Trauma Killers Objectives Case‐SCH
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Emergency Medicine – Trauma: What You Need to Know Whiteboard Animation Transcript with Kaushal Shah, MD
Emergency Medicine – Trauma: What You Need to Know Whiteboard Animation Transcript with Kaushal Shah, MD Trauma comes in two basic varieties: blunt trauma and penetrating trauma. Nonetheless, major trauma patients should always be approached the same way: primary survey followed by a secondary survey. Don’t let the blood and gore distract you. The primary survey entails a systematic assessment using ABCDE in order to identify the true life-threatening injuries and initiate resuscitation. Then a detailed head-to-toe exam should occur, which we call the secondary survey. A. Airway assessment. If blood, vomit or the patient’s own saliva is blocking the airway (which often occurs in unconscious patients), they will need suctioning and possibly intubation. B. Breathing. Examine the chest through inspection, auscultation, and palpation. You are looking for life-threatening injuries. Decreased breath sounds, subcutaneous emphysema, broken ribs, and tracheal deviation, are concerning for a tension pneumothorax, hemothorax, pulmonary contusions, flail chest, and cardiac tamponade. C. Circulation. If the patient has a fast heart rate or low blood pressure, suspect ongoing hemorrhage or blood loss, the number one cause of preventable death in trauma. Bleeding is likely in one of four locations: chest, abdomen, pelvis, or fractured long bones. Start IV fluids or blood transfusion through two big intravenous lines. D. Disability. A basic neurologic assessment will help you calculate a GCS or Glasgow Coma Scale. It evaluates Eye Opening, Verbal Response, and Motor Response that is universally understood on a 15-point scale. E. Exposure. The patient should be completely undressed to look for all injuries. -

Thoracic Gunshot Wound: a Tanmoy Ganguly1, 1 Report of 3 Cases and Review of Sandeep Kumar Kar , Chaitali Sen1, Management Chiranjib Bhattacharya2, Manasij Mitra3
2015 iMedPub Journals Journal of Universal Surgery http://www.imedpub.com Vol. 3 No. 1:2 ISSN 2254-6758 Thoracic Gunshot Wound: A Tanmoy Ganguly1, 1 Report of 3 Cases and Review of Sandeep Kumar Kar , Chaitali Sen1, Management Chiranjib Bhattacharya2, Manasij Mitra3, 1 Department of Cardiac Anesthesiology, Abstract Institute of Postgraduate Medical Thoracic gunshot injury may have variable presentation and the treatment plan Education and Research, Kolkata, India differs. The risk of injury to heart, major blood vessels and the lungs should be 2 Department of Anesthesiology, Institute evaluated in every patient with rapid clinical examination and basic monitoring and of Postgraduate Medical Education and surgery should be considered as early as possible whenever indicated. The authors Research, Kolkata, India present three cases of thoracic gunshot injury with three different presentations, 3 Krisanganj Medical College, Institute of one with vascular injury, one with parenchymal injury and one case with fortunately Postgraduate Medical Education and no life threatening internal injury. The first case, a 52 year male patient presented Research, Kolkata, India with thoracic gunshot with hemothorax and the bullet trajectory passed very near to the vital structures without injuring them. The second case presented with 2 hours history of thoracic gunshot wound with severe hemodynamic instability. Corresponding author: Sandeep Kumar Surgical exploration revealed an arterial bleeding from within the left lung. The Kar, Assistant Professor third case presented with post gunshot open pneumothorax. All three cases managed successfully with resuscitation and thoracotomy. Preoperative on table fluoroscopy was used for localisation of bullet. [email protected] Keywords: Horacic trauma, Gunshot injury, Traumatic pneumothorax, Emergency thoracotomy, Fluoroscopy. -

