories of the work with him. The opening of the new laboratory made Transvaal» im Jahr 1908 konnte Theiler als Leiter der e. g. Walter Frei, later professor for veterinary pathology Einrichtung einige Schweizer Tierärzte motivieren, mit at Zurich and Karl Friedrich Meyer, becoming an emi- ihm zusammenzuarbeiten. -

COME in PAIRS VETERINARY Veterinary
E Q SOMETIMES MIRACLES... UINE equine American Edition | February 2020 COME IN PAIRS VETERINARY veterinary EDUCATION/American education Edition Volume 32 Number 2 AND TOGETHER, ASSURE GUARD GOLD-NG AND ASSURE GUARD GOLD CREATE A POWERHOUSE AGAINST YOUR MOST CHALLENGING DIGESTIVE CASES. in this issue: February USE ASSURE GUARD GOLD-NG FOR FAST RELIEF AND MAINTAIN EXCELLENT DIGESTIVE Beyond good intentions: The ethics of ‘spotting’ medications to colleagues The official journal of the HEALTH WITH ASSURE GUARD GOLD. American Association of Theiler’s disease associated with administration of tetanus antitoxin contaminated 2020 Equine Practitioners, produced with nonprimate (equine) hepacivirus and equine parvovirus-hepatitis virus Ask your Arenus Veterinary Solution Specialist how Assure Guard Gold-NG in partnership with BEVA. and Assure Guard Gold can help your equine patients quickly and Treatment of haemoperitoneum secondary to ruptured granulosa cell effectivley recover from the digestive upsets you treat daily. tumours in two mares Arenus Animal Health | 866-791-3344 | www.arenus.com equine veterinary education American Edition FEBRUARY 2020 • Volume 32 • N umbER 2 AAEP NEWS In this issue contents Beyond good intentions: The ethics of ‘spotting’ medications to colleagues.. III Glanders Guidelines released on AAEP website, publications app..................... V Resolving conflict in a healthy way...........................................................................VIII Highlights of Recent Clinically Relevant Papers S. WRIGHT..............................................................................................................................58 -

Veterinary Pathology: Instructions to Authors
Veterinary Pathology: Instructions to Authors Table of Contents Submission and Evaluation of Manuscripts ................................................................................ 3 Editorial Policies ........................................................................................................................ 4 Scope and Criteria for Acceptance .......................................................................................................4 Authorship .........................................................................................................................................5 Research Ethics, Ethical Treatment of Animals, and Consent of Animal Owners ....................................5 Availability of supporting research data ..............................................................................................5 Duplicate or Related Publication, and Plagiarism .................................................................................6 Publication of Reprinted Material .......................................................................................................6 Conflict of Interest Policy: Authors ......................................................................................................6 Conflict of Interest Policy: Reviewers ..................................................................................................7 Exclusive License to Publish ................................................................................................................7 -

Sri Venkateswara Veterinary University, Tirupati
Volume - 15 Issue - 8 Jan-March, 2019 SRI VENKATESWARA VETERINARY UNIVERSITY, TIRUPATI Visit us at : svvu.edu.in From the Desk of Hon'ble Vice-Chancellor TIME TO RE-ORIENT OUR APPROACH Patron It gives me immense pleasure to announce that SVVU got two Dr. Y. Hari Babu mega projects of International collaboration coordinated by Royal Vice-Chancellor Veterinary College at London and the Scientific Research of Veterinary Republic of Tunisia. Chief Editor During this quarter, University has focused on the capacity building programmes for field Veterinarians, shepherds and dairy Dr. D. Sreenivasulu farmers, organization of kisan mela and breeding ram distribution Director of Extension at LRS, Palamaner, organization of special NSS camps, inaugurations of Diamond Jubilee pylon (1955- 2015), new boys hostel at CVSc, Advisors Tirupati and 10th sports, games, cultural and literary meet at CFSc., Dr. D. Srinivasa Rao Muthukur and a national conference organized by Dept. of Registrar Veterinary Parasitology of CVSc, Tirupati. The Principal Secretary, AHDD & Fishery, AP visited the campus Dr. T.S. Chandrasekhara Rao Dean, Faculty of Veterinary and reviewed the activities of University. The then Hon’ble Chief Science Minister of Andhra Pradesh, inaugurated the new spacious Veterinary Clinical Complex building with the state of art Dr. V. Padmanabha Reddy equipments to cater the needs of animal owners. The activities of Dean, Faculty of Dairy Science KVK, Lam, Guntur were remarkably appreciated by the farmers. The Dr. Y. Hari Babu, Vice-Chancellor work progress on conservation of Ongole and Punganur was Sri Venkateswara Veterinary University, Tirupati. Dr. T.V. Ramana Dean, Faculty of Fishery Science appreciated by the Principal Secretary. -

