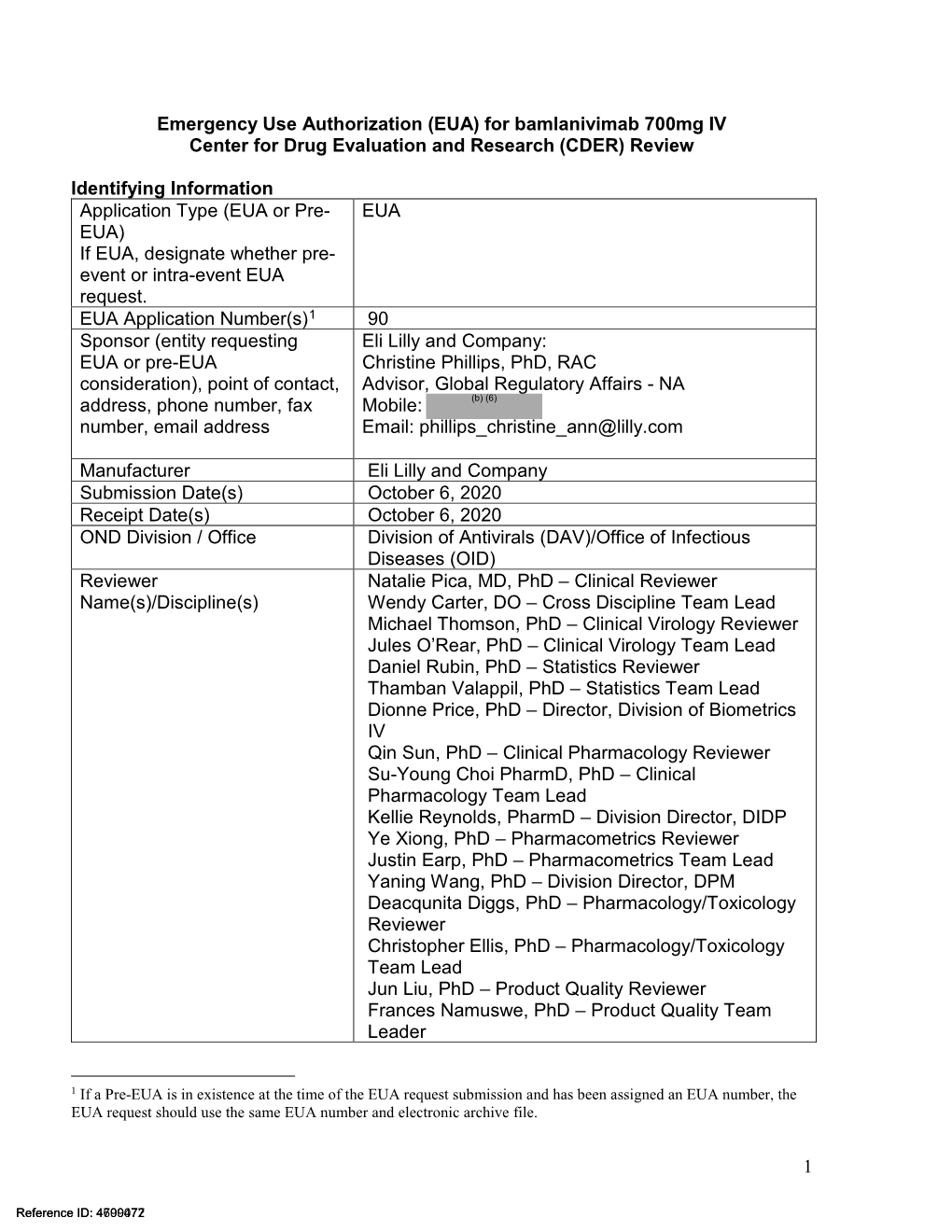
Emergency Use Authorization (EUA) for Bamlanivimab 700Mg IV Center for Drug Evaluation and Research (CDER) Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Emergency Use Authorization (EUA) for Bamlanivimab 700 Mg and Etesevimab 1400 Mg IV Administered Together Center for Drug Evaluation and Research (CDER) Review
________________________________________________________________ Emergency Use Authorization (EUA) for Bamlanivimab 700 mg and Etesevimab 1400 mg IV Administered Together Center for Drug Evaluation and Research (CDER) Review Identifying Information Application Type (EUA or Pre-EUA) EUA If EUA, designate whether pre-event or intra-event EUA request. 1 EUA Application Number(s) EUA 000094 Sponsor (entity requesting EUA or Eli Lilly and Company pre-EUA consideration), point of Christine Phillips, PhD, RAC contact, address, phone number, fax Advisor, Global Regulatory Affairs - NA (b) (6) number, email address Mobile: Email: [email protected] Manufacturer, if different from Eli Lilly and Company Sponsor Submission Date(s) November 16, 2020 Receipt Date(s) November 16, 2020 OND Division / Office Division of Antivirals/Office of Infectious Diseases Reviewer Name(s)/Discipline(s) Natalie Pica, MD, PhD – Clinical Reviewer Wendy Carter, DO – Cross Discipline Team Lead Michael Thomson, PhD – Clinical Virology Reviewer Jules O’Rear, PhD – Clinical Virology Team Lead Daniel Rubin, PhD – Statistics Reviewer Thamban Valappil, PhD – Statistics Team Lead Dionne Price, PhD – Director, Division of Biometrics IV Jason Moore, PharmD – Clinical Pharmacology Reviewer Su-Young Choi PharmD, PhD – Clinical Pharmacology Team Lead Kellie Reynolds, PharmD – Division Director, DIDP Ye Xiong, PhD – Pharmacometrics Reviewer Justin Earp, PhD – Pharmacometrics Team Lead Yaning Wang, PhD – Division Director, DPM 1 If a Pre-EUA is in existence at the time -
Hierarchical Mechanistic Modelling of Clinical Pharmacokinetic Data
Hierarchical mechanistic modelling of clinical pharmacokinetic data A thesis submitted to the University of Manchester for the degree of Doctor of Philosophy in the Faculty of Medical and Human Sciences 2015 Thierry Wendling Manchester Pharmacy School Contents List of Figures ........................................................................................................ 6 List of Tables .......................................................................................................... 9 List of abbreviations ............................................................................................ 10 Abstract ................................................................................................................ 13 Declaration ........................................................................................................... 14 Copyright ............................................................................................................. 14 Acknowledgements .............................................................................................. 15 Chapter 1: General introduction ...................................................................... 16 1.1. Modelling and simulation in drug development ........................................ 17 1.1.1. The drug development process .......................................................... 17 1.1.2. The role of pharmacokinetic and pharmacodynamic modelling in drug development .................................................................................................. -

Application of Pharmacometric Methods to Improve Pediatric Drug Development
Virginia Commonwealth University VCU Scholars Compass Theses and Dissertations Graduate School 2011 Application of Pharmacometric Methods to Improve Pediatric Drug Development Mallika Lala Virginia Commonwealth University Follow this and additional works at: https://scholarscompass.vcu.edu/etd Part of the Pharmacy and Pharmaceutical Sciences Commons © The Author Downloaded from https://scholarscompass.vcu.edu/etd/2467 This Dissertation is brought to you for free and open access by the Graduate School at VCU Scholars Compass. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of VCU Scholars Compass. For more information, please contact [email protected]. School of Pharmacy Virginia Commonwealth University This is to certify that the dissertation prepared by Mallika A. Lala entitled APPLICATION OF PHARMACOMETRIC METHODS TO IMPROVE PEDIATRIC DRUG DEVELOPMENT has been approved by her committee as satisfactory completion of the dissertation requirement for the degree of Doctor of Philosophy (Ph.D.) Jogarao V.S. Gobburu, FDA and F. Douglas Boudinot, School of Pharmacy Jurgen Venitz, School of Pharmacy Patricia W. Slattum, School of Pharmacy D’arcy P. Mays, College of Humanities and Sciences Susanna Wu-Pong, Graduate Program Director, School of Pharmacy Victor A. Yanchick, Dean, School of Pharmacy Dr. F. Douglas Boudinot, Dean of the Graduate School May 9th, 2011 i © Mallika A. Lala 2011 All Rights Reserved ii APPLICATION OF PHARMACOMETRIC METHODS TO IMPROVE PEDIATRIC DRUG DEVELOPMENT A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy at Virginia Commonwealth University. by MALLIKA A. LALA Bachelor of Pharmaceutical Science, UICT, India, 2006 Ph.D. -

Page | 1 Tuesday 7 June 14:00-18:00 Registration at the Conference
Tuesday 7 June 14:00-18:00 Registration at the Conference Venue 19:30-21:00 Welcome reception Wednesday 8 June 08:00-08:45 Registration 08:45-09:00 Welcome and Introduction Chair: Oscar Della Pasqua, 09:00-10:20 Immune response to drug treatment and immunotherapy Dinesh De Alwis A biological perspective on immune response to drug treatment 09:00-09:40 Nigel Klein (intended and unintended effects) Intricate PK and PD for the novel immunocytokine CEA-IL2v and their 09:40-10:00 Hans Peter Grimm pre-clinical to clinical translation Investigation of anti-CTLA-4 immuno-oncology therapy through a 10:00-10:20 Kirill Peskov quantitative systems pharmacology model 10:20-11:40 Coffee break, Poster and Software session I Posters in Group I (with poster numbers starting with I-) are accompanied by their presenter 11:40-12:20 Systems pharmacology Chair: Charlotte Kloft 11:40-12:00 Kapil Gadkar A Six-Stage Workflow for Robust Application of Systems Pharmacology The zebrafish as model for translational systems pharmacology: 12:00-12:20 Rob van Wijk expanding the allometric scale in vertebrates with five orders of magnitude 12:20-13:50 Lunch Chair: Leon Aarons, Shasha 13:50-15:05 Growth (I) Jumbe Introduction to the Gates' Healthy Birth, Growth & Development 13:50-14:05 Shasha Jumbe knowledge integration project 14:05-14:45 Louise Ryan Trajectory modelling based on early childhood longitudinal growth data Page | 1 Determinants for physical growth patterns in low- and middle-income 14:45-15:05 Niclas Jonsson countries 15:05-15:10 Announcement of WCoP 2016 -

Regulatory Pharmacometrics in the EU in Practice, and the Role of The
Pharmacometric Modelling to Support Extrapolation in Regulatory Submissions Kristin Karlsson, PhD Pharmacometric/Pharmacokinetic assessor Medical Products Agency, Uppsala ,Sweden PSI One Day Extrapolation Workshop Disclaimer The views expressed in this presentation are those of the speaker, and are not necessarily those of MPA or EMA. Outline • Introduction to pharmacometrics and extrapolation • Why population analysis • What are population models used for in support for extrapolation from adults to children • Design and modelling considerations • How to assess exposure similarity between adults and children • Conclusion Pharmacometrics “the science of developing and applying mathematical and statistical models to characterize, understand and predict a drug’s pharmacokinetics, pharmacodynamics and biomarker-outcome behavior, data visualization, statistics, stochastic simulations and computer programming” [1] • Pharmacokinetics “what the body does to the drug” • Pharmacodynamics (=Response) “what the drug does to the body” • Biomarker-outcome behavior disease progression, relationship between biomarkers and clinical endpoints etc. [1] Ette, E.I. and P.J. Williams, Pharmacometrics: The Science of Quantitative Pharmacology. 2007: John Wiley & Sons. EMA Modelling and Simulation Working Group 2016 Activity Report • 105 product related procedures – 41 from Paediatric committee, – 62 from Scientific advise working party, – 2 from CHMP – 7 Guidelines • A breakdown of the scope of questions addressed by M&S is shown in the pie chart Courtesy of -

The Utility of Pharmacometrics in Drug Development And
THE UTILITY OF PHARMACOMETRICS IN DRUG DEVELOPMENT AND PHARMACOTHERAPY OF ANTIMICROBIALS A DISSERTATION SUBMITTED TO THE FACULTY OF THE UNIVERSITY OF MINNESOTA BY ALI AHMED ALHADAB IN PARTIAL FULFILLIMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY RICHARD C. BRUNDAGE, Advisor MARNIE L. PETERSON, Co-Advisor December 2017 © Copyright Ali A. Alhadab 2017 All Rights Reserved AKNOWLEDGEMENTS Many people without who this thesis would not have been possible deserve my sincere gratitude. First and foremost, my wholehearted thanks go to Almighty Allah, the most Merciful the most Compassionate, the one who provides me with all I need, guides me throughout my journey, and equips me with the capabilities to accomplish this work. I am thankful and honored to work under the supervision of Dr. Richard Brundage. Not only was he an adviser, but also he was a mentor, friend and father as the same time. Your help, support, guidance, encouragement and patience throughout the program were surely behind my success. Thank you for always being there for me and putting my personal needs and professional aspirations first. You have been my last resort to go to because I knew you would do your best to ensure things go the way I wish. A special thanks to my co-adviser. Dr. Marine Peterson, the person behind my acceptance into the Experimental and Clinical Pharmacology (ECP) graduate program. She was also the one who introduced me to and established the collaboration with Dr. David Boulware. I am really indebted to her in many ways and I cannot thank her enough. -

Curriculum Vitae
Curriculum Vitae PERSONAL INFORMATION Leon Aarons WORK EXPERIENCE March 1976- Present Professor The University of Manchester (United Kingdom) Researcher and teacher in the areas of pharmacokinetics and pharmacodynamics EDUCATION AND TRAINING September 1971-December 1973 PhD The University of Manchester (United Kingdom) PhD in Theoretical Chemistry ADDITIONAL INFORMATION Expertise Pharmacokinetic and pharmacodynamic modelling; population pharmacokinetic modellingt; optimal design of pharmacokinetic and pharmacodynamic clinical trials; physiologically based pharmacokinetic modelling; drug absorption modelling Publications S.Y.A. Cheung, T. Rodgers, L. Aarons, I. Gueorguieva, G.L. Dickinson, S. Murby, C. Brown, B. Collins, M. Rowland, Whole body physiologically based modelling of -blockers in the rat: events in tissues and plasma following an i.v. bolus dose, Br J Pharmacol DOI:10.1111/bph.14071 (2017). Y.T. Patel, V.M. Daryani, P. Patel, D. Zhou, J. Fangusaro, D.J. Carlile, P.D. Martin, L Aarons, C.F. Stewart, 'Population pharmacokinetics of selumetinib and its metabolite N-desmethyl-selumetinib in adult patients with advanced solid tumors and children with low-grade gliomas CPT Pharmacometrics Syst Pharmacol 6, 305-314 (2017). S.C. Goulooze, S. Völler, P.A.J. Völitalo, E.A.M. Calvier, L. Aarons, E.H.J. Krekels, C.A.J. Knibbe, The influence of normalization weight in population pharmacokinetic covariate models, Clin Pharmacokinet DOI:10.1007/s40262-018-0652-7 (2018). C. Imholt,| T. Abdulla,| A. Stevens,| P. Edwards,| J. Jacob, D. Woods, E. Rogers, L. Aarons, D. Segelcke, Establishment and validation of microsampling techniques in wild rodents for ecotoxicological research, Appl Toxicol DOI: 10.1002/jat.3635 (2018). E.C. -

Pharmacometrics: a Multidisciplinary Field to Facilitate Critical Thinking in Drug Development and Translational Research Settings
FORUM Pharmacometrics: A Multidisciplinary Field to Facilitate Critical Thinking in Drug Development and Translational Research Settings Jeffrey S. Barrett, PhD, FCP, Michael J. Fossler, PharmD, PhD, FCP, K. David Cadieu, BS, and Marc R. Gastonguay, PhD Pharmacometrics has evolved beyond quantitative analy- without such backgrounds. Given the paucity of existing sis methods used to facilitate decision making in drug training programs, available training materials, and acad- development, although the application of the discipline in emic champions, a virtual faculty and online curriculum this arena continues to represent the primary emphasis of would allow students to matriculate into one of several scientists calling themselves pharmacometricians. While programs associated with their advisor but take instruc- related fields populate and interface with pharmacomet- tion from faculty at multiple institutions, including rics, there is a natural synergy with clinical pharmacology instructors in both industrial and regulatory settings. due to common areas of research and the decision-making Flexibility in both the curriculum and the governance of expectation with respect to evolving conventional and the degree would provide the greatest hope of addressing translational research paradigms. Innovative and adapt- the short supply of trained pharmacometricians. able training programs and resources are essential in this regard as both disciplines promise to be key elements of the clinical research workplace of the future. The demand Keywords: Pharmacometrics; -

Pharmacometric Models to Improve Treatment of Tuberculosis
Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Pharmacy 214 Pharmacometric Models to Improve Treatment of Tuberculosis ELIN M SVENSSON ACTA UNIVERSITATIS UPSALIENSIS ISSN 1651-6192 ISBN 978-91-554-9539-8 UPPSALA urn:nbn:se:uu:diva-282139 2016 Dissertation presented at Uppsala University to be publicly examined in B21, BMC, Husargatan 3, Uppsala, Friday, 20 May 2016 at 09:15 for the degree of Doctor of Philosophy (Faculty of Pharmacy). The examination will be conducted in English. Faculty examiner: Senior Program Officer, Quantitative Sciences N. L’Ntshotsholé (Shasha) Jumbe (Deptartment of Global Health, Bill & Melinda Gates Foundation). Abstract Svensson, E. M. 2016. Pharmacometric Models to Improve Treatment of Tuberculosis. Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Pharmacy 214. 79 pp. Uppsala: Acta Universitatis Upsaliensis. ISBN 978-91-554-9539-8. Tuberculosis (TB) is the world’s most deadly infectious disease and causes enormous public health problems. The comorbidity with HIV and the rise of multidrug-resistant TB strains impede successful therapy through drug-drug interactions and the lack of efficient second-line treatments. The aim of this thesis was to support the improvement of anti-TB therapy through development of pharmacometric models, specifically focusing on the novel drug bedaquiline, pharmacokinetic interactions and methods for pooled population analyses. A population pharmacokinetic model of bedaquiline and its metabolite M2, linked to semi-mechanistic models of body weight and albumin concentrations, was developed and used for exposure-response analysis. Treatment response was quantified by measurements of mycobacterial load and early bedaquiline exposure was found to significantly impact the half- life of bacterial clearance. -

Guideline for Exposure-Response Analysis of Drugs”
Provisional Translation (as of July 2020)* Administrative Notice June 8, 2020 To: Prefectural Health Department (Bureau) Pharmaceutical Evaluation Division, Pharmaceutical Safety and Environmental Health Bureau, Ministry of Health, Labour and Welfare English Translation of “Guideline for Exposure-Response Analysis of Drugs” The “Guideline for Exposure-Response Analysis of Drugs” (in Japanese language) has been published in the “Notification of Guideline for Exposure-Response Analysis of Drugs” (PSEHB/PED Notification No. 0608-4, by the Director of the Pharmaceutical Evaluation Division, Pharmaceutical Safety and Environmental Health Bureau, Ministry of Health, Labour and Welfare, dated June 8, 2020; hereinafter referred to as “Notification”) to ensure that relevant manufacturers and sellers placed under your administration are informed about the guideline. An English language translation of the Japanese language guideline has now been prepared as presented below. We ask you to inform relevant manufacturers and sellers placed under your administration about this English version of the guideline. It should be noted that the official text of this guideline is the Japanese language version as shown in the attachment to the Notification. The English version is provisional and is intended to be a reference material. *This English version of the Japanese Administrative Notice is provided for reference purposes only. In the event of any inconsistency between the Japanese original and the English translation, the former shall prevail. The following English translation of Japanese Guideline is intended to be a reference material to provide convenience for users. In the event of inconsistency between the Japanese original and the translation, the former shall prevail. Provisional Translation PSEHB/PED Notification No. -
Speaker Bios: Development of Best Practices in Physiologically Based Pharmacokinetic Modeling to Support Clinical Pharmacology R
