The Utility of Pharmacometrics in Drug Development And
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Theory, Measurement, and Methods in the Study of Family Influences on Adolescent Smoking
Blackwell Science, LtdOxford, UKADDAddiction1359-6357© 2003 Society for the Study of Addiction to Alcohol and Other Drugs98Supplement 12136Original ArticleTheory, measurement and methodsNancy Darling & Patricio Cumsille REVIEW Theory, measurement, and methods in the study of family influences on adolescent smoking Nancy Darling1 & Patricio Cumsille2 1Program in Psychology, Bard College, NY, USA; 2Escuela de Psicología, Universidad Católica de Chile, Chile Correspondence to: ABSTRACT Nancy Darling Program in Psychology Bard College This paper discusses three dilemmas faced by researchers interested in family Annandale-on-Hudson, NY 12504 influences in substance use: the transitional nature of adolescent smoking, the USA complexity and multi-dimensionality of family forms and influences, and the E-mail: [email protected] inter-relationship of family influences with other key developmental contexts. Methodological and conceptual issues stemming from these dilemmas are dis- RESEARCH REPORT cussed with regard to understanding why previous reviews have found the cor- relations between family predictors and adolescent smoking to be relatively low. In particular, the importance of understanding time, the transitional nature of the phenomenon, and within- and between- family processes are emphasized. More appropriate conceptual and statistical models for analyzing family influ- ences are suggested, including both mixed models and person-centered approaches. KEYWORDS Adolescence, family, methodology, parental monitoring, parenting, substance use, smoking, tobacco use. INTRODUCTION The second dilemma researchers interested in family influences on adolescent smoking must grapple with is Although researchers interested in the development of the nature of the family itself. Although we speak com- adolescent smoking have long been interested in family monly of ‘the family unit’, within-family influences can- influences, the literature has been less than clear about not accurately be conceptualized as singular. -

Ancestor Tables
Swedish American Genealogist Volume 10 Number 4 Article 9 12-1-1990 Ancestor Tables Follow this and additional works at: https://digitalcommons.augustana.edu/swensonsag Part of the Genealogy Commons, and the Scandinavian Studies Commons Recommended Citation (1990) "Ancestor Tables," Swedish American Genealogist: Vol. 10 : No. 4 , Article 9. Available at: https://digitalcommons.augustana.edu/swensonsag/vol10/iss4/9 This Article is brought to you for free and open access by the Swenson Swedish Immigration Research Center at Augustana Digital Commons. It has been accepted for inclusion in Swedish American Genealogist by an authorized editor of Augustana Digital Commons. For more information, please contact [email protected]. (ISSN 0275-9314) Swedis•h American Genealo ist A journal devoted to Swedish American biography, genealogy and personal history CONTENTS Repositories of Scandinavian-American Materials: A Partial Directory 162 Swedes in the Naturalization Index - A Sampling 170 John Root Once More 178 A Swedish Bible Inscription 185 When Andrew Jackson Helped a Swedish(?) Tailor 186 Brodd-Jonas and Brodd-Marta: Two Bishop Hill Colonists Identified 188 Charles XII in America 190 Ancestor Tables 191 Genealogical Queries 194 What Happened to John Asplund's New Collections? 201 Index of Personal Names 203 Index of Place Names 219 Index of Ships' Names 224 Vol. X December 1990 No. 4 1 l • • ,-1. 1I Swedish America~ Genealogist Copyright © 1990 Swedish American Genealogist P.O. Box 2186 Winter Park. FL 32790 Tel. (407) 647-4292 (ISSN 0275-9314) Editor and Publisher Ni ls William Olsson, Ph.D .. F.A.S.G. I Contributing Editors Glen E. Brolander, Augustana College, Rock Is land, IL I l Peter Stebbins Craig, J .D. -

Crawford County, Michigan, Naturalization Index
