FDA Briefing Document
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dextromethorphan Attenuates Sensorineural Hearing Loss in an Animal Model and Population-Based Cohort Study
International Journal of Environmental Research and Public Health Article Dextromethorphan Attenuates Sensorineural Hearing Loss in an Animal Model and Population-Based Cohort Study Hsin-Chien Chen 1,* , Chih-Hung Wang 1,2 , Wu-Chien Chien 3,4 , Chi-Hsiang Chung 3,4, Cheng-Ping Shih 1, Yi-Chun Lin 1,2, I-Hsun Li 5,6, Yuan-Yung Lin 1,2 and Chao-Yin Kuo 1 1 Department of Otolaryngology-Head and Neck Surgery, Tri-Service General Hospital, National Defense Medical Center, Taipei 114, Taiwan; [email protected] (C.-H.W.); [email protected] (C.-P.S.); [email protected] (Y.-C.L.); [email protected] (Y.-Y.L.); [email protected] (C.-Y.K.) 2 Graduate Institute of Medical Sciences, National Defense Medical Center, Taipei 114, Taiwan 3 School of Public Health, National Defense Medical Center, Taipei 114, Taiwan; [email protected] (W.-C.C.); [email protected] (C.-H.C.) 4 Department of Medical Research, Tri-Service General Hospital, National Defense Medical Center, Taipei 114, Taiwan 5 Department of Pharmacy Practice, Tri-Service General Hospital, National Defense Medical Center, Taipei 114, Taiwan; [email protected] 6 School of Pharmacy, National Defense Medical Center, Taipei 114, Taiwan * Correspondence: [email protected]; Tel.: +886-2-8792-7192; Fax: +886-2-8792-7193 Received: 31 July 2020; Accepted: 28 August 2020; Published: 31 August 2020 Abstract: The effect of dextromethorphan (DXM) use in sensorineural hearing loss (SNHL) has not been fully examined. We conducted an animal model and nationwide retrospective matched-cohort study to explore the association between DXM use and SNHL. -
Print Your Symptom Diary
MEDICATION GUIDE FETZIMA® (fet-ZEE-muh) (levomilnacipran) extended-release capsules, for oral use What is the most important information I should know about FETZIMA? FETZIMA may cause serious side effects, including: • Increased risk of suicidal thoughts or actions in some children, adolescents, and young adults. FETZIMA and other antidepressant medicines may increase suicidal thoughts or actions in some children and young adults, especially within the first few months of treatment or when the dose is changed. FETZIMA is not for use in children. o Depression or other serious mental illnesses are the most important causes of suicidal thoughts or actions. Some people may have a higher risk of having suicidal thoughts or actions. These include people who have (or have a family history of) depression, bipolar illness (also called manic-depressive illness) or have a history of suicidal thoughts or actions. How can I watch for and try to prevent suicidal thoughts and actions? o Pay close attention to any changes, especially sudden changes in mood, behavior, thoughts, or feelings, or if you develop suicidal thoughts or actions. This is very important when an antidepressant medicine is started or when the dose is changed. o Call your healthcare provider right away to report new or sudden changes in mood, behavior, thoughts, or feelings. o Keep all follow-up visits with your healthcare provider as scheduled. Call your healthcare provider between visits as needed, especially if you have concerns about symptoms. Call your healthcare provider or -

Clinical Biochemistry of Hepatotoxicity
linica f C l To o x l ic a o n r l o u g Singh, J Clinic Toxicol 2011, S:4 o y J Journal of Clinical Toxicology DOI: 10.4172/2161-0495.S4-001 ISSN: 2161-0495 ReviewResearch Article Article OpenOpen Access Access Clinical Biochemistry of Hepatotoxicity Anita Singh1, Tej K Bhat2 and Om P Sharma2* 1CSK Himachal Pradesh, Krishi Vishva Vidyalaya, Palampur (HP) 176 062, India 2Biochemistry Laboratory, Indian Veterinary Research Institute, Regional Station, Palampur (HP) 176 061, India Abstract Liver plays a central role in the metabolism and excretion of xenobiotics which makes it highly susceptible to their adverse and toxic effects. Liver injury caused by various toxic chemicals or their reactive metabolites [hepatotoxicants) is known as hepatotoxicity. The present review describes the biotransformation of hepatotoxicants and various models used to study