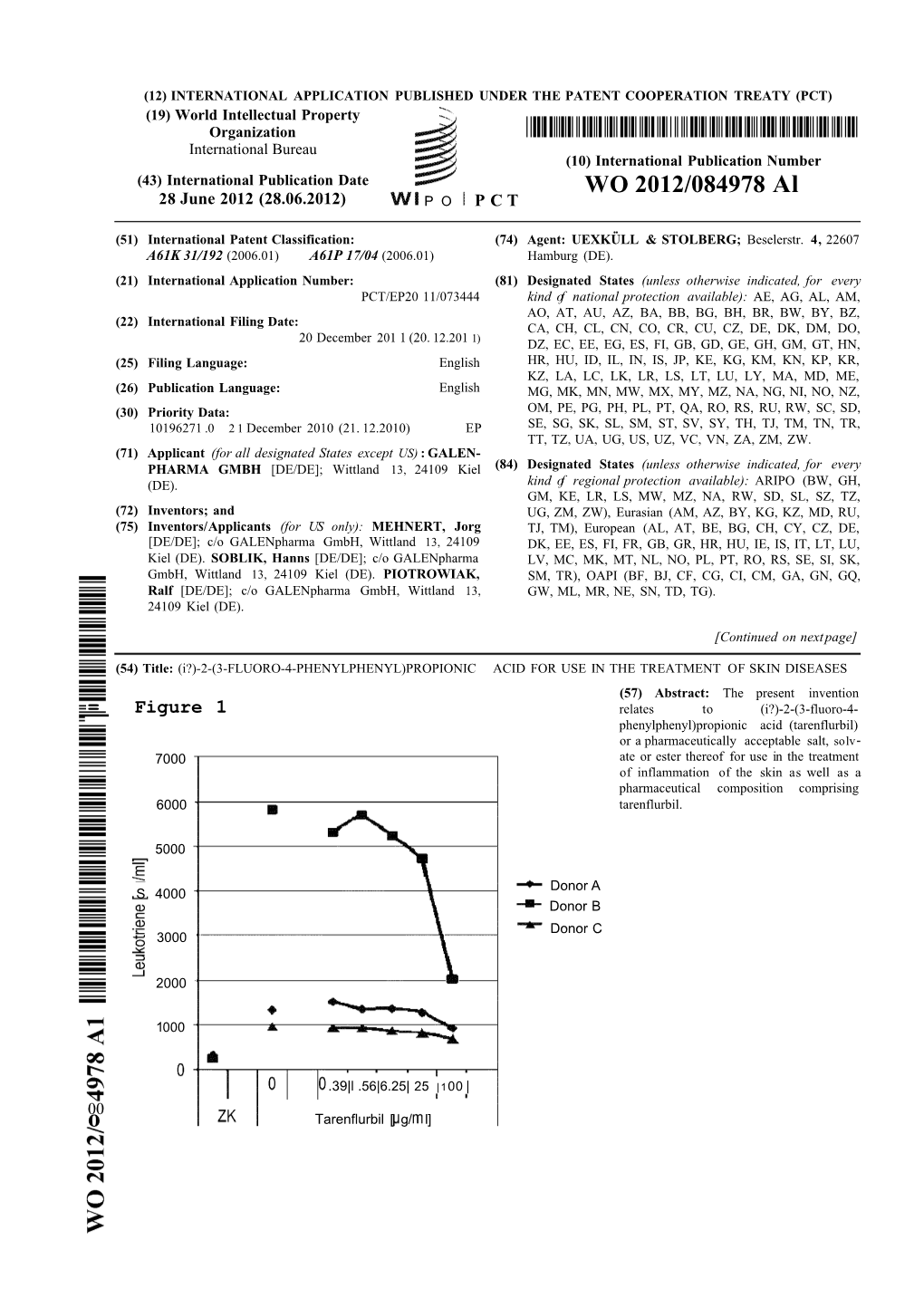
WO 2012/084978 Al 28 June 2012 (28.06.2012) P O P C T
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Are Nsaids Useful to Treat Alzheimer's Disease Or Mild Cognitive
REVIEW ARTICLE published: 21 May 2010 AGING NEUROSCIENCE doi: 10.3389/fnagi.2010.00019 Are NSAIDs useful to treat Alzheimer’s disease or mild cognitive impairment? Bruno P. Imbimbo1*, Vincenzo Solfrizzi 2 and Francesco Panza 3 1 Research and Development Department, Chiesi Farmaceutici, Parma, Italy 2 Department of Geriatrics, Center for Aging Brain, Memory Unit, University of Bari, Bari, Italy 3 Department of Medical Sciences, Geriatric Unit and Gerontology-Geriatrics Research Laboratory, IRCCS “Casa Sollievo della Sofferenza”, San Giovanni Rotondo, Foggia, Italy Edited by: Several epidemiological studies suggest that long-term use of non-steroidal anti-infl ammatory Elena Galea, Universitat Autònoma de drugs (NSAIDs) may protect subjects carrying one or more ε4 allele of the apolipoprotein E Barcelona, Spain (APOE ε4) against the onset of Alzheimer’s disease (AD). The biological mechanism of this Reviewed by: Mathieu Lichtenstein, Universitat protection is not completely understood and may involve the anti-infl ammatory properties of Autònoma de Barcelona, Spain NSAIDs or their ability of interfering with the β-amyloid (Aβ) cascade. Unfortunately, long-term, Merce Boada, Institut Català de placebo-controlled clinical trials with both non-selective and cyclooxygenase-2 (COX-2) selective Neurociències Aplicades, Spain inhibitors in mild-to-moderate AD patients produced negative results. A secondary prevention Elena Galea, Universitat Autònoma de Barcelona, Spain study with rofecoxib, a COX-2 selective inhibitor, in patients with mild cognitive impairment *Correspondence: was also negative. A primary prevention study (ADAPT trial) of naproxen (a non-selective COX Bruno P. Imbimbo, Research and inhibitor) and celecoxib (a COX-2 selective inhibitor) in cognitively normal elderly subjects with Development Department, Chiesi a family history of AD was prematurely interrupted for safety reasons after a median period Farmaceutici, Via Palermo 26/A, 43100 of treatment of 2 years. -

(12) Patent Application Publication (10) Pub. No.: US 2012/0202780 A1 Gavin Et Al
US 20120202780A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2012/0202780 A1 Gavin et al. (43) Pub. Date: Aug. 9, 2012 (54) CARRIER COMPOSITION Publication Classification (76) Inventors: Paul David Gavin, Chadstone (51) Int. Cl. (AU); Mahmoud El-Tamimy, A6II 47/24 (2006.01) Meadow Heights (AU); Jeremy A6II 3/196 (2006.01) James Cottrell, Caulfield South A6IP5/00 (2006.01) (AU); Giacinto Gaetano, South A 6LX 3/573 (2006.01) Melbourne (AU); Nicholas John A6IP 23/00 (2006.01) Kennedy, Boronia (AU) A6IP 29/00 (2006.01) A6II 3/167 (2006.01) (21) Appl. No.: 13/501,494 A63L/407 (2006.01) (22) PCT Fled: Dec. 22, 2010 (52) U.S. Cl. ......... 