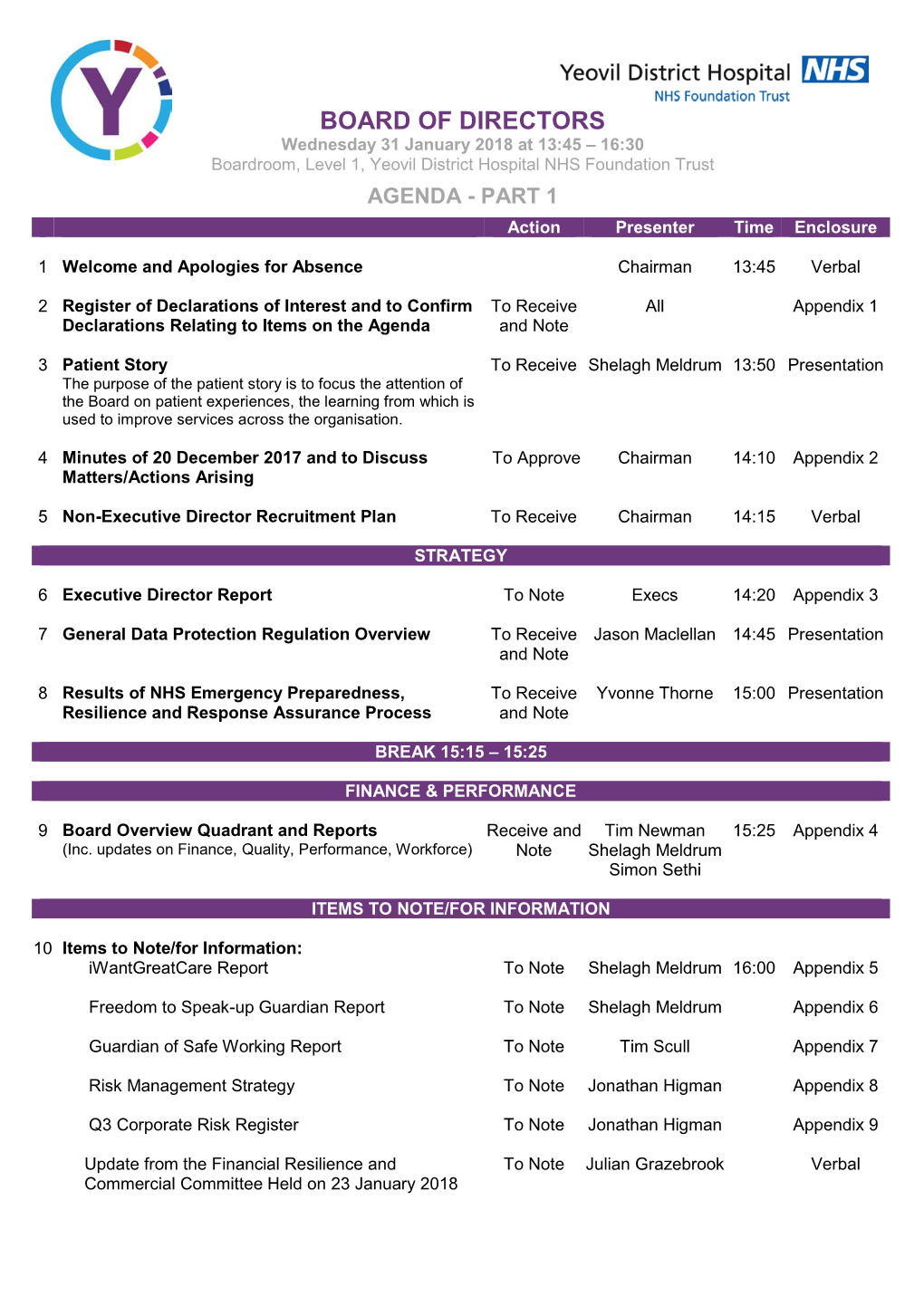
Board of Directors
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Spring 2021 FULL CHAT
Spring 2021 FULL CHAT Newsletter of Somerset Advanced Motorcyclists Group No. 1241 PHOTO FULL CHAT 1 SPRING 2021 SAM Officers Chair Kev Colmer 07557 552424 Deputy Chair Martin Surrey 07813 786427 Secretary Andy Bourne Deputy Secretary Andy Hall 01963 350452 Treasurer Rab Lavender 07968 283790 Membership Sec. Dave Parker 07340 180989 Chief Observer Gina Herridge 07745 052815 Training Team Jim Donnelly 07960 812688 Callum Bremner 07859 892566 Events Coordinator Jez Martin 07590 368808 Observer Co-ord. Tony Sauer 07983 088312 Taster Coordinator Roger Moffatt 07812 061793 Follow on Twitter Member’s Rep Janet Short @ SAMtweeps Publicity Officer TBA TBA Spons/Advertising Georges Dupuis 07999 349667 Recruitment Lead Georges Dupuis 07999 349667 Merchandise Nathan Beesley 07875 739071 Young Ambassador Richard Padfield 07478 675800 IT Lead Jez Martin 07590 368808 Social Media Lead Tom Moore 07739 191203 Full Chat Editorial Gina Herridge 07745 052815 Team Graham Tulloch 07825 201650 [email protected] www.somersetadvancedmotorcyclists.org.uk google community: Somerset Advanced Motorcyclists Facebook: Somerset Advanced Motorcyclists (Public plus Members Only pages) Front Cover: Kaye May on Countisbury Hill near Lynmouth, offering us a taste of freedom to come in the coming months. FULL CHAT 2 SPRING 2021 FORWARD OBSERVATIONS As we take the baby steps out of the third, and for me, most draining lockdown, it seems almost too good to be true that we are allowed out on our bikes, and to see at least a couple of our friends at a time. My feeling is that just about every one of us is un- characteristically fragile, and prone to acts and reac- tions which we would not recognize as part of who we think we are. -

Enjoy the Summer Riding
Enjoy the Summer Riding Welcome from ChainLinkEd MAGAZINE OF This edition is packed full of ride write ups, including our Super Sunday ride outs for members. BRISTOL ADVANCED I have included a ride write up from Steve Godfrey. A first MOTORCYCLISTS account Associate ride he did last September. Mar – Jun 19 Edition Thank you for those who volunteer to write up the ride out Issue 62 BAM IS AFFILIATED TO THE reports. It’s what keeps the magazine interesting as well as reading other riders accounts of the BAM ride outs, be they INSTITUTE OF ADVANCED Associate of Full Member. It’s bamper full of them. MOTORISTS (GROUP No. 1258) ARTICLES MAY ALSO BE PUBLISHED ON THE Steve Godfrey will be assisting me in the production of the GROUPS WEBSITE AND IN OTHER IAM GROUP Chain Link going forward. Steve will be providing his IT know NEWSLETTERS. THE OPINIONS EXPRESSED IN THIS NEWSLETTER ARE THOSE OF THE INDIVIDUAL how and we’ll be looking at blogs and video content for the CONTRIBUTORS AND DO NOT NECESSARILY FORM THE VIEWS OF THE EDITOR, BAM OR THE IAM. electronic versions of your Magazine. BAM ARE NOT RESPONSIBLE FOR THE CONTENTS OR ACCURACY OF ANY ADVERTS FEATURED IN THIS PUBLICATION. THIS EXTENDS TO THE LETTERS Remember the content and popularity of the Chain Link is with SUBMITTED BY READERS. all you BAM members and I look forward to your write ups no Image - FRONT COVER – BAM RIDE matter what they are. OUTS Visit us With the great weather comes great ride outs so enjoy but most of all be safe. -