hepatotoxicity. It provides an overview of pathological and biochemical mechanism involved during hepatotoxicity together with alteration of clinical biochemistry during liver injury. The review has been supported by a list of important hepatotoxicants as well as common hepatoprotective herbs. Keywords: Hepatotoxicity; Hepatotoxicant; In Vivo models; In Vitro production of bile thus leading to the body’s inability to flush out the models; Pathology; Alanine aminotransferase; Alkaline phosphatase; chemicals through waste. Smooth endoplasmic reticulum of the liver is Bilirubin; Hepatoprotective the principal ‘metabolic clearing house’ for both endogenous chemicals like cholesterol, steroid hormones, fatty acids and proteins, and Introduction exogenous substances like drugs and alcohol. The central role played by liver in the clearance and transformation of chemicals exposes it to Hepatotoxicity refers to liver dysfunction or liver damage that is toxic injury [4]. -

Levomilnacipran (Fetzima®) Indication
Levomilnacipran (Fetzima®) Indication: Indicated for the treatment of major depressive disorder (MDD), FDA approved July 2013. Mechanism of action Levomilnacipran, the more active enantiomer of racemic milnacipran, is a selective SNRI with greater potency for inhibition of norepinephrine relative to serotonin reuptake Compared with duloxetine or venlafaxine, levomilnacipran has over 10-fold higher selectivity for norepinephrine relative to serotonin reuptake inhibition The exact mechanism of the antidepressant action of levomilnacipran is unknown Dosage and administration Initial: 20 mg once daily for 2 days and then increased to 40 mg once daily. The dosage can be increased by increments of 40 mg at intervals of two or more days Maintenance: 40-120 mg once daily with or without food. Fetzima should be swallowed whole (capsule should not be opened or crushed) Levomilnacipran and its metabolites are eliminated primarily by renal excretion o Renal impairment Dosing: Clcr 30-59 mL/minute: 80 mg once daily Clcr 15-29 mL/minute: 40 mg once daily End-stage renal disease (ESRD): Not recommended Discontinuing treatment: Gradually taper dose, if intolerable withdrawal symptoms occur, consider resuming the previous dose and/or decrease dose at a more gradual rate How supplied: Capsule ER 24 Hour Fetzima Titration: 20 & 40 mg (28 ea) Fetzima: 20 mg, 40 mg, 80 mg, 120 mg Warnings and Precautions Elevated Blood Pressure and Heart Rate: measure heart rate and blood pressure prior to initiating treatment and periodically throughout treatment Narrow-angle glaucoma: may cause mydriasis. Use caution in patients with controlled narrow- angle glaucoma Urinary hesitancy or retention: advise patient to report symptoms of urinary difficulty Discontinuation Syndrome Seizure disorders: Use caution with a previous seizure disorder (not systematically evaluated) Risk of Serotonin syndrome when taken alone or co-administered with other serotonergic agents (including triptans, tricyclics, fentanyl, lithium, tramadol, tryptophan, buspirone, and St. -

Levomilnacipran for the Treatment of Major Depressive Disorder
Out of the Pipeline Levomilnacipran for the treatment of major depressive disorder Matthew Macaluso, DO, Hala Kazanchi, MD, and Vikram Malhotra, MD An SNRI with n July 2013, the FDA approved levomil- Table 1 once-daily dosing, nacipran for the treatment of major de- Levomilnacipran: Fast facts levomilnacipran pressive disorder (MDD) in adults.1 It is I Brand name: Fetzima decreased core available in a once-daily, extended-release formulation (Table 1).1 The drug is the fifth Class: Serotonin-norepinephrine reuptake symptoms of inhibitor serotonin-norepinephrine reuptake inhibi- MDD and was well Indication: Treatment of major depressive tor (SNRI) to be sold in the United States disorder in adults tolerated in clinical and the fourth to receive FDA approval for FDA approval date: July 26, 2013 trials treating MDD. Availability date: Fourth quarter of 2013 Levomilnacipran is believed to be the Manufacturer: Forest Pharmaceuticals more active enantiomer of milnacipran, Dosage forms: Extended–release capsules in which has been available in Europe for 20 mg, 40 mg, 80 mg, and 120 mg strengths years and was approved by the FDA in Recommended dosage: 40 mg to 120 mg 2009 for treating fibromyalgia. Efficacy of capsule once daily with or without food levomilnacipran for treating patients with Source: Reference 1 MDD was established in three 8-week ran- domized controlled trials (RCTs).1 cial and occupational functioning in addi- Clinical implications tion to improvement in the core symptoms Levomilnacipran is indicated for treating of depression.5 -