514/180: 514/785: 514/788: 514/772: 514/626; 514/567; 514/413: 514/179 (86) PCT NO.: S371 (c)(1), (57) ABSTRACT (2), (4) Date: Apr. 12, 2012 A carrier composition of the present invention comprises a phosphate compound of an electron transfer agent and a rela Related U.S. Application Data tively high concentration of a polar protic solvent. A biologi (60) Provisional application No. 61/289,507, filed on Dec. cally active compound may be formulated with a carrier com 23, 2009. position of the present invention to provide a formulation. Patent Application Publication Aug. 9, 2012 Sheet 1 of 5 US 2012/0202780 A1 - - if solvent E. -ie-20% solvent 3. ". S. .t E FGURE 1 Patent Application Publication Aug. 9, 2012 Sheet 2 of 5 US 2012/0202780 A1 -H 10 LC2 s -C- 20 ulcm2 . - a 30 ulcm2 t E re FIGURE 2A HO licm2 80i -o- 20 ul/cm2 'i -A-30 ul/cm2 140 EO 10 8 8 4) O O FIGURE 2B Patent Application Publication Aug. -

Review on Evaluating the Role of Nsaids for the Treatment of Alzheimer's Disease
International Journal of Applied Pharmaceutics ISSN- 0975-7058 Vol 13, Issue 1, 2021 Review Article REVIEW ON EVALUATING THE ROLE OF NSAIDS FOR THE TREATMENT OF ALZHEIMER'S DISEASE KRISHNENDU P. R.a, ARJUN B.a, VIBINA K.b, NIVEA CLEO T. S.c, DRISYA N. K.c, RADHIKA MOHANDASb, SUBIN MARY ZACHARIAHd* a,dDepartment of Pharmaceutical Chemistry and Analysis, Amrita School of Pharmacy, AIMS Health Sciences Campus, Amrita Vishwa Vidyapeetham, AIMS, Kochi 682041, Kerala, India, bDepartment of Pharmaceutical Chemistry, Lecturer, Crescent College of Pharmaceutical Science, Madayipara, P O. Payangadi (R. S.), 670358, Kannur, Kerala, India, cDepartment of Pharmaceutical Chemistry, Lecturer, KMCT College of Pharmaceutical Sciences, Technical Campus, Kallanthode, NITC, Calicut,673601, Kerala, India *Email: [email protected] Received: 05 Oct 2020, Revised and Accepted: 27 Nov 2020 ABSTRACT Recently, several studies have been reported that nonsteroidal anti-inflammatory drugs can fight against neurodegenerative disorders by various mechanisms. Currently, available therapies of neurodegenerative disorders (NDs) provide only symptomatic relief. This is the point at which we need an alternative that acts on the root cause of disease. Parkinson’s disease and Alzheimer’s disease are the two NDs concentrated here. Since the drug profile is already known, drug repurposing is a promising technique in research, thereby reducing the cost and period effectively. Epidemiological studies on various nonsteroidal anti-inflammatory drugs (NSAIDs) showed good results, but when it came to clinical studies the results are found to be poor. Hence, it can be concluded that NSAIDs provide its neuroprotective activity on its long-term use only, as the brain accessibility of this kind of drug is poor due to its lower lipophilicity. -

Phenotype-Based Drug Screening Reveals Association Between Venetoclax Response and Differentiation Stage in Acute Myeloid Leukemia
Acute Myeloid Leukemia SUPPLEMENTARY APPENDIX Phenotype-based drug screening reveals association between venetoclax response and differentiation stage in acute myeloid leukemia Heikki Kuusanmäki, 1,2 Aino-Maija Leppä, 1 Petri Pölönen, 3 Mika Kontro, 2 Olli Dufva, 2 Debashish Deb, 1 Bhagwan Yadav, 2 Oscar Brück, 2 Ashwini Kumar, 1 Hele Everaus, 4 Bjørn T. Gjertsen, 5 Merja Heinäniemi, 3 Kimmo Porkka, 2 Satu Mustjoki 2,6 and Caroline A. Heckman 1 1Institute for Molecular Medicine Finland, Helsinki Institute of Life Science, University of Helsinki, Helsinki; 2Hematology Research Unit, Helsinki University Hospital Comprehensive Cancer Center, Helsinki; 3Institute of Biomedicine, School of Medicine, University of Eastern Finland, Kuopio, Finland; 4Department of Hematology and Oncology, University of Tartu, Tartu, Estonia; 5Centre for Cancer Biomarkers, De - partment of Clinical Science, University of Bergen, Bergen, Norway and 6Translational Immunology Research Program and Department of Clinical Chemistry and Hematology, University of Helsinki, Helsinki, Finland ©2020 Ferrata Storti Foundation. This is an open-access paper. doi:10.3324/haematol. 2018.214882 Received: December 17, 2018. Accepted: July 8, 2019. Pre-published: July 11, 2019. Correspondence: CAROLINE A. HECKMAN - [email protected] HEIKKI KUUSANMÄKI - [email protected] Supplemental Material Phenotype-based drug screening reveals an association between venetoclax response and differentiation stage in acute myeloid leukemia Authors: Heikki Kuusanmäki1, 2, Aino-Maija -

Wo 2011/060944 A2
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date _ . ... _ 26 May 2011 (26.05.2011) WO 2011/060944 A2 (51) International Patent Classification: (74) Agents: CARVAJAL Y URQUIJO, Isabel et al; A61K 9/16 (2006.01) A61K 9/50 (2006.01) Clarke, Modet & Co., C/Goya 11, 28001 Madrid (ES). A61K 9/48 (2006.01) (81) Designated States (unless otherwise indicated, for every (21) International Application Number: kind of national protection available): AE, AG, AL, AM, PCT/EP20 10/007024 AO, AT, AU, AZ, BA, BB, BG, BH, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, (22) International Filing Date: DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, 19 November 2010 (19.1 1.2010) HN, HR, HU, ID, IL, IN, IS, JP, KE, KG, KM, KN, KP, (25) Filing Language: English KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, (26) Publication Langi English NO, NZ, OM, PE, PG, PH, PL, PT, RO, RS, RU, SC, SD, (30) Priority Data: SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, 200931026 20 November 2009 (20.1 1.2009) ES TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. (71) Applicants (for all designated States except US): GP (84) Designated States (unless otherwise indicated, for every PHARM, S.A. [ES/ES]; Poligono Industrial Els Vinyets- kind of regional protection available): ARIPO (BW, GH, Els Fogars, Ctra. -

Ep 2921486 B1
(19) TZZ __T (11) EP 2 921 486 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: C07D 303/18 (2006.01) A61K 31/336 (2006.01) 27.09.2017 Bulletin 2017/39 A61P 25/28 (2006.01) C07D 303/48 (2006.01) (21) Application number: 14188202.7 (22) Date of filing: 06.08.2010 (54) Compositions and methods for treating beta-amyloid related diseases Zusammensetzungen und Verfahren zur Behandlung von durch beta-Amyloid vermittelter Erkrankungen Compositions et procédés pour le traitement de maladies liées au bêta-amyloïde (84) Designated Contracting States: (56) References cited: AL AT BE BG CH CY CZ DE DK EE ES FI FR GB WO-A2-2004/084830 GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO PL PT RO SE SI SK SM TR • YAMAMOTO D ET AL: "Crystal Structure and Molecular Conformation of E-64,a Cysteine (30) Priority: 07.08.2009 US 232388 P Protease Inhibitor", CHEMICAL & 07.08.2009 US 232383 P PHARMACEUTICAL BULLETIN, vol. 37, no. 10, 25 11.01.2010 US 293783 P October 1989 (1989-10-25), pages 2577-2581, XP008152644, PHARMACEUTICAL SOCIETY OF (43) Date of publication of application: JAPAN, JP ISSN: 0009-2363 23.09.2015 Bulletin 2015/39 • Anonymous: "Precision Deuterium Chemistry Backgrounder", CoNCERT Pharmaceuticals, Ic. , (60) Divisional application: 2007, pages 1-6, XP002687117, lexington, MA 17182879.1 02421, USA Retrieved from the Internet: URL:http://www.concertpharma.com/about/doc (62) Document number(s) of the earlier application(s) in uments/ConcertProductPlatformBackgrounder. -

(12) Patent Application Publication (10) Pub. No.: US 2015/0258120 A1 Zarnitsyn Et Al
US 20150258120A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2015/0258120 A1 Zarnitsyn et al. (43) Pub. Date: Sep. 17, 2015 (54) METHODS AND DEVICES FOR THE 3, 2013, provisional application No. 61/873,660, filed TREATMENT OF OCULAR DISEASES IN on Sep. 4, 2013, provisional application No. 61/898, HUMAN SUBJECTS 926, filed on Nov. 1, 2013. (71) Applicant: CLEARSIDE BIOMEDICAL, INC., Publication Classification Alpharetta, GA (US) (51) Int. Cl. (72) Inventors: Vladimir Zarnitsyn, Atlanta, GA (US); A 6LX3/573 (2006.01) Samirkumar Patel, Atlanta, GA (US); A619/00 (2006.01) Daniel White, Suwanee, GA (US); A6M 37/00 (2006.01) Glenn Noronha, Atlanta, GA (US); A619/16 (2006.01) Brian Burke, Cary, NC (US) (52) U.S. Cl. CPC ................. A6 IK3I/573 (2013.01); A61 K9/16 (21) Appl. No.: 14/441,151 (2013.01); A61 K9/0048 (2013.01); A61M 37/0015 (2013.01); A61M 2037/0023 (22) PCT Fled: Nov. 8, 2013 (2013.01); A61M 2037/0061 (2013.01) (86) PCT NO.: PCT/US13A69156 (57) ABSTRACT S371 (c)(1), Methods and devices are provided for targeted non-Surgical (2) Date: May 6, 2015 administration of a drug formulation to the Suprachoroidal space (SCS) of the eye of a human subject for the treatment of a posterior ocular disorder or a choroidal malady. In one Related U.S. Application Data embodiment, the method comprises inserting a hollow (60) Provisional application No. 61/724,144, filed on Nov. microneedle into the eye at an insertion site and infusing a 8, 2012, provisional application No. -

ALZHEIMER's DISEASE UPDATE on CURRENT RESEARCH Lawrence S
ALZHEIMER'S DISEASE UPDATE ON CURRENT RESEARCH Lawrence S. Honig, MD, PhD, FAAN Department of Neurology, Taub Institute for Research on Alzheimer’s Disease & the Aging Brain, Gertrude H. Sergievsky Center, and New York State Center of Excellence for Alzheimer’s Disease Columbia University Irving Medical Center / New York Presbyterian Hospital DISCLOSURES Consultant: Eisai, Miller Communications Recent Research Funding: Abbvie, Axovant, Biogen, Bristol-Myer Squibb, Eisai, Eli Lilly, Genentech, Roche, TauRx Share Holder: none I will discuss investigational drugs, and off-label usage of drugs. 2 ALZHEIMER’S DISEASE Research in Epidemiology ALZHEIMER’S RISK FACTORS AGE Education Gender Head Trauma? Diet? Exercise? Hypertension? Hyperlipidemia? Diabetes? Evans DA JAMA 1989; 262:2551-6 Cardiovascular or Cerebrovascular Disease? GENETICS ALZHEIMER’S GENETIC FACTORS Early-onset autosomal dominant disorders APP, PS1, PS2 : (<0.1% of patients) Late-onset risk factors AD Neuropathology Change (ADNC) % e4neg %e4pos N APOE-e4 Low ADNC 73% 27% 367 Intermediate ADNC 57% 43% 429 High ADNC 39% 61% 1097 SORL1, CLU, CR1, BIN1, PICALM, EXOC3L2, ABCA7, CD2AP, EPHA1, TREM2 + >20 others! Late onset