5.A. Trustees Report
inspiring philanthropy Trustees’ Annual Report & Financial Statements 2016/17 Registered Charity No. 1094446 Registered Company No. 04530979 Contents Page Welcome and Key Achievements 1 Trustees’ Report 3 Statement of Trustees’ Responsibilities 16 Independent Auditors’ Report 17 Financial Statements 19 Somerset Community Foundation Welcome to our Annual Report for 2016/17 Somerset Community Foundation’s provisionally agreed our fourth mission is to be the catalyst for worth £25,000; inspirational philanthropy, providing a • produced our first ‘Vital Signs’ simpler and more effective way for donors report, highlighting the hidden to make a lasting difference in Somerset needs in our communities and the through our community investment and opportunities for philanthropy to thought leadership. respond; • received our largest one-off During 2016/17 we consolidated our donation from an individual; and position as the leading organisation to • grew our endowment to over £5m. deliver inspiring philanthropy in Somerset. We worked with more donors and funders Following the EDF Final Investment than ever before, and increased our Decision and the Government’s final investment into local voluntary approval for the Hinkley Point C project, organisations, charities and social we undertook considerable work to enterprises. prepare for the launch of the EDF Energy Community Fund in 2017/18. We also In particular we: began negotiations with the Access Foundation to diversify our social • awarded grants worth £516,234 to investment programme with almost -

Controversy Over Wedding Venue Planning
THE WEEK IN East Bristol & North East Somerset FREE Issue 586 24th July 2019 Read by more than 40,000 people each week Controversy over wedding venue planning bid A planning application to create a wedding venue in the committee, which met last Tuesday, is unhappy and has Hanham Abbots Conservation Area is causing controversy. asked South Gloucestershire Council to take enforcement The 90-guest marquee for wedding business Bickley Barns action. at Bickley Farm in Abbots Road has already been erected. The application has been submitted to South Gloucestershire But Hanham Abbots Parish Council’s environment Council by Graham New, who was involved in forming the Bickley Farm Friends of Hanham Abbots Conservation Group. He was chairman although he resigned following last week’s meeting, saying it is clear his views for the area are “not aligned” with the rest of the group. The application is for a marquee and change of use of part of an existing barn. Weddings would be held from 1st April until 31st October. Parking for 30 cars is proposed. The application says the position of the marquee doesn’t harm the conservation area or Green Belt. An accompanying transport statement concludes there are no highway safety issues. A noise report says that with appropriate mitigation, there will be no adverse impact on neighbours. This includes using highly directional loudspeakers, an in-house PA system that can be set at a restricted maximum noise level and signs asking people to leave quietly. Mr New attended the parish meeting, as did several local residents who are unhappy with the plans. -