CRAWFORD COUNTY NATURALIZATION INDEX Last Name First Name Middle Name First Paper Second Paper Ackerman Christopher A. V1 P1 Adamson William Buttle V3 P13 Ahman Frank Oscar V8 P15 Ahman Frank Oscar V2 P13 Ahrman Frank Oscar V7 P15 Alman Frank Oscar/Theodore V2 P13 Almon Mary Stephanie V11 P27 V11 P27 Almon Mary Stephanie V10 P159 Andereson Hans V3 P50 Andersen Hans V3 P50 Andersen Hilmas V1 P237 Andersen Jacob V1 P246 Andersen Soren V8 P40 Andersenn George V1 P243 Anderson August V1 P113 Anderson Charles V1 P134 Anderson Charles Ludwig V1 P39 Anderson Emil V1 P227 Anderson G V1 P243 Anderson George V7 P5 Anderson George V8 P5 Anderson Gust V5 P45 Anderson Gust V1 P154 Anderson Hans V1 P7 Anderson Hans Frederick V1 P35 Anderson Hilmar V1 P237 Anderson Israel V1 P3 Anderson Jacob V1 P246 Monday, July 22, 2002 Page 1 of 46 Last Name First Name Middle Name First Paper Second Paper Anderson John FP V5 P52 Anderson Karl V1 P147 Anderson Lassis A. V1 P21 Anderson Piven V1 P145 Anderson Sam V5 P115 Anderson Soren V8 40 Anderson Soren V1 P170 Anderson Soren V7 P40 Andersson George V1 P243 Andeson August V1 P131 Annette Jospeh L. V1 P90 Annis Hella Waili V10 P149 Annis Hella Walli V11 P24 V11 P24 Anstett Francis Louis V9 P5 V9 P5 Anthony Charles V1 P246 Appellery Oscar Edmund V2 P87 Appellury Oscar Edward V2 P87 Arenbren Hans Peter V1 P169 Arldsen Peter V1 P73 Armerson William John V1 P83 Armstrong James V9 P38 V9 P38 Armstrong James V3 P19 Arnold Alexander V1 P162 Arnold Erika V11 P20 Arnold Erika Luise V10 P142 Atkinson Marshall Alexander V9 P42 V9 P42 Atkinson Marshall Alexander V2 P97 Baddy Silas V1 P104 Badore Angnus V1 P182 Bandy Frank JR V5 P97 Monday, July 22, 2002 Page 2 of 46 Last Name First Name Middle Name First Paper Second Paper Banfield James V4 P180 Banney John V1 P152 Barber Charles V1 P53 Barber Charles Sidney V7 P28 Barber Charles Sidney V2 P31 Barber Charles Sidney V8 P28 Barber Chas V5 P34 Barber Ernest Roy V9 P27 Barber Fred E. -

Emergency Use Authorization (EUA) for Bamlanivimab 700 Mg and Etesevimab 1400 Mg IV Administered Together Center for Drug Evaluation and Research (CDER) Review
________________________________________________________________ Emergency Use Authorization (EUA) for Bamlanivimab 700 mg and Etesevimab 1400 mg IV Administered Together Center for Drug Evaluation and Research (CDER) Review Identifying Information Application Type (EUA or Pre-EUA) EUA If EUA, designate whether pre-event or intra-event EUA request. 1 EUA Application Number(s) EUA 000094 Sponsor (entity requesting EUA or Eli Lilly and Company pre-EUA consideration), point of Christine Phillips, PhD, RAC contact, address, phone number, fax Advisor, Global Regulatory Affairs - NA (b) (6) number, email address Mobile: Email: [email protected] Manufacturer, if different from Eli Lilly and Company Sponsor Submission Date(s) November 16, 2020 Receipt Date(s) November 16, 2020 OND Division / Office Division of Antivirals/Office of Infectious Diseases Reviewer Name(s)/Discipline(s) Natalie Pica, MD, PhD – Clinical Reviewer Wendy Carter, DO – Cross Discipline Team Lead Michael Thomson, PhD – Clinical Virology Reviewer Jules O’Rear, PhD – Clinical Virology Team Lead Daniel Rubin, PhD – Statistics Reviewer Thamban Valappil, PhD – Statistics Team Lead Dionne Price, PhD – Director, Division of Biometrics IV Jason Moore, PharmD – Clinical Pharmacology Reviewer Su-Young Choi PharmD, PhD – Clinical Pharmacology Team Lead Kellie Reynolds, PharmD – Division Director, DIDP Ye Xiong, PhD – Pharmacometrics Reviewer Justin Earp, PhD – Pharmacometrics Team Lead Yaning Wang, PhD – Division Director, DPM 1 If a Pre-EUA is in existence at the time -
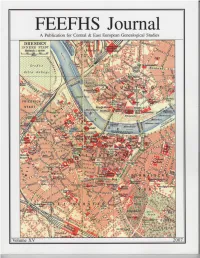
FEEFHS Journal Volume 15, 2007
FEEFHS Journal Volume 15, 2007 FEEFHS Journal Who, What and Why is FEEFHS? The Federation of East European Family History Societies Guest Editor: Kahlile B. Mehr. [email protected] (FEEFHS) was founded in June 1992 by a small dedicated group of Managing Editor: Thomas K. Edlund American and Canadian genealogists with diverse ethnic, religious, and national backgrounds. By the end of that year, eleven societies FEEFHS Executive Council had accepted its concept as founding members. Each year since then FEEFHS has grown in size. FEEFHS now represents nearly two 2006-2007 FEEFHS officers: hundred organizations as members from twenty-four states, five Ca- President: Dave Obee, 4687 Falaise Drive, Victoria, BC