Femoral Shaft Fracture Fixation and Chest Injury After Polytrauma
This is an enhanced PDF from The Journal of Bone and Joint Surgery The PDF of the article you requested follows this cover page. Femoral Shaft Fracture Fixation and Chest Injury After Polytrauma Lawrence B. Bone and Peter Giannoudis J Bone Joint Surg Am. 2011;93:311-317. doi:10.2106/JBJS.J.00334 This information is current as of January 25, 2011 Reprints and Permissions Click here to order reprints or request permission to use material from this article, or locate the article citation on jbjs.org and click on the [Reprints and Permissions] link. Publisher Information The Journal of Bone and Joint Surgery 20 Pickering Street, Needham, MA 02492-3157 www.jbjs.org 311 COPYRIGHT Ó 2011 BY THE JOURNAL OF BONE AND JOINT SURGERY,INCORPORATED Current Concepts Review Femoral Shaft Fracture Fixation and Chest Injury After Polytrauma By Lawrence B. Bone, MD, and Peter Giannoudis, MD, FRCS Thirty years ago, the standard of care for the multiply injured tients with multiple injuries, defined as an ISS of ‡18, and patient with fractures was placement of the fractured limb in a patients with essentially an isolated femoral fracture and an splint or skeletal traction, until the patient was considered stable ISS of <18. Pulmonary complications consisting of ARDS, enough to undergo surgery for fracture fixation1. This led to a pulmonary dysfunction, fat emboli, pulmonary emboli, and number of complications2, such as adult respiratory distress pneumonia were present in 38% (fourteen) of thirty-seven syndrome (ARDS), infection, pneumonia, malunion, non- patients in the late fixation/multiple injuries group and 4% union, and death, particularly when the patient had a high (two) of forty-six in the early fixation/multiple injuries group; Injury Severity Score (ISS)3. -

Effect of Hypothermia on Haemostasis and Bleeding Risk: a Narrative Review
Review Journal of International Medical Research 2019, Vol. 47(8) 3559–3568 Effect of hypothermia on ! The Author(s) 2019 Article reuse guidelines: haemostasis and bleeding sagepub.com/journals-permissions DOI: 10.1177/0300060519861469 risk: a narrative review journals.sagepub.com/home/imr Thomas Kander and Ulf Schott€ Abstract It must be remembered that clinically important haemostasis occurs in vivo and not in a tube, and that variables such as the number of bleeding events and bleeding volume are more robust measures of bleeding risk than the results of analyses. In this narrative review, we highlight trauma, surgery, and mild induced hypothermia as three clinically important situations in which the effects of hypothermia on haemostasis are important. In observational studies of trauma, hypothermia (body temperature <35C) has demonstrated an association with mortality and morbidity, perhaps owing to its effect on haemostatic functions. Randomised trials have shown that hypothermia causes increased bleeding during surgery. Although causality between hypothermia and bleeding risk has not been well established, there is a clear association between hypothermia and negative outcomes in connection with trauma, surgery, and accidental hypothermia; thus, it is crucial to rewarm patients in these clinical sit- uations without delay. Mild induced hypothermia to 33C for 24 hours does not seem to be associated with either decreased total haemostasis or increased bleeding risk. Keywords Hypothermia, coagulopathy, haemostasis, bleeding, trauma, surgery, injury Date received: 20 March 2019; accepted: 13 June 2019 Introduction Many studies have been conducted to inves- Lund University, Ska˚ne University Hospital, Department tigate the effects of hypothermia on haemo- of Clinical Sciences Lund, Intensive and Perioperative stasis, and these have yielded contradictory Care, Lund, Sweden results. -

EDUCATION STANDARDS Tabe of Contents
2020 NATIONAL EMERGENCY MEDICAL SERVICES EDUCATION STANDARDS Tabe of Contents Executive Summary 4 Pathophysiology X Introduction X Life Span Development X Historical Development of EMS in the United States X The National EMS Education Standards X Public Health X Description, Explanation, and Rationale Related to the Update X Pharmacology X 2019 National EMS Scope of Practice Model Relationship X Principles of Pharmacology X NREMT Practice Analysis X Medication Administration X Domains of EMS: Learning, Competency, Authorization, and X Emergency Medications X Operational/Local Qualification X Education Standards vs. Instructional Guidelines vs. Curriculum X Airway Management, Respirations and Artificial Ventilation X What Are the Instructional Guidelines: X Airway Management X Beyond the Scope of the Project X Respiration X Degree Requirements X Artificial Ventilation X AEMT Accreditation X Portable Technologies X Assessment X Instructional Practices: X Scene Size-Up X Interprofessional Education, Simulation, Shadowing X Primary Assessment X Team Composition X History Taking X Sequence of Instruction X Secondary Assessment X Locally Identified Topics X Monitoring Devices X Implicit Expectations X Reassessment X Resource Documents/Appendix X Evidence Based Guidelines – NASEMSO Clinical Guidelines X Medicine X Education Standards with Noteworthy Adjustment X Medical Overview X Neurology X National EMS Education Standards X Abdominal and Gastrointestinal Disorders X Preparatory X Immunology X EMS Systems X Infectious Diseases X Research X -

Ad Ult T Ra Uma Em E Rgen Cies
Section SECTION: Adult Trauma Emergencies REVISED: 06/2017 4 ADULT TRAUMA EMERGENCIES TRAUMA ADULT 1. Injury – General Trauma Management Protocol 4 - 1 2. Injury – Abdominal Trauma Protocol 4 - 2 (Abdominal Trauma) 3. Injury – Burns - Thermal Protocol 4 - 3 4. Injury – Crush Syndrome Protocol 4 - 4 5. Injury – Electrical Injuries Protocol 4 - 5 6. Injury – Head Protocol 4 - 6 7. Exposure – Airway/Inhalation Irritants Protocol 4 - 7 8. Injury – Sexual Assault Protocol 4 - 8 9. General – Neglect or Abuse Suspected Protocol 4 - 9 10. Injury – Conducted Electrical Weapons Protocol 4 - 10 (i.e. Taser) 11. Injury - Thoracic Protocol 4 - 11 12. Injury – General Trauma Management Protocol 4 – 12 (Field Trauma Triage Scheme) 13. Spinal Motion Restriction Protocol 4 – 13 14. Hemorrhage Control Protocol 4 – 14 Section 4 Continued This page intentionally left blank. ADULT TRAUMA EMERGENCIES ADULT Protocol SECTION: Adult Trauma Emergencies PROTOCOL TITLE: Injury – General Trauma Management 4-1 REVISED: 06/2015 PATIENT TRAUMA ASSESSMENT OVERVIEW Each year, one out of three Americans sustains a traumatic injury. Trauma is a major cause of disability in the United States. According to the Centers for Disease Control (CDC) in 2008, 118,021 deaths occurred due to trauma. Trauma is the leading cause of death in people under 44 years of age, accounting for half the deaths of children under the age of 4 years, and 80% of deaths in persons 15 to 24 years of age. As a responder, your actions within the first few moments of arriving on the scene of a traumatic injury are crucial to the success of managing the situation. -