Police Aviation News September 2015
Police Aviation News September 2015 ©Police Aviation Research Number 233 September 2015 PAR Police Aviation News September 2015 2 PAN—Police Aviation News is published monthly by POLICE AVIATION RESEARCH, 7 Wind- mill Close, Honey Lane, Waltham Abbey, Essex EN9 3BQ UK. Contacts: Main: +44 1992 714162 Cell: +44 7778 296650 Skype: BrynElliott E-mail: [email protected] Police Aviation Research Airborne Law Enforcement Member since 1994—Corporate Member since 2014 SPONSORS Airborne Technologies www.airbornetechnologies.at AeroComputers www.aerocomputers.com Avalex www.avalex.com Broadcast Microwave www.bms-inc.com Enterprise Control Systems www.enterprisecontrol.co.uk FLIR Systems www.flir.com L3 Wescam www.wescam.com Powervamp www.powervamp.com Trakka Searchlights www.trakkacorp.com Airborne Law Enforcement Association www.alea.org LAW ENFORCEMENT BULGARIA BORDER CONTROLS: Bulgaria will increase the number of helicopters available to the border authorities to monitor the refugee flows close to the state border. After leaving their own countries the ongoing tide of migrants from such as Africa and the Middle East enter Europe either via the dangerous southern sea crossing to Italy or Malta or via a north- er route through Greece and Turkey. In the latter case many end up trying to pass through Bulgaria. Prime Minister Boyko Borisov has announced additional resources to cover the Greek and Turkish border crossings. More than 15,000 people have been detained trying to illegally cross the border in the past six months. Helicopters of the General Directorate of Border Police are monitoring the Bulgarian- Macedonian and part of the Bulgarian-Greek borders at regular intervals to meet a strict schedule of regular flights. -
Read Or Download Searchable Pdf Version
THE LINK the newsletter of Bristol Advanced Motorists Circulation 450 no: 270 Sept 2014 The Newsletter of Bristol Advanced Motorists We hope you will find this September newsletter interesting. This LINK is a little different. There is much Group and Chiswick News. A few Letters. A Meeting Summary of Freewheelers Motorcycle EVS, and to continue the theme there’s a Motorcycle article near the back. On the back page are Contact Details for the Club Committee. Members, feel free to contact us to talk about what the Club is doing, and what you would like to see it do. In the middle find details of upcoming meetings, 3-in-a-Car driving update sessions, etc. on the Calendar. We hope to see you at (even just) one of our events soon. Got something to say? Please don’t be shy. Contact the Editor now. Find more information on our website www.iam-bristol.org.uk - in fact, this newsletter is put-up there about a week after you receive this hard copy. Would you like to read it there and cancel your hard copy? You can also sign up to our email distribution of IAM and Group news releases. Regards, PAUL, the Editor If you want to write something for the LINK – or advertise – contact: [email protected] 0117 960 8494 21 De Verose Court Hanham BRISTOL BS15 3SW th COPY DEADLINE for the next issue is: Sat 11 October Bristol Advanced Motorists Registered Charity No 289807 Run entirely by volunteers Affiliated to the IAM Ltd: Group no: 1009 Secretary. -
