Intervertebral Disk Disease
Total Page:16
File Type:pdf, Size:1020Kb
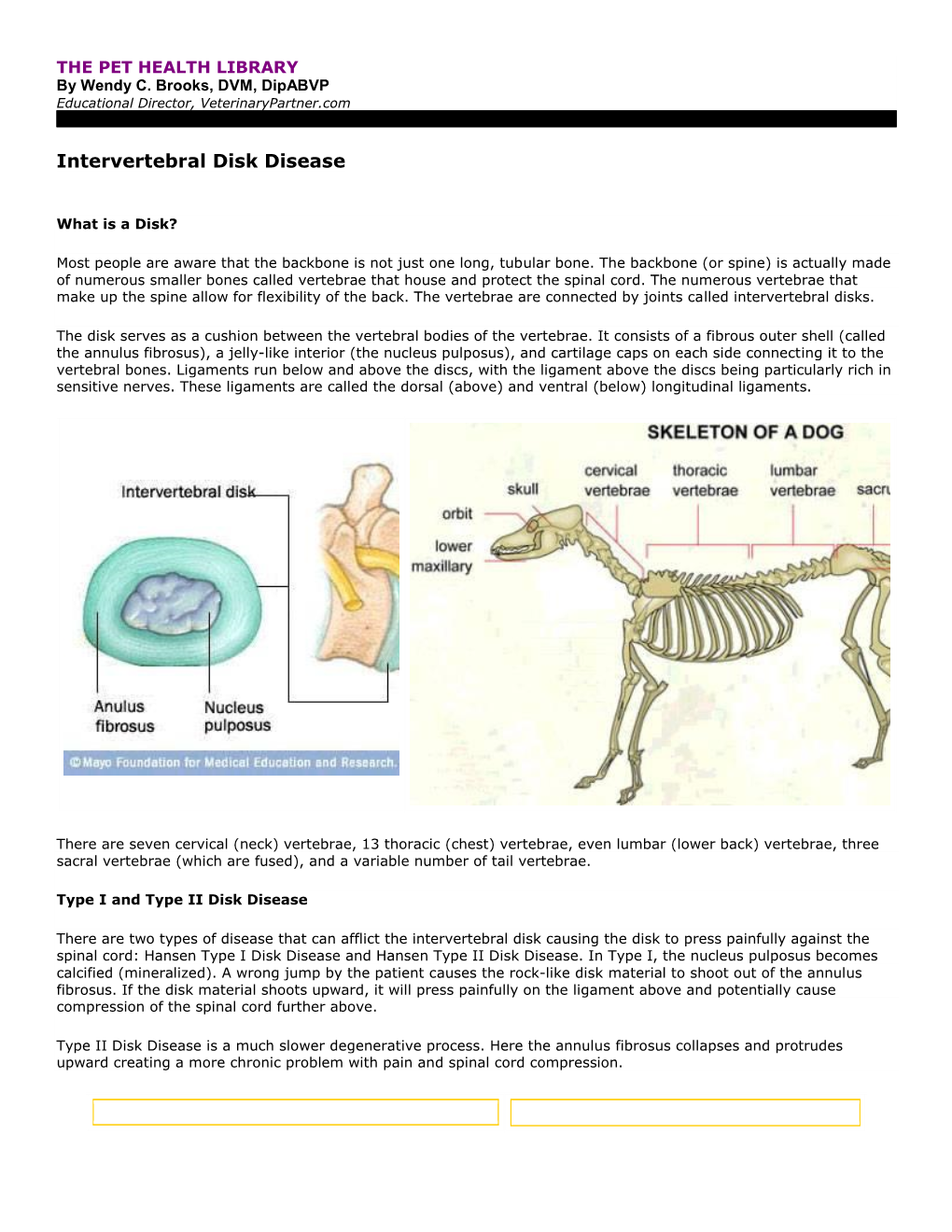
Load more
Recommended publications
-

Relationships Between Play and Responses to Tickling in Male Juvenile Rats
Scotland's Rural College Relationships between play and responses to tickling in male juvenile rats Hammond, TJH; Bombail, Vincent; Nielsen, Birte L; Meddle, Simone L; Lawrence, AB; