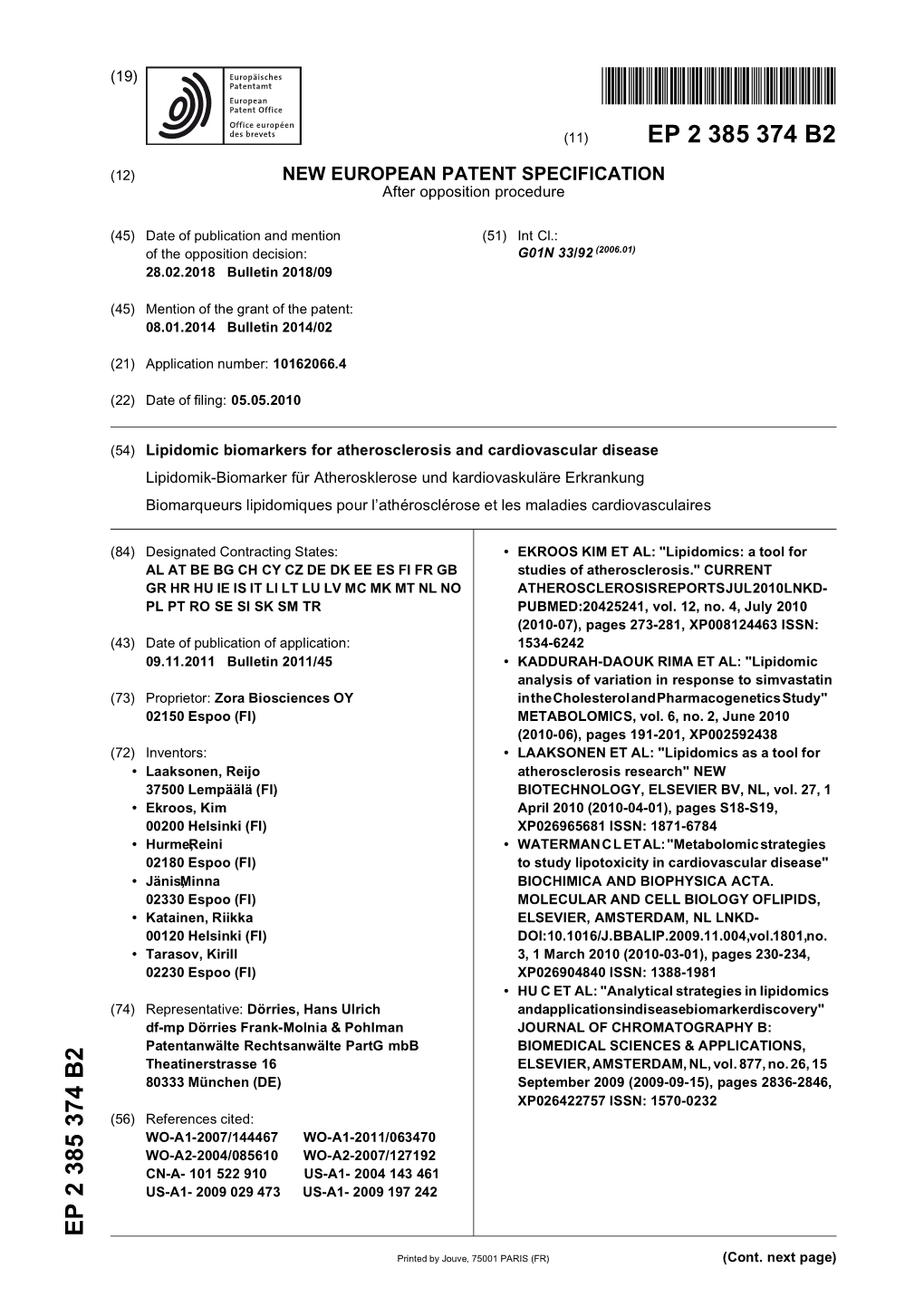
Lipidomic Biomarkers for Atherosclerosis and Cardiovascular Disease
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Prevention of Coronary Heart Disease
PREVENTION OF CORONARY PATIENT WITH CHD HEART DISEASE • Obese male patient with previous angina, cardiac catheterization with placement of two stents and now stable. • Notable clinical characteristics: Thomas F . Wh ayne, J r, MD , PhD, FACC Triglycerides 354 mg/dl. Professor of Medicine (Cardiology) HDL 28 mg/dl in men. Gill Heart Institute BP 140/90 mm/Hg. University of Kentucky Fasting glucose 120 mg/dl. November, 2009 • Specific management? Characteristics of Plaques Prone to HIGH SENSENSITIVITY Rupture From Inflammation and LDL CREACTIVE PROTEIN (hs-CRP) Fibrous cap Media • A MARKER OF INFLAMMATION: CRP AND Lumen Lipid hsCRP ARE SAME PROTEIN Core • MAY BE ANOTHER RISK FACTOR AND PLAY A ROLE IN PLAQUE FORMATION “Vulnerable” plaque • MAY PREDICT HIGH RISK ACUTE CORONARY SYNDROME • MAY INDICATE PATIENTS MOST LIKELY TO Lumen RESPOND TO STATINS T lymphocyte Lipid • STATINS SHOWN TO REDUCE CRP Core Macrophage foam cell (tissue factor) “Activated” Intimal SMC (HLA-DR+) – EZETIMIBE ACCENTUATES THIS EFFECT* “Stable” plaque Normal medial SMC • NEED STATIN DOSE RESPONSE CURVE Libby P. Circulation. 1999; 91:284491:2844--2850.2850. *Sager PT, et al. Am J Cardiol. 2003;92:1414-1418. Resultados Estudio VYTAL sobre PCR: Ezetimiba/Simvastatina vs. Atorvastatina en pts con DM II e Hipercolesterolemia (n=1229) CURRENT CLINICALLY USEFUL MARKERS OF INFLAMMATION Atorvastatina E/Simvas Atorvas E/S 10 mg 20 mg 10/20 40 mg 10/40 0 • LIPOPROTEIN-ASSOCIATED Ezetimiba/ --55 Simvastatina PHOSPHOLIPASE A2*. Atorvastatina ® asales --1010 a Sensibilidad – PLAC TEST. t b --1515 --13.713.7 de Al --13.813.8 • HIGH SENSITIVITY C-REACTIVE --2020 # PCR PROTEIN (hsCRP) . -

1 CETP Inhibition Improves HDL Function but Leads to Fatty Liver and Insulin Resistance in CETP-Expressing Transgenic Mice on A
Page 1 of 55 Diabetes CETP inhibition improves HDL function but leads to fatty liver and insulin resistance in CETP-expressing transgenic mice on a high-fat diet Lin Zhu1,2, Thao Luu2, Christopher H. Emfinger1,2, Bryan A Parks5, Jeanne Shi2,7, Elijah Trefts3, Fenghua Zeng4, Zsuzsanna Kuklenyik5, Raymond C. Harris4, David H. Wasserman3, Sergio Fazio6 and John M. Stafford1,2,3,* 1VA Tennessee Valley Healthcare System, 2Division of Diabetes, Endocrinology, & Metabolism, 3Department of Molecular Physiology and Biophysics, 4Devision of Nephrology and Hypertension, Vanderbilt University School of Medicine. 5Division of Laboratory Sciences, Centers for Disease Control and Prevention. 6The Center for Preventive Cardiology at the Knight Cardiovascular Institute, Oregon Health & Science University. 