Issue 56 Aug – Oct 2017
ISSUE 56 AUG – OCT 2017 B R I S T O L A D V A N C E D M O T O R C Y C L I S T S 2 C O N T E N T S S U M M E R I S S U E 5 6 A U G – O C T 2 0 1 7 R E G U L A R S R E V I E W S & R E P O R T S 5 Kipper’s Komments 16 The Big Quiz 6 Chairman’s Chatter 18 Mendip Meander 8 Super Sundays 20 Sammy Millers Motorcycle Museum 11 The News At BAM 22 ‘My First Ride Out’ 14 CONGRATULATIONS – 28 Associate Group Ride TEST PASSES 26 BAM Events Calendar 30 GWAAC Ride 4 Life 27 Race Calendar 32 GWAA Talk from Coalpit Heath meeting 14 June 39 Useful Contacts 43 IFRD Event 40 Kessi’s Kapers BAM IS AFFILIATED TO THE INSTITUTE OF ADVANCED MOTORISTS (GROUP No. 1258) ARTICLES MAY ALSO BE PUBLISHED ON THE GROUPS WEBSITE AND IN OTHER IAM GROUP NEWSLETTERS. THE OPINIONS EXPRESSED IN THIS NEWSLETTER ARE THOSE OF THE INDIVIDUAL CONTRIBUTORS AND DO NOT NECESSARILY FORM THE VIEWS OF THE EDITOR, BAM OR THE IAM. BAM ARE NOT RESPONSIBLE FOR THE CONTENTS OR ACCURACY OF ANY ADVERTS FEATURED IN THIS PUBLICATION. Images - FRONT COVER – WEB IMAGE CONTENTS PAGE – DONATED HOLIDAY IMAGE B R I S T O L A D V A N C E D M O T O R C Y C L I S T S 3 B R I S T O L A D V A N C E D M O T O R C Y C L I S T S 4 Kipper’s Komments Welcome to the Summer Edition of Chain Link It has been yet again a busy time for BAM, with lots of new associates, successful test passes and new observer passes so welcome and well done to you all. -

In This Issue TT EXPERIENCE BAM WELSH WEEKEND RIDE OUT
In this issue TT EXPERIENCE BAM WELSH WEEKEND RIDE OUT REPORTS THE LAST EVER VIEW FROM THE SIDE B R I S T O L A D V A N C E D M O T O R C Y C L I S T S 2 S U M M E R I S S U E 4 8 A U G – O C T 2 0 1 5 R E G U L A R S R I D E R E P O R T S 5 Kipper’s Komments 14 Last of the Autumn Sun 2014 7 Chairman’s Chatter 16 First Ride, First Report With Chips 8 Super Sundays 22 You Take The High Road 10 The News At BAM 43 Associates Group Ride Taster 18 CONGRATULATIONS – TEST PASSES 45 Jurassic & Chips 19 Useful Contacts 51 The Long Way Round 30 BAM Events Calendar F E A T U R E S 31 2015 Super Bike Race Calendar 21 DWDAM – Ladies Day 44 Puzzle Time 24 View From The Side – The Last Time! 54 Kessi’s Kapers 33 Tales of an Isle of Man TT 58 Retail Therapy 46 Rhayader There & Back On A Bike Articles may also be published on the group’s website and in other IAM group newsletters. The opinions expressed in this newsletter are those of the individual contributors and do not necessarily form the views of the editor, BAM or the IAM B R I S T O L A D V A N C E D M O T O R C Y C L I S T S 3 B R I S T O L A D V A N C E D M O T O R C Y C L I S T S 4 Phew it’s been warm out there and the roads have been much busier with motorcyclists taking full advantage of the conditions, which includes me getting out onto the group rides and the Wales weekend in Rhayader. -

From Chainlinked
Welcome from ChainLinkEd Welcome to the 2019 edition of the BAM magazine Chain Link. First issue of the year and the remaining three, throughout 2019, will be electronic only unless you already subscribe to MAGAZINE OF receive a hard copy version in 2019. If you wish to receive a hard copy version for the remainder of the year there is a BRISTOL ADVANCED £5.00 subscription fee to cover the administration cost putting the magazine together, printing and postage. MOTORCYCLISTS So, we appear to have put the worst of the weather behind us Nov – Jan 19 Edition and some of you are bringing your two, three or even four- Issue 61 wheel steeds out of hibernation and on to the roads. BAM IS AFFILIATED TO THE INSTITUTE OF ADVANCED The format is pretty much the same, but we have had readers MOTORISTS (GROUP No. 1258) wanting to add sections in that will prove interesting to many of you. ARTICLES MAY ALSO BE PUBLISHED ON THE GROUPS WEBSITE AND IN OTHER IAM GROUP NEWSLETTERS. THE OPINIONS EXPRESSED IN THIS I have put a 12-month BAM Events Diary in this issue so you NEWSLETTER ARE THOSE OF THE INDIVIDUAL CONTRIBUTORS AND DO NOT NECESSARILY FORM can all start filling up your diaries and planning ahead. THE VIEWS OF THE EDITOR, BAM OR THE IAM. BAM ARE NOT RESPONSIBLE FOR THE CONTENTS OR ACCURACY OF ANY ADVERTS FEATURED IN THIS You’ll also be given a look ahead of events locally, around the PUBLICATION. THIS EXTENDS TO THE LETTERS SUBMITTED BY READERS. -

35P MARCH 2014
NT KN E OL R L B MARCH 2014 35p LANZA HAIRCARE EST. 1994 HAIR BY DESIGN HAIR EXTENSION SPECIALISTS For the ultimate hairstyling experience we will make every clients visit unique, and work with you to create your own individual style. Sam is now offering RACOON HAIR EXTENSIONS, everything from simply refreshing your current style to developing a whole new image. Lisa, Rachael, Sam and Lauren thank all their existing clients for their continuous support. Hair by Design will be closed on Mondays A WARM WELCOME AWAITS ALL. Gift vouchers are available for all treatments The Pines, Brent Street, Brent Knoll Call us now on 01278 760 506 Please mention the Brent Knoll News when replying to adverts 3 The Parish of Three Saints St Christopher, Lympsham St Michael, Brent Knoll St Mary, East Brent BAPTISM WEDDING When do we hold baptisms? How do we book our wedding? - on the fourth or fifth Sunday of a month at - please contact our Parish Administrator in 12.15pm or 1.15pm; the Church Office, who will discuss with we normally have one family at each time, you availability of dates and times; will talk however, there may be occasions when we to you about the qualifying connection you have another child to baptise and so there have with the parish; and will take you and will be two families together; your fiancé’s details; - or at our regular worship on a Sunday - you will then be contacted by our vicar to morning at 10.00am; arrange a date to meet. There will be exceptions due to the church CHURCH OFFICE calendar Church Road, East Brent, TA9 4HZ How do you book a baptism? E-mail: [email protected] - collect an application form the Church Phone: 01278 769082 Office Open Tuesday & Wednesday, 10.30am-3.30pm Priest in Charge Revd. -

WESTON-SUPER-MARE TOWN COUNCIL 2014/2015 Invoices