Staged Abdominal Re-Operation for Abdominal Trauma
TJTES Ulus Travma Derg. 2003 Jul;9(3):149-153 TURKISH JOURNAL OF TRAUMA & EMERGENCY SURGERY STAGED ABDOMINAL RE-OPERATION FOR ABDOMINAL TRAUMA Korhan TAVILOGLU, MD, FACS ABSTRACT Background: To review the current developments in staged abdominal re-operation for abdominal trauma. Methods: To overview the steps of damage control laparotomy. Results: The ever increasing importance of the resuscitation phase with current intensive care unit (ICU) support techniques should be emphasized. Conclusions: General surgeons should be familiar to staged abdominal re-operation for abdominal trauma and collaborate with ICU teams, interventional radiologists and several other specialties to overcome this entity. Key words: abdominal trauma, staged laparotomy, abdominal compartment syndrome, damage control surgery INTRODUCTION Feliciano et al.12 reported the survival in nine of ten During the past decade, a new surgical patients who underwent temporary laparotomy approach to patients with devastating trauma has with pad tamponade for hepatic injuries. In the emerged. Based on a modified operative beginning of the 1980’s, two studies reported sequence using rapid lifesaving techniques, abdominal packing followed by rapid abdominal definitive resection and reconstruction are closure that was used for treatment of delayed until the patient can be adequately coagulopathy of nonhepatic abdominal injuries. resuscitated and stabilized in the surgical intensive care unit.1-5 WHAT IS STAR? Damage control is currently the most common STAR is a technique of serial -

Traumatic Deceleration Injury of the Thoracic Aorta
ECHO ROUNDS Section Editor: Edmund Kenneth Kerut, M.D. Traumatic Deceleration Injury of the Thoracic Aorta Edmund Kenneth Kerut, M.D.,∗,∗∗ Glenn Kelley, M.D.,† Vivian Carina Falco, M.D.,† Ty Ovella, M.D.,‡ Lisa Diethelm, M.D.,‡ and Frederick Helmcke, M.D.† ∗Departments of Pharmacology and Physiology, Louisiana State University Health Sciences Center, New Orleans, Louisiana, ∗∗Heart Clinic of Louisiana, Marrero, Louisiana, †Division of Cardiology, Department of Medicine, Louisiana State University Health Sciences Center, New Orleans, Louisiana, and ‡Department of Radiology, Louisiana State University Health Sciences Center, New Orleans, Louisiana (ECHOCARDIOGRAPHY, Volume 22, September 2005) deceleration, trauma, transection, aorta, transesophageal echocardiography, multislice computed tomography A 42-year-old intoxicated male pedestrian to surgery, where a spiral, subtotal, subadventi- was struck by a motor vehicle and “thrown” 45 tial aortic disruption (see discussion) involving feet. The patient did not lose consciousness. He three-fourths of the circumference of the aorta had no specific localized pain, and was initially was found.1,2 The tear was successfully resected noted to have only minor limb abrasions. He and replaced with a composite thoracic graft. was then admitted to the trauma center for ob- Blunt traumatic chest injury (deceleration in- servation. A screening CT was performed using jury) most often occurs from a steering wheel in- a16row multidetector CT scanner. It revealed jury or from a fall from a height. This may result a mediastinal hematoma, and also an aortic in myocardial contusion, traumatic ventricular pseudoaneurysm with an intraluminal defect septal defect, tricuspid or mitral valve trauma, at the level of the aortic isthmus (Fig. -