Speaker Bios Development of Best Practices in Physiologically Based Pharmacokinetic Modeling to Support Clinical Pharmacology Regulatory Decision-Making November 18th, 2019 FDA White Oak Campus Great Room Susan Cole, BSc Expert Pharmacokinetics Assessor and Head of the Pharmacokinetics Group, Medicines and Healthcare products Regulatory Agency Susan Cole is an Expert Pharmacokinetics Assessor and Head of the Pharmacokinetics group at the UK Regulatory Agency. She is also a member of the Pharmacokinetics Working Party and the Modelling and Simulation Working Party at the European Medicines Agency. Prior to joining the MHRA in 2012, Sue worked for 26 years at Pfizer in the UK in the field of Drug Metabolism and Pharmacokinetics. While in industry, Sue fulfilled several roles including: Head of the Preclinical Pharmacokinetics and Modelling group and as a Clinical Pharmacologist. Sue was also one of the Rapporteurs on the EMA guideline: The Reporting of Physiologically Based Pharmacokinetic (PBPK) Modelling and Simulation. Grace Fraczkiewicz, BS, MSc Team Leader, Simulation Studies, Simulations Plus, Inc. Grace Fraczkiewicz is currently Team Leader of the Simulation Studies Team at Simulations Plus, where she mentors and manages a team of scientists providing mechanistic absorption and PBPK modeling consulting services for the pharmaceutical industry. Projects performed by her group encompass all areas of pharmaceutical product development, from early discovery through clinical development, and she has been involved in numerous studies that informed regulatory decisions. Grace joined Simulations Plus in 2000 as a scientist supporting the development and validation of new software tools for the pharmaceutical industry, such as GastroPlus™, ADMET Predictor™, and DDDPlus™. She has been leading the consulting services team since 2010. -
Quantitative and Systems Pharmacology in the Post-Genomic Era: New Approaches to Discovering Drugs and Understanding Therapeutic Mechanisms
Quantitative and Systems Pharmacology in the Post-genomic Era: New Approaches to Discovering Drugs and Understanding Therapeutic Mechanisms An NIH White Paper by the QSP Workshop Group – October, 2011 Peter K. Sorger (co-chair), Sandra R.B. Allerheiligen (co-chair) Darrell R. Abernethy, Russ B. Altman, Kim L. R. Brouwer, Andrea Califano, David Z. D'Argenio, Ravi Iyengar, William J. Jusko, Richard Lalonde, Douglas A. Lauffenburger, Brian Shoichet, James L. Stevens, Shankar Subramaniam, Piet Van der Graaf and Paolo Vicini Rebecca Ward (editor) This work is licensed under a Creative Commons Attribution-ShareAlike 3.0 License Author Affiliations Peter K. Sorger Richard L. Lalonde WAB432, Department of Systems Biology Department of Clinical Pharmacology Harvard Medical School Pfizer Inc. Boston MA 02115 445 Eastern Point Road Groton, CT 06340 Darrell R. Abernethy Office of Clinical Pharmacology/FDA Douglas A. Lauffenburger 10903 New Hampshire Avenue Department of Biological Engineering 16-343 Silver Spring, MD 20993 Massachusetts Institute of Technology Cambridge MA 02139 Sandra R. B. Allerheiligen Merck Research Laboratories Brian Shoichet 351 N. Sumneytown Pike University of California, San Francisco North Wales, PA 19454-1099 Dept. of Pharmaceutical Chemistry San Francisco CA Russ B. Altman Stanford University James L. Stevens 301 Campus Drive, S170 Lilly Research Laboratories Stanford, CA 94025-5444 Indianapolis, IN 46285 Kim L. R. Brouwer Shankar Subramaniam UNC Eshelman School of Pharmacy Department of Bioengineering The University of North Carolina at Chapel Hill 9500 Gilman Drive #0412 Chapel Hill, NC 27599-7569 University of California San Diego La Jolla CA 92093 Andrea Califano Herbert Irving Comprehensive Cancer Center Piet Van der Graaf 1130 St.