Premium Non-Specialty Quantity Limit List January 2016
Premium Non-Specialty Quantity Limit List January 2016 Therapeutic Category Drug Name Dispensing Limit Anti-infectives Antibiotics DIFICID (fidaxomicin) 200 mg 2 tabs/day & 10 days/30 days SIVEXTRO (tedizolid) Solr 6 vials/30 days SIVEXTRO (tedizolid) Tabs 6 tabs/30 days ZYVOX (linezolid) 28 tabs/30 days ZYVOX (linezolid) Suspension 4 bottles (600 mL)/28 days Antifungals LAMISIL (terbinafine) 250 mg 84 days supply/180 days Antimalarial QUALAQUIN (quinine) QL varies* Antivirals, Herpetic FAMVIR (famciclovir) 125 mg 1 tab/day FAMVIR (famciclovir) 250 mg 2 tabs/day FAMVIR (famciclovir) 500 mg 21 tabs/30 days SITAVIG (acyclovir) 50 mg 2 tabs/30 days VALTREX (valacyclovir) 1000 mg 3 tabs/day VALTREX (valacyclovir) 500 mg 2 tabs/day Antivirals, Influenza RELENZA (zanamivir) QL is 40 inh per 365 days. TAMIFLU (oseltamivir) 30 mg 40 caps per 365 days TAMIFLU (oseltamivir) 45 mg, 75 mg 20 caps per 365 days TAMIFLU (oseltamivir) Suspension 360 mL/365 days Cardiology Anticoagulants ELIQUIS (apixiban) 2 tabs/day ELIQUIS (apixiban) 5 mg 3 tabs/day IPRIVASK (desirudin) 35 days supply/180 days PRADAXA (dabigatran) 2 caps/day SAVAYSA (edoxaban) 1 tab/day XARELTO (rivaroxaban) 10 mg 35 days supply/180 days XARELTO (rivaroxaban) 15 mg 2 tabs/day XARELTO (rivaroxaban) 20 mg 1 tab/day XARELTO (rivaroxaban) Starter Pack 2 starter packs/year Heart Failure CORLANOR (ivabradine) 2 tabs/day Central Nervous System ADHD Agents ADDERALL (amphetamine/dextroamphetamine) 3 tabs/day ADDERALL XR (amphetamine/dextroamphetamine mixed salts) 1 cap/day APTENSIO XR (methylphenidate) -
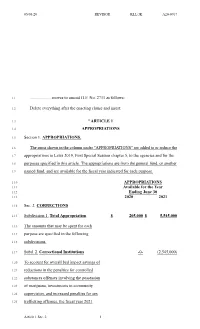
Moves to Amend HF No. 2711 As Follows
05/05/20 REVISOR KLL/JK A20-0767 1.1 .................... moves to amend H.F. No. 2711 as follows: 1.2 Delete everything after the enacting clause and insert: 1.3 "ARTICLE 1 1.4 APPROPRIATIONS 1.5 Section 1. APPROPRIATIONS. 1.6 The sums shown in the column under "APPROPRIATIONS" are added to or reduce the 1.7 appropriations in Laws 2019, First Special Session chapter 5, to the agencies and for the 1.8 purposes specified in this article. The appropriations are from the general fund, or another 1.9 named fund, and are available for the fiscal year indicated for each purpose. 1.10 APPROPRIATIONS 1.11 Available for the Year 1.12 Ending June 30 1.13 2020 2021 1.14 Sec. 2. CORRECTIONS 1.15 Subdivision 1. Total Appropriation $ 205,000 $ 5,545,000 1.16 The amounts that may be spent for each 1.17 purpose are specified in the following 1.18 subdivisions. 1.19 Subd. 2. Correctional Institutions -0- (2,545,000) 1.20 To account for overall bed impact savings of 1.21 reductions in the penalties for controlled 1.22 substances offenses involving the possession 1.23 of marijuana, investments in community 1.24 supervision, and increased penalties for sex 1.25 trafficking offenses, the fiscal year 2021 Article 1 Sec. 2. 1 05/05/20 REVISOR KLL/JK A20-0767 2.1 appropriation from Laws 2019, First Special 2.2 Session chapter 5, article 1, section 15, 2.3 subdivision 2, is reduced by $2,545,000. 2.4 Subd. -

Hallucinogens
Hallucinogens What are hallucinogens? Hallucinogens are a diverse group of drugs that alter a person’s awareness of their surroundings as well as their own thoughts and feelings. They are commonly split into two categories: classic hallucinogens (such as LSD) and dissociative drugs (such as PCP). Both types of hallucinogens can cause hallucinations, or sensations and images that seem real though they are not. Additionally, dissociative drugs can cause users to feel out of control or disconnected from their body and environment. Some hallucinogens are extracted from plants or mushrooms, and some are synthetic (human- made). Historically, people have used hallucinogens for religious or healing rituals. More recently, people