Unc-Health-Proposal.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
We're Racing Ahead
We’re racing ahead to solve complex and compelling 21st-century public health problems SPRING 2011 VOLUME 1 · NUMBER 10 Public Health Foundation, Incorporated BOARD OF DIRECTORS Jack E. Wilson, PE, MSENV Fred T. Brown Jr., MPH, FACHE Sandra W. Green, MBA, MHA, BSPH Laura Helms Reece, DrPH President Group Senior Vice President President Chief Operating Officer Member of the Board of Directors Eastern Division East Coast Customer Management Group Rho TEC Inc. Carolinas HealthCare System MedAssets Inc. James Rosen, MBA, MSPH Delton Atkinson, MPH, MPH, PMP Kelly B. Browning, MA C. David Hardison, PhD Partner Vice President Executive Vice President Vice President, Chief Health Scientist Intersouth Partners Deputy Director American Institute for Cancer Research Science Applications International Corp. Jacqueline vdH Sergent, MPH, Division of Vital Statistics P. LaMont Bryant, PhD, RAC Deborah Parham Hopson, PhD, RN RD, LDN National Center for Health Statistics Product Director, Global Marketing Assistant Surgeon General Health Promotion Coordinator/ Centers for Disease Control and Prevention Ethicon Endo-Surgery/Johnson Associate Administrator Health Education Supervisor Barbara K. Rimer, DrPH & Johnson HIV/AIDS Bureau Granville-Vance (N.C.) District Executive Vice President Cynthia H. Cassell, PhD Health Resources and Services Health Department Ex Officio Administration Health Scientist, Epidemiology Team Ilene C. Siegler, PhD, MPH Dean Birth Defects Branch Joan C. Huntley, PhD, MPH Professor of Medical Psychology Alumni Distinguished Professor Division of Birth Defects and Adjunct Professor of Epidemiology Duke University UNC Gillings School of Global Developmental Disabilities UNC Gillings School of Global Public Health Jeffrey B. Smith, MHA, CPA National Center for Birth Defects and Public Health Partner Peggy Dean Glenn Developmental Disabilities Joseph F. -
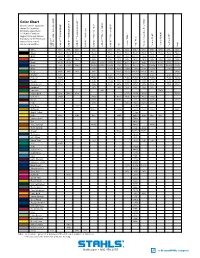
Color Chart ® ® ® ® Closest Pantone® Equivalent Shown
™ ™ II ® Color Chart ® ® ® ® Closest Pantone® equivalent shown. Due to printing limitations, colors shown 5807 Reflective ® ® ™ ® ® and Pantone numbers ® ™ suggested may vary from ac- ECONOPRINT GORILLA GRIP Fashion-REFLECT Reflective Thermo-FILM Thermo-FLOCK Thermo-GRIP ® ® ® ® ® ® ® tual colors. For the truest color ® representation, request Scotchlite our material swatches. ™ CAD-CUT 3M CAD-CUT CAD-CUT CAD-CUT CAD-CUT CAD-CUT CAD-CUT Felt Perma-TWILL Poly-TWILL Thermo-FILM Thermo-FLOCK Thermo-GRIP Vinyl Pressure Sensitive Poly-TWILL Sensitive Pressure CAD-CUT White White White White White White White White White* White White White White White Black Black Black Black Black Black Black Black Black* Black Black Black Black Black Gold 1235C 136C 137C 137C 123U 715C 1375C* 715C 137C 137C 116U Red 200C 200C 703C 186C 186C 201C 201C 201C* 201C 186C 186C 186C 200C Royal 295M 294M 7686C 2747C 7686C 280C 294C 294C* 294C 7686C 2758C 7686C 654C Navy 296C 2965C 7546C 5395M 5255C 5395M 276C 532C 532C* 532C 5395M 5255C 5395M 5395C Cool Gray Warm Gray Gray 7U 7539C 7539C 415U 7538C 7538C* 7538C 7539C 7539C 2C Kelly 3415C 341C 340C 349C 7733C 7733C 7733C* 7733C 349C 3415C Orange 179C 1595U 172C 172C 7597C 7597C 7597C* 7597C 172C 172C 173C Maroon 7645C 7645C 7645C Black 5C 7645C 7645C* 7645C 7645C 7645C 7449C Purple 2766C 7671C 7671C 669C 7680C 7680C* 7680C 7671C 7671C 2758U Dark Green 553C 553C 553C 447C 567C 567C* 567C 553C 553C 553C Cardinal 201C 188C 195C 195C* 195C 201C Emerald 348 7727C Vegas Gold 616C 7502U 872C 4515C 4515C 4515C 7553U Columbia 7682C 7682C 7459U 7462U 7462U* 7462U 7682C Brown Black 4C 4675C 412C 412C Black 4C 412U Pink 203C 5025C 5025C 5025C 203C Mid Blue 2747U 2945U Old Gold 1395C 7511C 7557C 7557C 1395C 126C Bright Yellow P 4-8C Maize 109C 130C 115U 7408C 7406C* 7406C 115U 137C Canyon Gold 7569C Tan 465U Texas Orange 7586C 7586C 7586C Tenn. -

Ch 5 NC Legislature.Indd
The State Legislature The General Assembly is the oldest governmental body in North Carolina. According to tradition, a “legislative assembly of free holders” met for the first time around 1666. No documentary proof, however, exists proving that this assembly actually met. Provisions for a representative assembly in Proprietary North Carolina can be traced to the Concessions and Agreements, adopted in 1665, which called for an unicameral body composed of the governor, his council and twelve delegates selected annually to sit as a legislature. This system of representation prevailed until 1670, when Albemarle County was divided into three precincts. Berkeley Precinct, Carteret Precinct and Shaftsbury Precinct were apparently each allowed five representatives. Around 1682, four new precincts were created from the original three as the colony’s population grew and the frontier moved westward. The new precincts were usually allotted two representatives, although some were granted more. Beginning with the Assembly of 1723, several of the larger, more important towns were allowed to elect their own representatives. Edenton was the first town granted this privilege, followed by Bath, New Bern, Wilmington, Brunswick, Halifax, Campbellton (Fayetteville), Salisbury, Hillsborough and Tarborough. Around 1735 Albemarle and Bath Counties were dissolved and the precincts became counties. The unicameral legislature continued until around 1697, when a bicameral form was adopted. The governor or chief executive at the time, and his council constituted the upper house. The lower house, the House of Burgesses, was composed of representatives elected from the colony’s various precincts. The lower house could adopt its own rules of procedure and elect its own speaker and other officers. -

2021 Medicare Advantage Provider Directory
2021 Medicare Advantage Provider Directory FirstCarolinaCare Insurance Company’s FirstMedicare Direct plans are HMO and PPO plans with a Medicare contract. Enrollment in FirstMedicare Direct plans depend on contract renewal. This document is available in other formats such as large print. Y0094_21_11246_C FirstMedicare Direct POS Plus FirstMedicare Direct POS Standard FirstMedicare POS Choice FirstMedicare Direct PPO Plus FirstMedicare Direct PPO Premier New Hanover Health FirstMedicare Select New Hanover Health FirstMedicare Platinum 2021 Medicare Advantage Provider Directory This directory is current as of 10/1/2020 This directory provides a list of FirstMedicare Direct’s current network providers. This directory is for the following North Carolina Counties: Brunswick, Buncombe, Chatham, Henderson, Hoke, Lee, Madison, McDowell, Montgomery, Moore, New Hanover, Pender, Richmond, Scotland, Transylvania, and Yancey. To access FirstMedicare Direct’s online provider directory, you can visit www.FirstMedicare.com. For any questions about the information contained in this directory, please call our Member Services at (877) 210-9167 or by TTY/TDD 711, 8 a.m. – 8 p.m., Local Time, 7-days a week. From April 1 – September 30, voicemail will be used on weekends and holidays. This document is available in other formats such as large print. Y0094_21_11246_C_FMD Approved 10/13/2020 1 Table of Contents Section 1-Introduction…………………………………………………………….......………3 What is the service area for FirstMedicare Direct?................................................................4 -

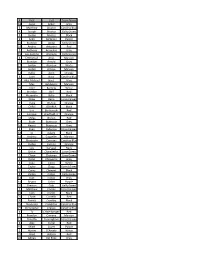
First Last Number Team Color Notes Wilfredo Acevedo 15 Orange
First Last Number Team Color Notes Wilfredo Acevedo 15 Orange Jason Acker 21 Purple Xavier Acosta 1 Carolina Blue cory acton 17 White Alexander Aguila 5 Navy Miguel Alba 4 Purple Jordan Alvarez 2 White Joseph Alvarez 3 Green Sean Ambrose 5 Carolina Blue BRANDON ANDAL 8 White Christian Aniello 10 Navy ANDRES ANTONINI 21 Lime Green antthony arancibia 1 Texas Orange David Archacki 23 Orange Jack (John) Archer 16 Garnett Playing on Royal Blue Luis Santino Arenado 21 Royal Blue James Arnaez 3 Royal Blue Jordan Arroyo 19 Royal Blue Ari Arteaga 11 Carolina Blue Zachary Audet 22 Black Brandon Auerbach 4 White Jack Azulay 13 Texas Orange Maxwell Baldaccini 3 Texas Orange Julian Barcelo 24 Orange JONATHAN BARDITCH 3 Gold Tyler Barrella 21 Texas Orange Brendan Bell 4 Gold Alexandro Bello 14 Garnett Playing on White Carlos Benitez 16 Gold Drew Beno 6 Texas Orange Brady Blocker 5 Royal Blue Eric Bonkowski 7 Royal Blue Alejandro Borjas 3 Red gionn brigitha 2 Garnett Playing with Red Team SETH BRIZEL 5 Green Keanu Buerosse 22 Green Jordan Bustabad 2 Black CJ Calero 16 White Andrew Cappeller 19 Gold Peter Carcioppolo 15 Purple Glenn Carlton 12 Orange Joseph Carnicella 2 Carolina Blue Jordan Carrion 11 Navy Gavin Casas 24 Navy Triston Casas 24 White Ihosvany Castaneda 6 Garnett Playing with Black Team EJ Cavieres 3 Navy Jeffrey "Drake" Chamberlin 4 Navy Yamil Chavarria 4 Orange Taylor Clapp 8 Texas Orange Corey Clement 22 Lime Green Dylan Cloonan 12 Red Liam Cogswell 11 Texas Orange Kaden Cohen 11 White Kurt Cohen 16 Green Jason Cohen 2 Green Kyle Cole -

NC DHSR HPCON: Comments from Orthonc
COMPETITIVE COMMENTS ON WAKE COUNTY 2018 OPERATING ROOM NEED DETERMINATION SUBMITTED BY ORTHONC ASC OrthoNC ASC (“OrthoNC”) (Project ID No. J-011561-18) proposes to develop a new ambulatory surgery center (“ASC”) with one operating room (“OR”) and one procedure room in North Raleigh/Wakefield. Eight additional applications were submitted in response to the need determination in the 2018 State Medical Facilities Plan (“SMFP”) for six ORs in Wake County: Comments Applicant Begin on page # 1. RAC Surgery Center (“RAC”) Project ID No. J-011551-18 17 Develop a new ASC with 1 OR and 2 procedure rooms in Raleigh 2. REX Surgery Center of Garner (“UNC REX Garner”) Project ID No. J-011553-18 24 Develop a new ASC with 2 ORs and 2 procedure rooms in Garner 3. UNC Health Care Panther Creek Ambulatory Surgery Center (“UNC Panther Creek”) Project ID No. J-011554-18 43 Develop a new ASC with 2 ORs and 2 procedure rooms in Panther Creek/West Cary 4. REX Hospital (“UNC REX”) Project ID No. J-011555-18 63 Add 2 shared ORs to its existing hospital in Raleigh for a total of 24 ORs 1 5. Green Level Ambulatory Surgical Center (“Duke Green Level”) Project ID No. J-011557-18 80 Develop a new ASC with 4 ORs in Cary 6. Duke Raleigh Hospital (“Duke Raleigh”) Project ID No. J-011558-18 87 Add 2 shared ORs to its existing hospital in Raleigh for a total of 17 ORs 7. WakeMed Surgery Center-North Raleigh (“WakeMed-NR”) Project ID No. J-011564-18 93 Develop a new ASC with 2 ORs and 2 procedure rooms in North Raleigh 8. -

Impact Report Fy 2015 2018
FROM INKLING TO INNOVATION UNC Office of Technology Commercialization How faculty and staff at the University of North Carolina at Chapel Hill take FY 2015 IMPACT ideas to market and innovations to scale 2018 REPORT Office of Technology Commercialization Impact Report UNC Office of Technology Commercialization FY2015-18 Impact Report 2 One of the reasons I came to Carolina as a faculty member in 1995 is because of our University’s commitment to be the leading innovation and entrepreneurship center in higher education. Today, Carolina has created and nurtured a strong culture of innovation that is turning the knowledge of our faculty and students into practical solutions, taking valuable ideas to the inventive edge. Thanks to the dedication of Judith Cone and her team, we are working strategically, collaborating creatively and fully activating this culture of success. The ripple effect of this commitment is making a global impact: Talented researchers and those with entrepreneurial aspirations are moving more ideas, more rapidly and more effectively, into the world where this work has the greatest impact. We are far from done – Carolina is committed to innovation and entrepreneurship that boldly addresses our world’s most pressing challenges. KEVIN GUSKIEWICZ INTERIM CHANCELLOR, UNC-CHAPEL HILL One of the most important things that we can do for the people of North Carolina and the people of this country is to create that next big opportunity that is going to have a chance to change the world and make a difference in our lives. BOB BLOUIN EXECUTIVE VICE CHANCELLOR AND PROVOST, UNC-CHAPEL HILL As a public institution and leading research university, Carolina has an obligation to seek the answer to this question: How do we ensure that the great talent of our faculty, staff and students is put to its highest use? For UNC-Chapel Hill, that means doing everything we can to support our people as they uncover solutions that make a real difference to the citizens of North Carolina and the world. -

South Carolina Department of Natural Resources
FOREWORD Abundant fish and wildlife, unbroken coastal vistas, miles of scenic rivers, swamps and mountains open to exploration, and well-tended forests and fields…these resources enhance the quality of life that makes South Carolina a place people want to call home. We know our state’s natural resources are a primary reason that individuals and businesses choose to locate here. They are drawn to the high quality natural resources that South Carolinians love and appreciate. The quality of our state’s natural resources is no accident. It is the result of hard work and sound stewardship on the part of many citizens and agencies. The 20th century brought many changes to South Carolina; some of these changes had devastating results to the land. However, people rose to the challenge of restoring our resources. Over the past several decades, deer, wood duck and wild turkey populations have been restored, striped bass populations have recovered, the bald eagle has returned and more than half a million acres of wildlife habitat has been conserved. We in South Carolina are particularly proud of our accomplishments as we prepare to celebrate, in 2006, the 100th anniversary of game and fish law enforcement and management by the state of South Carolina. Since its inception, the South Carolina Department of Natural Resources (SCDNR) has undergone several reorganizations and name changes; however, more has changed in this state than the department’s name. According to the US Census Bureau, the South Carolina’s population has almost doubled since 1950 and the majority of our citizens now live in urban areas. -

FULL BOARD MEETING January 28, 2021, 1:00PM Zoom
FULL BOARD MEETING January 28, 2021, 1:00PM Zoom Teleconference hosted in 105 South Building OPEN SESSION 1. Convene Meeting Richard Stevens, Chair 2. Roll Call Teresa Artis Neal, Secretary 3. Statement of Ethics 4. Consent Agenda I. Approval of November 12, 2020 Minutes (Regular Meeting) Attachment A II. Approval of Revised 2021 Meeting Dates Attachment B 5. Board of Trustees Chair’s Remarks Richard Stevens, Chair 6. Student Body President’s Remarks Reeves Moseley, Student Body President 7. Chancellor’s Remarks Dr. Kevin Guskiewicz, Chancellor 8. Carolina Together Testing Program Update Dr. Amir Barzin, Assistant Professor, UNC School of Medicine Dr. Amy Loftis, Medical Laboratory Supervisor, Department of Global Health & Infectious Disease 9. *Report of the Finance, Infrastructure & Audit Committee Haywood Cochrane, Committee Chair 10. *Report of the University Affairs Committee Chuck Duckett, Committee Chair 11. *Report of the External Relations Committee Gene Davis, Committee Chair CLOSED SESSION 12. *Report of the University Affairs Committee Chuck Duckett, Committee Chair 13. *Report of the External Relations Committee Gene Davis, Committee Chair *Some of the business to be conducted is authorized by the N.C. Open Meetings Law to be conducted in closed session. FULL BOARD MEETING January 28, 2021, 1:00PM Zoom Teleconference hosted in 105 South Building 14. Legal Update Charles Marshall, Vice Chancellor and General Counsel OPEN SESSION 15. Report of University Affairs Committee Chuck Duckett, Committee Chair 16. Adjournment Richard Stevens, Chair *Some of the business to be conducted is authorized by the N.C. Open Meetings Law to be conducted in closed session. MEMORANDUM To: Members of the Board of Trustees From: Richard Stevens, Chair Date: January 28, 2021 RE: Revised 2021 Meeting Dates Due to conflicts, the July and November 2021 BOT meetings need to be rescheduled. -

Linesthe Cancer Program of UNC-Chapel Hill & UNC Health Care Spring 2008 Cancer Survivorship: from Clinics N.C
30928_UNC.qxp 5/2/2008 1:04 PM Page 2 UNC Linebcancererger Comprehensive Cancer Center LinesThe Cancer Program of UNC-Chapel Hill & UNC Health Care Spring 2008 Cancer Survivorship: From Clinics N.C. CANCER HOSPITAL to Communities, UNC is There LINEBERGER COMPREHENSIVE CANCER CENTER For many cancer patients, the end of active treatment creates address the needs of the growing number of cancer survivors. a lot of uncertainty. After long periods of regular treatments There are now about 12 million cancer survivors in the U.S.; and doctor visits, the routine changes. But concerns, about 300,000 North Carolinians are survivors. challenges and potential "In the past the focus health problems remain. has almost entirely "Some have described been on treatment it as being 'dropped off a and 'beating' the cliff,' " says Elizabeth cancer," explains Marci Sherwood, coordinator of Campbell, the Center's cancer survivorship principal investigator programs. "Their cancer and professor of may be treated, but the nutrition at UNC's cancer is still part of their School of Public Health. Profile: life. As healthcare "Our cancer survivors Nancy Raab-TTraub professionals, we can need programs and 4 facilitate this transition services to help them up ... from active treatment to deal with long-term surveillance by attending health issues including to the concerns of the possible late effects of patient and managing their cancer. They some of the ongoing are concerned about physical issues related to wellness issues such as cancer and cancer Dr. Paul Godley (left) and Elizabeth Sherwood (right) meet with patient Nathan Ladd healthy eating, exercise, treatment." during his visit to the survivorship clinic. -