7Trinity College of Art and Science, Duke University. * Address correspondence and request for reprints to: John. M. Stafford, 7445D Medical Research Building IV, Nashville, TN 37232-0475, phone (615) 936-6113, fax (615) 936- 1667 Email: [email protected] Running Title: CETP inhibition and insulin resistance Word Count: 5439 Figures: 7 Tables: 1 1 Diabetes Publish Ahead of Print, published online September 13, 2018 Diabetes Page 2 of 55 Abstract In clinical trials inhibition of cholesteryl ester transfer protein (CETP) raises HDL cholesterol levels but doesn’t robustly improve cardiovascular outcomes. About 2/3 of trial participants were obese. Lower plasma CETP activity is associated with increased cardiovascular risk in human studies, and protective aspects of CETP have been observed in mice fed a high-fat diet (HFD) with regard to metabolic outcomes. To define if CETP inhibition has different effects depending on the presence of obesity, we performed short- term anacetrapib treatment in chow- and HFD-fed CETP-transgenic mice. -

PHARMACEUTICAL APPENDIX to the TARIFF SCHEDULE 2 Table 1
Harmonized Tariff Schedule of the United States (2020) Revision 19 Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2020) Revision 19 Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 2 Table 1. This table enumerates products described by International Non-proprietary Names INN which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service CAS registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. -

Dysfunctional High-Density Lipoproteins in Type 2 Diabetes Mellitus: Molecular Mechanisms and Therapeutic Implications
Journal of Clinical Medicine Review Dysfunctional High-Density Lipoproteins in Type 2 Diabetes Mellitus: Molecular Mechanisms and Therapeutic Implications Isabella Bonilha 1 , Francesca Zimetti 2,* , Ilaria Zanotti 2 , Bianca Papotti 2 and Andrei C. Sposito 1,* 1 Atherosclerosis and Vascular Biology Laboratory (AtheroLab), Cardiology Department, State University of Campinas (Unicamp), Campinas 13084-971, Brazil; [email protected] 2 Department of Food and Drug, University of Parma, 43124 Parma, Italy; [email protected] (I.Z.); [email protected] (B.P.) * Correspondence: [email protected] (F.Z.); [email protected] (A.C.S.); Tel.: +39-05-2190-6172 (F.Z.); +55-19-3521-7098 (A.C.S.); Fax: +55-1-9328-9410 (A.C.S.) Abstract: High density lipoproteins (HDLs) are commonly known for their anti-atherogenic prop- erties that include functions such as the promotion of cholesterol efflux and reverse cholesterol transport, as well as antioxidant and anti-inflammatory activities. However, because of some chronic inflammatory diseases, such as type 2 diabetes mellitus (T2DM), significant changes occur in HDLs in terms of both structure and composition. These alterations lead to the loss of HDLs’ physiological functions, to transformation into dysfunctional lipoproteins, and to increased risk of cardiovascular disease (CVD). In this review, we describe the main HDL structural/functional alterations observed in T2DM and the molecular mechanisms involved in these T2DM-derived modifications. Finally, the main available therapeutic interventions targeting HDL in diabetes are discussed. Citation: Bonilha, I.; Zimetti, F.; Keywords: high density lipoprotein; type 2 diabetes mellitus; HDL function; glycation; oxidation; Zanotti, I.; Papotti, B.; Sposito, A.C. -