report using these drugs for social or recreational purposes, including to have fun, deal with stress, have spiritual experiences, or just to feel different. Common classic hallucinogens include the following: • LSD (D-lysergic acid diethylamide) is one of the most powerful mind-altering chemicals. It is a clear or white odorless material made from lysergic acid, which is found in a fungus that grows on rye and other grains. LSD has many other street names, including acid, blotter acid, dots, and mellow yellow. • Psilocybin (4-phosphoryloxy-N,N- dimethyltryptamine) comes from certain types of mushrooms found in tropical and subtropical regions of South America, Mexico, and the United States. Some common names for Blotter sheet of LSD-soaked paper squares that users psilocybin include little smoke, magic put in their mouths. mushrooms, and shrooms. Photo by © DEA • Peyote (mescaline) is a small, spineless cactus with mescaline as its main ingredient. Peyote can also be synthetic. -
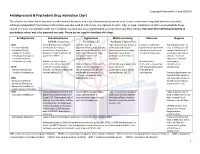
Antidepressant & Psychedelic Drug Interaction Chart
Copyright Psychedelic School 8/2020 Antidepressant & Psychedelic Drug Interaction Chart This chart is not intended to be used to make medical decisions and is for informational purposes only. It was constructed using data whenever possible, although extrapolation from known information was also used to inform risk. Any decision to start, stop, or taper medication and/or use psychedelic drugs should be made in conjunction with your healthcare provider(s). It is recommended to not perform any illicit activity. This chart the intellectual property of psychedelic school and is for personal use only. Please do not copy or distribute this chart. Antidepressant Phenethylamines Tryptamines MAOI-containing Ketamine Ibogaine -MDMA, mescaline -Psilocybin, LSD -Ayahuasca, Syrian Rue SSRIs Taper & discontinue at least 2 Consider taper & Taper & discontinue at least 2 Has been studied and Taper & discontinue at · Paroxetine (Paxil) weeks prior (all except discontinuation at least 2 weeks weeks prior (all except found effective both with least 2 weeks prior (all · Sertraline (Zoloft) fluoxetine) or 6 weeks prior prior (all except fluoxetine) or 6 fluoxetine) or 6 weeks prior and without concurrent except fluoxetine) or 6 · Citalopram (Celexa) (fluoxetine only) due to loss of weeks prior (fluoxetine only) (fluoxetine only) due to use of antidepressants weeks prior (fluoxetine · Escitalopram (Lexapro) psychedelic effect due to potential loss of potential risk of serotonin only) due to risk of · Fluxoetine (Prozac) psychedelic effect syndrome additive QTc interval · Fluvoxamine (Luvox) MDMA is unable to cause Recommended prolongation, release of serotonin when the Chronic antidepressant use may Life threatening toxicities can to be used in conjunction arrhythmias, or SPARI serotonin reuptake pump is result in down-regulation of occur with these with oral antidepressants cardiotoxicity · Vibryyd (Vilazodone) blocked. -

Janssen Research & Development, LLC Advisory Committee Briefing
Janssen Research & Development, LLC Advisory Committee Briefing Document Esketamine Nasal Spray for Patients with Treatment-resistant Depression JNJ-54135419 (esketamine) Status: Approved Date: 16 January 2019 Prepared by: Janssen Research & Development, LLC EDMS number: EDMS-ERI-171521650, 1.0 ADVISORY COMMITTEE BRIEFING MATERIALS: AVAILABLE FOR PUBLIC RELEASE 1 Status: Approved, Date: 16 January 2019 JNJ-54135419 (esketamine) Treatment-resistant Depression Advisory Committee Briefing Document GUIDE FOR REVIEWERS This briefing document provides 3 levels of review with increasing levels of detail: The Executive Overview (Section 1, starting on page 11) provides a narrative summarizing the disease, need for novel treatments, key development program characteristics for esketamine nasal spray, study results, and conclusions. References are made to the respective supporting sections in the core document. The core document (Section 2 to Section 11, starting on page 30) includes detailed summaries and discussion in support of the Executive Overview. The appendices (starting on page 180) provide additional or more detailed information to complement brief descriptions provided in sections of the core document (e.g., demographic and baseline characteristics of the study populations, additional efficacy analyses in the Phase 3 studies, statistical methods). These appendices are referenced in the core document when relevant. This review structure allows review at varying levels of detail; however, reviewers who read at multiple levels will necessarily -