First Last Team Name 18 Jason Acker Grey 5 Matthew Alvarez Carolina
# First Last Team Name 18 Jason Acker Grey 5 Matthew Alvarez Carolina Blue 4 Joseph Alvarez Kelly Green 5 Jordan Alvarez Black 9 Sean Ambrose Purple 10 Brandon Andal Kelly Green 18 Andres Antonini Red 5 Anthony Arancibia Grey 15 Luis Santino Arenado Kelly Green 4 Emmanuel Arias Maroon 7 Brandon Arnold Grey 17 Jordan Aronson White 11 Jordan Arroyo Maroon 11 Kolbe Aven Orange 8 Joan Baez Carolina Blue 15 Alec-Michael Baez Grey 14 Max Baldaccini Maroon 23 Tyler Barrella White 5 Brendan Bell Red 1 Alexandro Bello Black 6 Drew Beno Forest Green 9 Trace Bishop Orange 19 CHRIS BOHRER Black 7 Eric Bonkowski Red 3 Enrique Bradfield, Jr Orange 23 Myles Brown Red 14 Bode Buerosse Grey 16 Keanu Buerosse Grey 2 Ryan Cabarcas Forest Green 18 CJ Calero Black 18 Andrew Cappeller Maroon 1 Alexander Carreras Carolina Blue 6 Jordan Carrion Orange 1 Luis Carvajal Navy 7 Drake Chamberlin Lime Green 5 Chase Chatman Lime Green 3 Dylan Chiaverini Grey 6 Joey Cicini White 12 Taylor Clapp Forest Green 9 Corey Clement Black 8 Kaden Cohen Kelly Green 12 Kurt Cohen Grey 14 Bryant Colon Purple 20 Preston Colp Kelly Green 3 Matthew Corpas Forest Green 24 Julio Cortez Black 24 Chase Costello Red 20 Patrick Crawley Black 25 Alexander Creighton Carolina Blue 21 Christopher Crespo Carolina Blue 4 Ty Crittenberger Red 7 Brandon Cumana Maroon 17 Timothy Cunningham Forest Green 6 Alex Curiel Red 16 Mikel Cuvet Purple 2 Hunter D'Amato White 21 Jared deFaria Red 22 Adrian Del Pozo Grey 17 Nicholas Del Prado Orange 22 Lanel Delgado Forest Green 22 ernest denis White 17 Gabriel -

CERF 2011 21St Biennial Conference of the Coastal and Estuarine Research Federation ABSTRACTS
CERF 2011 21st Biennial Conference of the Coastal and Estuarine Research Federation ABSTRACTS Ocean's Eleventh Hour by Paul Balicker SOCIETIES, ESTUARIES & COASTS: Adapting to Change 6-10 November 2011 • Daytona Beach, Florida, USA www.erf.org United States Environmental Protection Agency, National Estuary Program a network of voluntary community-based programs that safeguards the health of important coastal ecosystems across the country. Proud Sponsor of CERF 2011 Abstracts Book Daytona Beach, FL 6 - 10 November, 2011 Visit our Website at: http://water.epa.gov/type/oceb/nep Conference Abstracts 21st Biennial Conference of the Coastal and Estuarine Research Federation 6 - 10 November 2011 Daytona Beach, Florida, USA This book includes all of the abstracts referenced in the CERF 2011 Program Book. Abstracts are listed in alphabetical order by the first author's last name. The index in the back of the Abstract Book provides an alphabetical listing of all authors and page numbers of respective abstracts. CERF 2011 Conference Leadership Team Student Activities Conference Co-Chairs Chair Jim Fourqurean, Florida International University Amanda Kahn, University of North Carolina, Wilmington Holly Greening, Tampa Bay Estuary Program Student Career Event Scientific Program Leanna Heffner, University of Rhode Island Co-Chair David Rudnick, South Florida Water Management District Student Travel Awards Paul Carlson, Florida Marine Research Institute Co-Chair David Yoskowitz, Harte Research Institute for Gulf of Mexico Student Presentation Judging/Awards Studies (SEERS) Southeastern Estuarine Research Society Poster Chair Conference Oversight Linda Walters, University of Central Florida Joy Bartholomew, CERF HQ Alejandra Garza, CERF HQ Plenary and Synthesis Sessions Bill Nuttle, Eco-Hydrology Webmaster Chris Schneider, The Schneider Group Regional Issues Bob Virnstein, St.