WESTON-SUPER-MARE TOWN COUNCIL 2014/2015 Invoices totalling £500 or more for the period: 01/07/2014 - 31/07/2014 Invoice Number Cost Centre Description Nominal Code Description Transaction Detail Invoice Date Net VAT Total Supplier Account Name IMPCHQ2455 Central Grounds Maintenance Petrol / Diesel Fuel for June 2014 01/07/2014 £470.16 £94.03 £564.19 Atos Wordline UK Ltd re Fuelgenie 161548135 Blakehay Central Costs Utilities - Heat & Light Gas 01/03-25/03/2014 01/07/2014 £652.57 £130.51 £783.08 BRITISH GAS - 600205105 D/D 161548136 Blakehay Central Costs Utilities - Heat & Light Gas 26/03-24/04/2014 01/07/2014 £571.80 £114.36 £686.16 BRITISH GAS - 600205105 D/D HONORIAMAUG-OCT Civic Support Mayors Allowance Mayor honoriam Aug-Oct 01/07/2014 £1,075.00 £0.00 £1,075.00 Mrs R Willis 140257AUGUST Museum NNDR 140257AUGUST/18096/North Somer 01/07/2014 £2,579.00 £0.00 £2,579.00 North Somerset Council MCFCHQ283 Mayors Charity Due 1 ProceedsCllrMorrischarityfund 03/07/2014 £2,141.00 £0.00 £2,141.00 Freewheelers EVS MCHCHQ282 Mayors Charity Due 1 ProceedsCllrMorris charityfund 03/07/2014 £2,141.00 £0.00 £2,141.00 RNLI Weston-super-Mare MCFCHQ281 Mayors Charity Due 1 ProccedsCllrMorris charityfund 03/07/2014 £2,141.00 £0.00 £2,141.00 Weston Hospice Care 5778 Earmarked Reserves EMR Public conveniences Toilet refurb 5th payment 04/07/2014 £19,000.00 £3,800.00 £22,800.00 Chedvale Construction Ltd 19072 Central Grounds Maintenance Staffing Costs K. Waite&A. Mason 28/6-4/7/14 05/07/2014 £684.50 £136.90 £821.40 RBS Invoice Finance Limited 800116249 Earmarked -

2015-16 Bristol Health Partners Annual Review (PDF)
About Bristol Health Partners The partner organisations employ Bristol Health Partners is a collaboration between the city’s three NHS trusts, three clinical commissioning groups, two universities and its local authority. We exist to improve the health of those who live in and around Bristol, and the services on which they rely. The nine organisations formed Bristol Health Partners voluntarily, and it is funded by contributions from the partners. Find out more about us at: www.bristolhealthpartners.org.uk/about-us/ Research income for the partner organisations is 39,000 £180 people million Together the partners have an annual turnover £4.3 of over billion The partners serve 1,083,000 people living in the Bristol area Avon and Wiltshire Mental Health Partnership NHS Trust Bristol Clinical Commissioning Group North Bristol NHS Trust North Somerset Clinical Commissioning Group South Gloucestershire Clinical Commissioning Group University Hospitals Bristol NHS Foundation Trust Contents Welcome from Chair Andrea Young ........................................................................................................... 3 Update from Director David Relph ................................................................................................................. 4 Milestones in 2015-16 .................................................................................................................................................................... 6 The Bristol Health and Care Awards 2016 ..................................................................................