6) Hepatotoxic Drugs
ILOs § Define the role of liver in drug detoxification § Discuss the types (patterns) of hepatotoxicity § Classify hepatotoxins § Explain how a drug can inflict hepatotoxicity § State the pathological consequences of hepatic injury § Contrast the various clinical presentation of hepatotoxicity § Enlist the possible treatment PHYSIOLOGICAL has multiple functions (>5000) è can be categorized into: 1. Regulation, synthesis & secretion. èutilization of glucose, lipids & proteins + bile for digesting fats. 2. Storage. è Glucose (as glycogen), fat soluble vitamins (A, D, E & K) & minerals 3. Purification, transformation & clearance è of endogenous (steroid hormones, cholesterol, FA, & proteins..) & exogenous (drugs, toxins, herbs…etc ) chemicals. Human body identifies almost all drugs as foreign substances i.e. XENOBIOTIC Has to get rid of them "METABOLIC CLEARING HOUSE" PHARMACOLOGICAL HEPATOTOXIC DRUGS Subjects drugs to chemical transformation (METABOLISM) è to become inactive & easily excreted. Since most drugs are lipophilic è they are changed into hydrophilic water soluble products è suitable for elimination through the bile or urine Such metabolic transformation usually occur in 2 PHASES: Phase 1 reactions Yields intermediates è Oxidation, Reduction, polar, transient, usually highly reactive è Hydrolysis, Hydration far more toxic than parent substrates è Catalyzed by CYT P-450 may result in liver injury Drug-Induced Liver Injury (DILI) Phase 2 reactions Yields products of increased solubility Conjugation with a moiety If of high molecular weight è (acetate, a.a., glutathione, excreted in bile glucuronic a., sulfate ) If of low molecular weight è to blood è excreted in urine Hepatotoxicity è Is the Leading cause of ADRs Injury / damage of the liver è Caused by exposure to a drug è Inflict varying impairment in liver functions è Manifests clinically a long range è hepatitis ðfailure Inflammation ðApoptosis ð Necrosis Why the liver is the major site of ADRs ? It is the first organ to come in contact with the drug after absorption from the GIT. -

Drug and Alcohol Induced Hepatotoxicity
From The Department of Physiology and Pharmacology, Section of Pharmacogenetics Karolinska Institutet, Stockholm, Sweden DRUG AND ALCOHOL INDUCED HEPATOTOXICITY Angelica Butura Stockholm 2008 All previously published papers were reproduced with permission from the publisher. Published by Karolinska Institutet. © Angelica Butura, 2008 ISBN 978-91-7409-055-0 To my parents for always believing in me ABSTRACT Drug induced hepatotoxicity is the most common reason cited for withdrawal of already approved drugs from the market and accounts for more than 50 percent of cases of acute liver failure in the United States. Ethanol (EtOH) causes a further substantial amount of liver insufficiencies world wide. The current thesis was focused on the mechanisms behind hepatotoxicity caused by these agents. Using a rat in vivo model for alcoholic liver disease (ALD) it was found that cytokine and chemokine levels in blood accompanied the fluctuating levels of blood EtOH, indicating that they are directly influenced by absolute EtOH concentration. During the early phases of ALD in this model, a strong initial Th1 response was observed as revealed by increased levels of cytokine as well as transcription factor mRNAs, followed by a downregulation, whereas Th2 response was decreased by EtOH over the entire treatment period of four weeks. We found that supplementation with the antioxidant NAC to ethanol treated animals decreases severity of liver damage and somewhat decreases initial inflammatory response mediated by TNFα. NAC also diminished the ethanol-induced formation of protein adducts of lipid peroxidation products like MDA and HNE. Also, the formation of antibodies against neo-antigens formed by MDA, HNE and HER protein adducts was lowered.