protective factors APP Icelandic mutation (A673T) ALZHEIMER’S DISEASE Research in Diagnostics EXAMINATION: General, Neurological, Cognitive, Lab, MRI Consciousness Attention and concentration Language: expression, comprehension, naming, repetition Orientation to time, place, and person Memory functions: immediate, short-term, long-term Visuospatial abilities: drawing Analytic abilities Judgment and Insight Positron Emission Tomography-FDG AMYLOID IMAGING CC Rowe & VL Villemagne. J Nuc Med 2011; 52:1733-1740 TAU SYNAPTIC IMAGING IMAGING Normal MCI/AD UCB1017 Chen et al. JAMA Neurol 2018 Villemagne VL et al. Sem Nuc Med 2017;47:75-88 CEREBROSPINAL FLUID JR Steinerman & LS Honig. -

5Th Conference Clinical Trials on Alzheimer's Disease
The Journal of Nutrition, Health & Aging© 5th Conference Clinical Trials on Alzheimer’s Disease October 29-31, 2012 Grimaldi Forum, Convention Center, Monte Carlo TH requirements in the U.S. and Europe for demonstrating disease- MONDAY, OCTOBER 29 modification in early Alzheimer’s disease; • Identify whether these differences are scientifically based or influenced by the cultural factors SYMPOSIUM within the regulatory bodies; and • Call for harmonization of current requirements that are not deemed scientifically based and propose a S1 - HARMONIZING REGULATORY REQUIREMENTS TO mechanism for collaboration among global regulatory bodies beyond BENEFIT FUTURE ALZHEIMER’ DISEASE PATIENTS. the U.S. and Europe to harmonize the issuance of new guidelines or D. PERRY1, D. STEPHENSON2, R. KATZ3, K. BROICH4 (1. ACT-AD requirements for Alzheimer’s disease. Conclusion: Alzheimer’s Coalition, Alliance for Aging Research, USA; 2. Coalition Against disease is one of the most important health challenges in the world Major Diseases, Critical Path Institute, USA; 3. U.S. Food and Drug today. The World Health Organization in April 2012 called for Administration; 4. Federal Institute for Drugs and Medical Devices nations to address dementia as a public health priority. Pursuing a (BfArM)) global consensus on regulatory requirements for the approval of early Alzheimer’s disease treatments is a timely topic and could have a The coalition to Accelerate Cure/Treatments for Alzheimer’s significant impact on advancing drug development. CTAD has become Disease (ACT-AD) is comprised of more than 50 not-for-profit a leading forum for international experts to engage in exchanges about organizations representing Alzheimer’s patients, caregivers, older opportunities and challenges for research and development across the people, health care providers and researchers. -

New Perspectives for the Treatment of Alzheimer's Disease
The Open Geriatric Medicine Journal, 2008, 1, 33-42 33 Open Access New Perspectives for the Treatment of Alzheimer’s Disease Daniela Galimberti* and Elio Scarpini Department of Neurological Sciences, "Dino Ferrari" Center, University of Milan, IRCCS Fondazione Ospedale Mag- giore Policlinico, Via F. Sforza 35, 20122, Milan, Italy Abstract: The hallmark pathologic lesions of Alzheimer’s disease (AD) are extracellular senile plaques, composed by Amiloid (A) peptide and intraneuronal neurofibrillary tangles, made of tau protein. According to the amyloid hypothe- sis, the increased production or decreased clearance of A peptide