Patent Application Publication ( 10 ) Pub . No . : US 2019 / 0192440 A1
US 20190192440A1 (19 ) United States (12 ) Patent Application Publication ( 10) Pub . No. : US 2019 /0192440 A1 LI (43 ) Pub . Date : Jun . 27 , 2019 ( 54 ) ORAL DRUG DOSAGE FORM COMPRISING Publication Classification DRUG IN THE FORM OF NANOPARTICLES (51 ) Int . CI. A61K 9 / 20 (2006 .01 ) ( 71 ) Applicant: Triastek , Inc. , Nanjing ( CN ) A61K 9 /00 ( 2006 . 01) A61K 31/ 192 ( 2006 .01 ) (72 ) Inventor : Xiaoling LI , Dublin , CA (US ) A61K 9 / 24 ( 2006 .01 ) ( 52 ) U . S . CI. ( 21 ) Appl. No. : 16 /289 ,499 CPC . .. .. A61K 9 /2031 (2013 . 01 ) ; A61K 9 /0065 ( 22 ) Filed : Feb . 28 , 2019 (2013 .01 ) ; A61K 9 / 209 ( 2013 .01 ) ; A61K 9 /2027 ( 2013 .01 ) ; A61K 31/ 192 ( 2013. 01 ) ; Related U . S . Application Data A61K 9 /2072 ( 2013 .01 ) (63 ) Continuation of application No. 16 /028 ,305 , filed on Jul. 5 , 2018 , now Pat . No . 10 , 258 ,575 , which is a (57 ) ABSTRACT continuation of application No . 15 / 173 ,596 , filed on The present disclosure provides a stable solid pharmaceuti Jun . 3 , 2016 . cal dosage form for oral administration . The dosage form (60 ) Provisional application No . 62 /313 ,092 , filed on Mar. includes a substrate that forms at least one compartment and 24 , 2016 , provisional application No . 62 / 296 , 087 , a drug content loaded into the compartment. The dosage filed on Feb . 17 , 2016 , provisional application No . form is so designed that the active pharmaceutical ingredient 62 / 170, 645 , filed on Jun . 3 , 2015 . of the drug content is released in a controlled manner. Patent Application Publication Jun . 27 , 2019 Sheet 1 of 20 US 2019 /0192440 A1 FIG . -

Pharmacogenomics Variability of Lipid-Lowering Therapies in Familial Hypercholesterolemia
Journal of Personalized Medicine Review Pharmacogenomics Variability of Lipid-Lowering Therapies in Familial Hypercholesterolemia Nagham N. Hindi 1,†, Jamil Alenbawi 1,† and Georges Nemer 1,2,* 1 Division of Genomics and Translational Biomedicine, College of Health and Life Sciences, Hamad Bin Khalifa University, Doha P.O. Box 34110, Qatar; [email protected] (N.N.H.); [email protected] (J.A.) 2 Department of Biochemistry and Molecular Genetics, Faculty of Medicine, American University of Beirut, Beirut DTS-434, Lebanon * Correspondence: [email protected]; Tel.: +974-445-41330 † Those authors contributed equally to the work. Abstract: The exponential expansion of genomic data coupled with the lack of appropriate clinical categorization of the variants is posing a major challenge to conventional medications for many common and rare diseases. To narrow this gap and achieve the goals of personalized medicine, a collaborative effort should be made to characterize the genomic variants functionally and clinically with a massive global genomic sequencing of “healthy” subjects from several ethnicities. Familial- based clustered diseases with homogenous genetic backgrounds are amongst the most beneficial tools to help address this challenge. This review will discuss the diagnosis, management, and clinical monitoring of familial hypercholesterolemia patients from a wide angle to cover both the genetic mutations underlying the phenotype, and the pharmacogenomic traits unveiled by the conventional and novel therapeutic approaches. Achieving a drug-related interactive genomic map will potentially benefit populations at risk across the globe who suffer from dyslipidemia. Citation: Hindi, N.N.; Alenbawi, J.; Nemer, G. Pharmacogenomics Variability of Lipid-Lowering Keywords: familial hypercholesterolemia; pharmacogenomics; PCSK9 inhibitors; statins; ezetimibe; Therapies in Familial novel lipid-lowering therapy Hypercholesterolemia. -

Articles Article: Non-Statin Treatments for Managing LDL Cholesterol and Their Outcomes Download
Clinical Therapeutics/Volume 37, Number 12, 2015 Review Article Non-statin Treatments for Managing LDL Cholesterol and Their Outcomes Traci Turner, MD; and Evan A. Stein, MD, PhD Metabolic & Atherosclerosis Research Center, Cincinnati, Ohio ABSTRACT agents are being developed as orphan indications ex- Purpose: Over the past 3 decades reducing LDL-C pressly for patients with homozygous familial hyper- has proven to be the most reliable and easily achiev- cholesterolemia, including peroxisome proliferator able modifiable risk factor to decrease the rate of activated receptor-δ agonists, angiopoietin-like protein 3 cardiovascular morbidity and mortality. Statins are inhibitors, and gene therapy. effective, but problems with their side effects, adher- Implications: Monoclonal antibodies that inhibit ence, or LDL-C efficacy in some patient groups PCSK9 were shown to be very effective reducers of remain. Most currently available alternative lipid- LDL-C and well tolerated despite subcutaneous ad- modifying therapies have limited efficacy or tolerabil- ministration, and no significant safety issues have yet ity, and additional effective pharmacologic modalities emerged during large Phase II and III trials. They have to reduce LDL-C are needed. the potential to substantially impact further the risk of Methods: Recent literature on new and evolving cardiovascular disease. A number of additional new, LDL-C–lowering modalities in preclinical and clinical but less effective, oral LDL-C–lowering agents are development was reviewed. also in various stages of development, including Findings: Several new therapies targeting LDL-C are some which are targeted only to patients with homo- in development. Inhibition of proprotein convertase sub- zygous familial hypercholesterolemia. (Clin Ther. -

2 12/ 35 74Al