Chapter 1 - Trauma Team from Prehospital Through the Emergency Department Test Questions
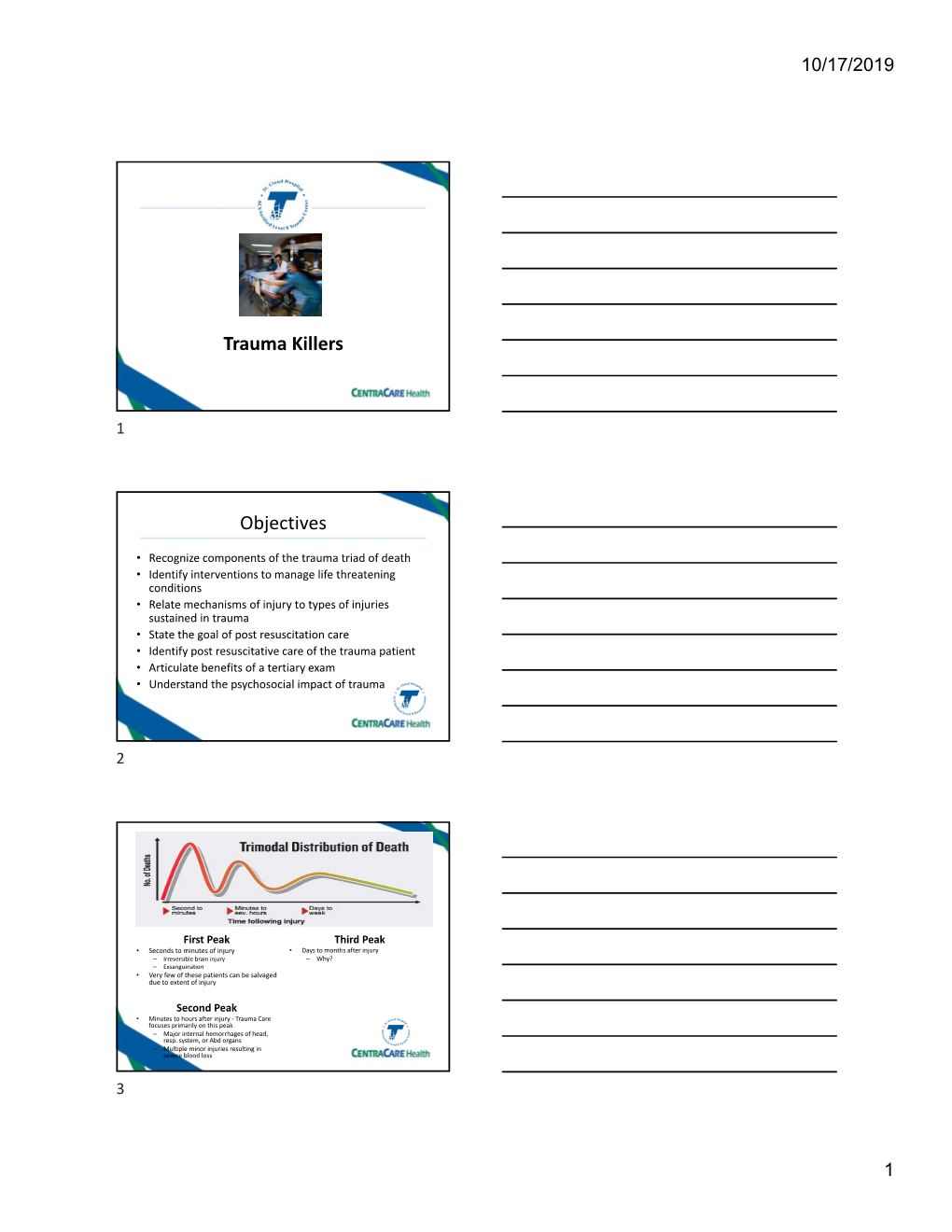
Chapter 1 - Trauma Team from Prehospital through the Emergency Department Test Questions 1. As the prehospital provider approaches the scene of a trauma call, they perform a. a radio transmission to the hospital b. a scene size up c. an estimate of neck size for c-collar d. an estimate of victim’s height and weight 2. Field intubation has been proven to improve outcome in a. patients with BP less than 90 mm Hg b. patients with GCS less than 9 c. patients with acute respiratory distress d. none of the above 3. A proven technique of hemorrhage control is a. Direct pressure b. Elevate above the heart c. Pressure points d. Cold application 4. Prehospital care for apparent pelvic fractures includes a. DO NOT ROCK or palpate the pelvis in the prehospital arena b. Avoid log rolling as much as possible c. Apply splint if in your area protocols d. All of the above 5. Most preventable deaths in trauma care are due to a. Delay in CPR b. Cardiac tamponade c. Airway obstruction d. Tension pneumothorax STN 2012 Electronic Library: Chapter 1 - Trauma Team from Prehospital Through the Emergency Department Test Questions 2 6. For resuscitation to occur, there must be a. Cellular perfusion and tissue oxygenation b. Restoration of a blood pressure greater than 90mm Hg c. A hemoglobin greater than 9g/dL d. A PaO2 greater than 80 mm Hg 7. The Trauma Triad of Death is a. Hypotension, tachycardia and decreased urine output b. Infection, inadequate nutrition, DVT’s c. Hypothermia, acidosis and coagulopathy d. -

Incidence of Asymptomatic Pulmonary Embolism in Moderately to Severely Injured Trauma Patients David J
The Journal of TRAUMA Injury, Infection, and Critical Care Incidence of Asymptomatic Pulmonary Embolism in Moderately to Severely Injured Trauma Patients David J. Schultz, MD, Karen J. Brasel, MD, MPH, Lacey Washington, MD, Lawrence R. Goodman, MD, Robert R. Quickel, MD, Randolph J. Lipchik, MD, Todd Clever, BS, and John Weigelt, MD Background: Chest computed tomo- sessed using an anatomic scoring system. patients receiving pharmacologic prophy- graphic (CT) scanning is used frequently Patients not receiving anticoagulation laxis had a PE. to evaluate symptomatic patients for pul- were followed. Conclusion: Asymptomatic PE occur monary embolus (PE). The incidence of Results: Twenty-two of 90 patients in 24% of moderately to severely injured PE diagnosed by helical CT scanning in had a PE. Four had major clot burden, patients. Age, head, chest, and lower ex- asymptomatic patients is unknown. including one patient with a saddle embo- tremity injury are associated with an in- Methods: Asymptomatic trauma pa- lus. Risk factors for asymptomatic PE in- creased risk. Standard thromboembolic tients with an Injury Severity Score > 9 clude age (odds ratio [OR], 1.04), head prophylaxis is not reliably protective. were studied with contrast-enhanced heli- injury (OR, 6.78), chest injury (OR, 4.51), Key Words: Computed tomographic cal CT images of the chest, pelvis, and lower extremity injury (OR, 5.03), and scanning, Pulmonary embolus, Head in- lower extremities. Clot burden was as- transfusion (OR, 3.42). Thirty percent of jury, Chest injury, Transfusion. J Trauma. 2004;56:727–733. hromboembolic complications are common in the uate respiratory symptoms in these patients. -