V8Y 1B4 nadian provinces, and fourteen countries. It continues to grow. Canada. [email protected] About half of these are genealogy societies, others are multi- 1st Vice-president: Brian J. Lenius. [email protected] purpose societies, surname associations, book or periodical publish- 2nd Vice-president: Lisa A. Alzo ers, archives, libraries, family history centers, online services, insti- 3rd Vice-president: Werner Zoglauer tutions, e-mail genealogy list-servers, heraldry societies, and other Secretary: Kahlile Mehr, 412 South 400 West, Centerville, UT. ethnic, religious, and national groups. FEEFHS includes organiza- [email protected] tions representing all East or Central European groups that have ex- Treasurer: Don Semon. [email protected] isting genealogy societies in North America and a growing group of worldwide organizations and individual members, from novices to Other members of the FEEFHS Executive Council: professionals. Founding Past President: Charles M. Hall, 4874 S. 1710 East, Salt Lake City, UT 84117-5928 Goals and Purposes: Immediate Past President: Irmgard Hein Ellingson, P.O. -
Hierarchical Mechanistic Modelling of Clinical Pharmacokinetic Data
Hierarchical mechanistic modelling of clinical pharmacokinetic data A thesis submitted to the University of Manchester for the degree of Doctor of Philosophy in the Faculty of Medical and Human Sciences 2015 Thierry Wendling Manchester Pharmacy School Contents List of Figures ........................................................................................................ 6 List of Tables .......................................................................................................... 9 List of abbreviations ............................................................................................ 10 Abstract ................................................................................................................ 13 Declaration ........................................................................................................... 14 Copyright ............................................................................................................. 14 Acknowledgements .............................................................................................. 15 Chapter 1: General introduction ...................................................................... 16 1.1. Modelling and simulation in drug development ........................................ 17 1.1.1. The drug development process .......................................................... 17 1.1.2. The role of pharmacokinetic and pharmacodynamic modelling in drug development .................................................................................................. -

Save the Date Join
WINTER 2015 changing lives, one child at a time. CSI Team Travels to Bangladesh for Teaching Mission In this Issue In 2010 Fazly Alahi, a native of Bangladesh currently CSI Travels to Bangladesh 1 living and working in Minnesota with his family, contacted Children’s Surgery International. He had Welcome, Dr. Sidman 2 a dream to make a connection between the United CSI Welcomes New Medical 3 States and Bangladesh that could bring much- Director, David Tetzlaff needed medical care and education to his home country. After a site visit, CSI chose Rangpur Thank You to Departing 3 Community Medical College Hospital in the northern Board Members region of the country. Partner Program: Vietnam 4 The first surgical mission traveled to Rangpur in 2011. Edina Couple Transform 4 The trip was a great success, performing many cleft- Young Lives related procedures and identifying the educational needs of local professionals. CSI’s partnership 2015 Mission Calendar 5 with Fazly and his family, as well as the Rangpur Fazly Alahi Thank You to CSI Donors 6-7 Community Medical College Hospital, provided crucial support to our team. The CSI medical team worked closely alongside local professionals, teaching and learning from one another. A second successful mission was completed in 2013. CSI hopes to send two mission teams to Bangladesh in 2015. Our teams will focus on promotion of self-sufficiency through hands-on training, education, and collaboration with local health save the date professionals. This year, CSI volunteer surgeons and nurses will implement site-specific educational curriculum during our stay in Rangpur. -

The 1693 Census of the Swedes on the Delaware
THE 1693 CENSUS OF THE SWEDES ON THE DELAWARE Family Histories of the Swedish Lutheran Church Members Residing in Pennsylvania, Delaware, West New Jersey & Cecil County, Md. 1638-1693 PETER STEBBINS CRAIG, J.D. Fellow, American Society of Genealogists Cartography by Sheila Waters Foreword by C. A. Weslager Studies in Swedish American Genealogy 3 SAG Publications Winter Park, Florida 1993 Copyright 0 1993 by Peter Stebbins Craig, 3406 Macomb Steet, N.W., Washington, D.C. 20016 Published by SAG Publications, P.O. Box 2186, Winter Park, Florida 32790 Produced with the support of the Swedish Colonial Society, Philadelphia, Pa., and the Delaware Swedish Colonial Society, Wilmington, Del. Printed in the United States of America Library of Congress Catalog Card Number 92-82858 ISBN Number: 0-9616105-1-4 CONTENTS Foreword by Dr. C. A. Weslager vii Introduction 1 Chapter 1: The 1693 Census 15 Chapter 2: The Wicaco Congregation 25 Chapter 3: The Wicaco Congregation - Continued 45 Chapter 4: The Wicaco Congregation - Concluded 65 Chapter 5: The Crane Hook Congregation 89 Chapter 6: The Crane Hook Congregation - Continued 109 Chapter 7: The Crane Hook Congregation - Concluded 135 Appendix: Letters to Sweden, 1693 159 Abbreviations for Commonly Used References 165 Bibliography 167 Index of Place Names 175 Index of Personal Names 18 1 MAPS 1693 Service Area of the Swedish Log Church at Wicaco 1693 Service Area of the Swedish Log Church at Crane Hook Foreword Peter Craig did not make his living, or support his four children, during a career of teaching, preparing classroom lectures, or burning the midnight oil to grade examination papers. -

Marriage Book Index, 1837-1920 Lake County, Indiana
Marriage Book Index, 1837‐1920 Lake County, Indiana This index was developed from marriage license books located in Lake County, Indiana, spanning 1837 to 1920. Both groom and bride indexes will provide the following information: the book number, page number, a license number, application number, groom and bride’s name, age (if given), a second spelling (if given), and the marrying official. We have added the church name (if given) in the notes columns and whether there was consent by a parent or nearest relative. Requests for copies of the original marriage application and license can be made by contacting the Lake County, Indiana, Clerk’s Office using the form at the following website (Note that the Clerk's Office asks that you send no more than three requests at one time): http://www.rootsweb.ancestry.com/~innwigs/Archives/MarriageLicCopies.pdf © 2009 ‐ Northwest Indiana Genealogical Society Northwest Indiana Genealogical Society Marriage Book Index, 1837-1920 Brides Lake County, Indiana Surname Begins with P Bk# Pg# Lic # Appl Rec Groom's L Name G 2nd Sp Groom's F Name Groom's Age Bride's L Name B 2nd Sp Bride's F Name Bride's Age Appl Date Return Date Marr Date Marrying Official Title Clerk Misc Notes 059 421 085452 256 SPISAK Joseph PAA Elsie 06/08/1926 07/01/1926 06/08/1926 Kemp, Howard H. JP John Killigrew 010 094 MAY Daniel J, Jr. 21 PAAPE Minnie 18 02/10/1903 02/20/1903 02/15/1903 Wood, A. W. Min Harold H. Wheeler Hammond 026 129 032422 080 PIERCE LeRoy PAASCH Elsie 09/23/1915 09/28/1915 09/23/1915 Stockbarger, Charles U. -

Results Autumn Classic Sale 559
Results Autumn Classic Sale 559 No. Item Hammer price 1 Carl Johansson, Spring landscape. 22 000 SEK 2 Alfred Bergström, Summer landscape, Concarneau. 17 000 SEK 3 Georg Pauli, "Franskt landskap" (French landscape). 20 000 SEK 4 Georg Pauli, French landscape. Unsold 5 Carl Skånberg, Boats on the shore, coastal scene from the north of France. 16 000 SEK 6 Per Ewert, The harbour in Concarneau, Brittany. Unsold 7 Bror Oscar Eugen Börjeson, Still life. 25 000 SEK 8 Mina (Vilhelmina) Carlsson-Bredberg, Still life. 17 000 SEK 9 Emma Löwstedt-Chadwick, Angling boy. 14 500 SEK 10 Carl Trägårdh, Elegant lady by the sea. 72 000 SEK 11 Nils Kreuger, "Gråväder", Knapegård (Grey weather, Knapegård). 330 000 SEK 12 Nils Kreuger, "Tjur och ko vid Snärjebäcken", Knapegård (Bull and cow by 160 000 SEK Snärjebäcken, Knapegård). 13 Nils Kreuger, "Bessie vid krysantemumträdet" (Bessie by the chrysanthemum). Unsold 14 Nils Kreuger, Spring evening. 68 000 SEK 15 Nils Kreuger, "Vårafton" (Spring evening). 105 000 SEK 16 Helmer Osslund, "Hösttavla från Abisko" (Autumn painting from Abisko). 32 000 SEK 17 Helmer Osslund, "Niporna i Ångermanälven" (Sandbanks in the Ångerman river). 17 500 SEK 18 Helmer Osslund, Autumn landscape with dark skies. 25 000 SEK 19 Helmer Osslund, River landscape with darkening skies. 15 000 SEK 20 Helmer Osslund, Autumn landscape from Torne träsk with Lapporten. 410 000 SEK 21 Thure Wallner, Osprey in nest. 21 000 SEK 22 Thure Wallner, Winter landscape with partridges. 31 000 SEK 23 Thure Wallner, "Lövsångare i vårsol" (Willow warbler in spring sun). 19 000 SEK 24 Mosse Stoopendaal, "Rödhakar" (Redbreasts). -

Kent County Naturalization Name Index, Paauwe to Radamacher
Last name First name Middle name Volume Page Fir Sec Paauwe Jacobus V79 23 Paauwe Leonard V36 24 Paauwe Leonard V75 161 Paauwe Marienis V16 564 Paauwe Nicolaas V8 58 Paauwe Peter Albert V68 108 Paawue Nicholaas V17 328 Paawue Nicolaas V17 328 Paboyeski Theodore V18 31 Pacewiecz Frank V39 4 Pacher Peter V79 80 Pachowicz Edmund Antoni V35 69 Pachowicz Edmund Antoni V55 16 Pachowicz Ludwik V54 131 Pachowitz Edmund V35 64 Pachulski Felix V43 48 Pachulski Felix V68 21 Pacific Jun V40 470 Pacific Tito V40 478 Packer Albert B11 F7 Packer Albert V43 130 Packer Charles V33 51 Packer Cornelius B11 F9 Packer Cornelius V2 165 Packer Joseph B7 110 Packer Walter Jay V15 447 Packowski John V48 84 Pacukiewicz Karol V31 5365 Friday, January 19, 2001 Page 823 of 1325 Last name First name Middle name Volume Page Fir Sec Pacze James V18 157 Paczkowski John V40 257 Paczkowski John V64 74 Paczkowski Louis Joe V43 249 Paczkowski Murry V42 253 Paczkowski Stanislaw V20 119 Paczkowski Stanislaw V78 164 Padelt Frank B11 F8 Padelt Franz V14 487 Padelt Franz V2 10 Padgett William V5 12 Padgorski John V83 241 Padmos Adriana V68 192 Padmos Bouden Wyn V15 38 Padmos Cornelia V68 191 Padmos Gerrit Antoni V45 308 Padmos Gerrit Antoni V82 175 Paeceans Joseph B7 178 Paelman Anton V21 254 Paeplow Christ V14 211 Paesens Klaas V80 66 Paesens Nick V39 133 Paesens Nick V80 66 Paezens Antonetta Maria V47 169 Paff Peter V15 402 Paffhausen Anton V14 527 Paffhausen Anton V5 357 Paffhausen Casper V14 526 Friday, January 19, 2001 Page 824 of 1325 Last name First name Middle name Volume Page Fir Sec Paffhausen Casper V5 357 Paffhausen John A. -
Endophenotypes for Nicotine- Dependence Risk at Or Before Initial Nicotine Exposure
8 Endophenotypes for Nicotine- Dependence Risk at or before Initial Nicotine Exposure Janet Audrain-McGovern, Joel T. Nigg, and Kenneth A. Perkins Characteristics present before or at the time of nicotine exposure may play a key role in identifying individuals at genetic risk for nicotine dependence. This chapter examines the evidence base for several candidate endophenotypes for nicotine-dependence risk at or before smoking and nicotine exposure, including the following: ■ Approach-related smoking risk variables based on psychological traits such as impulsivity, novelty seeking, and extraversion, using laboratory measures for aspects of reinforcement and reward ■ Avoidance-related smoking risk variables based on psychological factors such as neuroticism, stress, depression, and anxiety, using laboratory measures including personality trait measures, peripheral nervous system (PNS) effects, and neuroendocrine response to cortisol ■ Control-related smoking risk based on psychological variables such as attention deficit hyperactivity disorder (ADHD), conduct disorders, aggression, and hostility, using laboratory measures including response inhibition, event-related potential (ERP) P300 amplitude, attention, and alertness ■ Measures of initial response to nicotine exposure, including reinforcement and reward measures of initial sensitivity to nicotine, as well as initial sensitivity to affective and mood responses to nicotine Although available evidence shows a link between many of these variables and smoking behavior, further research is