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date 22 March 2012 (22.03.2012) 2 12/ 35 74 Al (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 9/16 (2006.01) A61K 9/51 (2006.01) kind of national protection available): AE, AG, AL, AM, A61K 9/14 (2006.01) AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, (21) International Application Number: DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, PCT/EP201 1/065959 HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, (22) International Filing Date: KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, 14 September 201 1 (14.09.201 1) ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PE, PG, PH, PL, PT, QA, RO, RS, RU, (25) Filing Language: English RW, SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, (26) Publication Language: English TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (30) Priority Data: 61/382,653 14 September 2010 (14.09.2010) US (84) Designated States (unless otherwise indicated, for every kind of regional protection available): ARIPO (BW, GH, (71) Applicant (for all designated States except US): GM, KE, LR, LS, MW, MZ, NA, SD, SL, SZ, TZ, UG, NANOLOGICA AB [SE/SE]; P.O Box 8182, S-104 20 ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, MD, RU, TJ, Stockholm (SE). -

High-Density Lipoproteins in the Prevention of Cardiovascular Disease: Changing the Paradigm
State of the Art STATE ART nature publishing group High-Density Lipoproteins in the Prevention of Cardiovascular Disease: Changing the Paradigm S Tuteja1 and DJ Rader1 High-density-lipoprotein cholesterol (HDL-C) has been identified in population studies as an independent inverse predictor of cardiovascular events. Although the causal nature of this association has been questioned, HDL and its major protein, apolipoprotein (apo)A1, have been shown to prevent and reverse atherosclerosis in animal models. In addition, HDL and apoA1 have several putatively atheroprotective functions, such as the ability to promote efflux of cholesterol from macrophages in the artery wall, inhibit vascular inflammation, and enhance endothelial function. Therefore, HDL-C and apoA1 have been investigated as therapeutic targets for coronary heart disease. However, recent clinical trials with drugs that raise HDL-C, such as niacin and inhibitors of cholesteryl ester transfer protein, have been disappointing. Here, we review the current state of the science regarding HDL as a therapeutic target. Advances in the treatment of hypercholesterolemia, primarily increase HDL-C will prevent the occurrence of CHD.10 Te with statins, are responsible for the decline in mortality due to Veterans Afairs HDL Intervention Trial was one of the frst pro- coronary heart disease (CHD); however, CHD is still the cause spective studies to demonstrate that a therapy that increased lev- of death for one in six Americans.1 Low-density-lipoprotein els of HDL-C, gemfbrozil, reduced major -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -

Study Protocol 1002-039 Amendment 1, 05 March 2017