Modern Management of Traumatic Hemothorax
rauma & f T T o re l a t a m n r e u n o t J Mahoozi, et al., J Trauma Treat 2016, 5:3 Journal of Trauma & Treatment DOI: 10.4172/2167-1222.1000326 ISSN: 2167-1222 Review Article Open Access Modern Management of Traumatic Hemothorax Hamid Reza Mahoozi, Jan Volmerig and Erich Hecker* Thoraxzentrum Ruhrgebiet, Department of Thoracic Surgery, Evangelisches Krankenhaus, Herne, Germany *Corresponding author: Erich Hecker, Thoraxzentrum Ruhrgebiet, Department of Thoracic Surgery, Evangelisches Krankenhaus, Herne, Germany, Tel: 0232349892212; Fax: 0232349892229; E-mail: [email protected] Rec date: Jun 28, 2016; Acc date: Aug 17, 2016; Pub date: Aug 19, 2016 Copyright: © 2016 Mahoozi HR. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Hemothorax is defined as a bleeding into pleural cavity. Hemothorax is a frequent manifestation of blunt chest trauma. Some authors suggested a hematocrit value more than 50% for differentiation of a hemothorax from a sanguineous pleural effusion. Hemothorax is also often associated with penetrating chest injury or chest wall blunt chest wall trauma with skeletal injury. Much less common, it may be related to pleural diseases, induced iatrogenic or develop spontaneously. In the vast majority of blunt and penetrating trauma cases, hemothoraces can be managed by relatively simple means in the course of care. Keywords: Traumatic hemothorax; Internal chest wall; Cardiac Hemodynamic response injury; Clinical manifestation; Blunt chest-wall injuries; Blunt As above mentioned the hemodynamic response is a multifactorial intrathoracic injuries; Penetrating thoracic trauma response and depends on severity of hemothorax according to its classification. -
General Approach to Traumatic Injuries
Cambridge University Press 978-1-108-45028-7 — The Emergency Medicine Trauma Handbook Edited by Alex Koyfman , Brit Long Excerpt More Information Chapter General Approach to 1 Traumatic Injuries Ryan O’Halloran and Kaushal Shah Introduction Trauma is the fourth leading cause of death overall in the United States and the number one cause of death for ages 1 to 44 – second only to heart disease and cancer in those older than 45 (CDC).1 As the disease burden from infectious diseases declines and secondary preven- tion of chronic conditions improves, the relative importance of the practice of trauma care becomes even more apparent. Though safety engineering has improved across many indus- tries (one need only consider examples such as crosswalk and bike lane planning, football helmet technology, and motor vehicle computerized improvements), trauma remains a significant threat to life and limb in emergency medicine. The Trauma Team The American College of Surgeons, the governing body for credentialing trauma centers, has provided guidelines for optimal resources necessary for a coordinated response to a critically injured trauma patient. Box 1.1 demonstrates the players suggested for an optimal response. While response teams may vary, several principles are key to the functioning of a good, interdisciplinary team. These include clearly establishing roles for members of the team, following policy and protocols established in advance, briefing prior to the arrival of the patient, and debriefing after the event, whether immediately after the event