initiates a pathological process leading to neurodegen- eration, dementia and death. Under normal circumstances, the Amyloid Precursor Protein (APP) is cleaved by secretase, but, in pathological conditions, it is cleaved first by secretase (BACE) and subsequently by -secretase, to form A42 toxic peptide. Accumulation of A42 starts a cascade of events associated with neuronal and synaptic dys- function, inflammatory responses, hyperphosphorylation of tau protein and neuronal death. This theory identifies biologi- cal targets for disease-modifying treatments, including the modulation of APP metabolism, the reduction of A aggrega- tion or the enhancement of A clearance, and the reduction of inflammation. Regarding secretases, different approaches are under evaluation, primarily aiming to decrease - and -secretase. A promising approach is the modulation of A, with either vaccination or antiaggregation agents. Regarding inflammation, despite trials with Rofecoxib, Naproxen or Di- clofenac failed to slow progression of cognitive decline in patients with AD, Indomethacin showed positive results in de- laying cognitive decline. However, gastrointestinal toxicity was treatment-limiting, therefore other compounds have been developed, including Nitroflurbiprofen. -
Effect of Tarenflurbil on Cognitive Decline and Activities of Daily Living in Patients with Mild Alzheimer Disease a Randomized Controlled Trial
ORIGINAL CONTRIBUTION Effect of Tarenflurbil on Cognitive Decline and Activities of Daily Living in Patients With Mild Alzheimer Disease A Randomized Controlled Trial Robert C. Green, MD, MPH   Context Amyloid- peptide (A 42) has been implicated in the pathogenesis of Alz-  Lon S. Schneider, MD heimer disease (AD). Tarenflurbil, a selective A 42-lowering agent, demonstrated en- David A. Amato, PhD couraging results on cognitive and functional outcomes among mildly affected pa- tients in an earlier phase 2 trial. Andrew P. Beelen, MD Objective To determine the efficacy, safety, and tolerability of tarenflurbil. Gordon Wilcock, MD Design, Setting, and Patients A multicenter, randomized, double-blind, placebo- Edward A. Swabb, MD, PhD controlled trial enrolling patients with mild AD was conducted at 133 trial sites in the Kenton H. Zavitz, PhD United States between February 21, 2005, and April 30, 2008. Concomitant treat- ment with cholinesterase inhibitors or memantine was permitted. for the Tarenflurbil Phase 3 Study Group Intervention Tarenflurbil, 800 mg, or placebo, administered twice a day. Main Outcome Measures Co-primary efficacy end points were the change from EADING THEORIES ON THE PATHO- baseline to month 18 in total score on the subscale of the Alzheimer Disease Assess- physiology of Alzheimer disease ment Scale−Cognitive Subscale (ADAS-Cog, 80-point version) and Alzheimer Disease (AD) implicate overproduction of Cooperative Studies–activities of daily living (ADCS-ADL) scale. Additional prespeci- amyloid- (A), particularly 42 fied slope analyses explored the possibility of disease modification.  1-3 Lamino acid peptide A 42. Com- Results Of the 1684 participants randomized, 1649 were included in the analysis, and pounds modulating ␥-secretase en- 1046 completed the trial. -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data.