1. TITLE PAGE BEMPEDOIC ACID (ETC-1002) 1002-039 A RANDOMIZED, DOUBLE-BLIND, PARALLEL GROUP, MULTICENTER STUDY TO EVALUATE THE EFFICACY AND SAFETY OF BEMPEDOIC ACID (ETC-1002) 180 MG QD WHEN ADDED TO PROPROTEIN CONVERTASE SUBTILISIN/KEXIN TYPE 9 (PCSK9)-INHIBITOR THERAPY Study Phase: 2 IND Number: 106,654 EudraCT Number: n/a Indication: Treatment of hyperlipidemia Investigators: Approximately 20-30 sites located in North America Sponsor: Esperion Therapeutics, Inc. 3891 Ranchero Drive, Suite 150 Ann Arbor, MI 48108 Phone: 734-862-4840 Fax: 734-582-9720 Sponsor Contact: Medical Monitor: Version Date Original Protocol 22 November 2016 Protocol Amendment 1: 05 March 2017 Confidentiality Statement THIS CONFIDENTIAL INFORMATION IS ABOUT AN INVESTIGATIONAL DRUG PROVIDED FOR THE EXCLUSIVE USE OF INVESTIGATORS OF THIS DRUG AND IS SUBJECT TO RECALL AT ANY TIME. THE INFORMATION IN THIS DOCUMENT MAY NOT BE DISCLOSED UNLESS SUCH DISCLOSURE IS REQUIRED BY FEDERAL OR STATE LAW OR REGULATIONS. SUBJECT TO THE FOREGOING, THIS INFORMATION MAY BE DISCLOSED ONLY TO THOSE PERSONS INVOLVED IN THE STUDY WHO HAVE NEED TO KNOW, WITH THE OBLIGATION NOT TO FURTHER DISSEMINATE THIS INFORMATION. THESE RESTRICTIONS ON DISCLOSURE WILL APPLY EQUALLY TO ALL FUTURE ORAL OR WRITTEN INFORMATION, SUPPLIED TO YOU BY ESPERION THERAPEUTICS, INC., WHICH IS DESIGNATED AS “PRIVILEGED” OR “CONFIDENTIAL.” NCT number: NCT03193047 This NCT number has been applied to the document for purposes of posting on clinicaltrials.gov Confidential Page 1 of 114 Bempedoic Acid Esperion Therapeutics, Inc. Clinical Study Protocol 1002-039 Amendment 1, 05 March 2017 2. SYNOPSIS Name of Sponsor: Esperion Therapeutics, Inc. -

Ep 2838891 B1
(19) TZZ ¥__T (11) EP 2 838 891 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: C07D 333/60 (2006.01) C07D 407/14 (2006.01) 02.08.2017 Bulletin 2017/31 C07D 417/12 (2006.01) C07D 495/04 (2006.01) C07D 307/82 (2006.01) A61K 31/381 (2006.01) (2006.01) (2006.01) (21) Application number: 13710076.4 A61K 31/343 A61K 31/4355 A61K 31/4365 (2006.01) A61P 3/04 (2006.01) (22) Date of filing: 22.02.2013 (86) International application number: PCT/JP2013/055605 (87) International publication number: WO 2013/125732 (29.08.2013 Gazette 2013/35) (54) AROMATIC RING COMPOUND AS GHRELIN O-ACYLTRANSFERASE INHIBITOR AROMATISCHE RINGVERBINDUNG ALS GHRELIN O-ACYLTRANSFERASE HEMMER COMPOSÉ À NOYAU AROMATIQUE COMME INHIBITEURS DE GHRéLINE O-ACYL TRANSFéRASE (84) Designated Contracting States: • KITAMURA, Shuji AL AT BE BG CH CY CZ DE DK EE ES FI FR GB Fujisawa-shi GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO Kanagawa 251-0012 (JP) PL PT RO RS SE SI SK SM TR • TOMATA, Yoshihide Fujisawa-shi (30) Priority: 24.02.2012 US 201261602888 P Kanagawa 251-0012 (JP) • YASUMA, Tsuneo (43) Date of publication of application: Osaka-shi 25.02.2015 Bulletin 2015/09 Osaka 532-0024 (JP) • IKOMA, Minoru (73) Proprietor: Takeda Pharmaceutical Company Fujisawa-shi Limited Kanagawa 251-0012 (JP) Osaka-shi, Osaka 541-0045 (JP) • MASUDA, Kei Fujisawa-shi (72) Inventors: Kanagawa 251-0012 (JP) • TAKAKURA, Nobuyuki Fujisawa-shi (74) Representative: Held, Stephan et al Kanagawa 251-0012 (JP) Meissner Bolte Patentanwälte