…From the President Winter Is Waning and Spring Is Near! for Theriogenology, Spring Is Always a Busy Time, No Matter What Your Favorite Species
THE OFFICIAL PUBLICATION OF THE SOCIETY FOR THERIOGENOLOGY …from the president Winter is waning and Spring is near! For Theriogenology, Spring is always a busy time, no matter what your favorite species. our Executive Board just returned from a very busy DR. DWIGHT WOLFE Winter Board meeting in Charleston, SC, and we are Yexcited about the future for the SFT. We welcome new SFT board members Dr. Tamara Dobbie, equine practitioner from New York, Dr. Scott Pretzer, small animal practitioner from Kansas, and Dr. Richard Hopper, Assistant NANDI, SACRED BULL AND SYMBOL OF FRUITFULNESS news Professor at Mississippi State University, to their first SFT Executive Board meeting. Vol. 28, No. 1 Dr. Walter Zent and his program committee have an excellent Annual Conference WINTER 2005 planned for our August meeting. The 2005 Annual Conference is rapidly approach- ing. The Francis Marion Hotel, located in the historic district of scenic Charleston, From the President . .1 S.C., provides an outstanding venue for our next conference. Make your hotel Make Plans for Charleston . .2 reservations now so not to miss this excellent CE opportunity. Charleston is a charming city that everyone will enjoy. Thanks to the generosity of Pfizer, Inc. Charleston Attractions . .3 Family Night will be at the Charleston Aquarium, a fabulous facility boasting one of the largest tanks in the United States. The evening proves to be a fun and enter- Annual Conference & Symposia Schedule . .4 taining evening for everyone to relax and visit with old friends and new. SFT Selects Publishing Partner . .6 The SFT Executive Board approved 2 important new initiatives for our organization. -
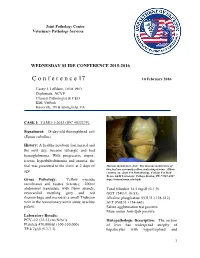
C O N F E R E N C E 17 10 February 2016
Joint Pathology Center Veterinary Pathology Services WEDNESDAY SLIDE CONFERENCE 2015-2016 C o n f e r e n c e 17 10 February 2016 Casey J. LeBlanc, DVM, PhD Diplomate, ACVP Clinical Pathologist & CEO KDL VetPath Knoxville, TN & Springfield, VA CASE I: TAMU-1-2013 (JPC 4033379). Signalment: 18-day-old thoroughbred colt (Equus caballus) History: A healthy newborn foal nursed and the next day, became lethargic and had hemoglobinuria. With progressive stupor, icterus, hyperbilirubinemia and anemia, the foal was presented to the clinic at 2 days of Mucous membranes, foal. The mucous membranes of this foal are extremely yellow, indicating icterus. (Photo age. courtesy of: Dept Vet Pathobiology, College Vet Med Texas A&M University, College Station, TX 77843-4467 Gross Pathology: Yellow mucous http://vetmed.tamu.edu/vtpb) membranes and tissues (icterus); ~200ml abdominal transudate with fibrin strands; Total bilirubin 14.5 mg/dl (0-1.9) myocardial mottling grey and red GGT 124U/L (0-53) (hemorrhage and necrosis) a small Thebsian Alkaline phosphatase 553U/L (128-512) vein in the noncoronary aortic sinus; urachus ALT 850U/L (134-643) patent. Saline agglutination test positive Mare serum Anti-Qab positive Laboratory Results: PCV=12 (32-53) no Nrbc’s Histopathologic Description: The section Platelets 470,000/ul (100-350,000) of liver has widespread atrophy of TP 4.7g/dl (5.3-7.3) hepatocytes with hypertrophied and 1 Liver, foal. There is extensive pigment deposition throughout the section, to include brown granules in hepatocytes (lipofuscin- yellow arrows), brown spicular material (acid hematin – green arrows) and distended bile canaliculi (cholestasis – black arrows).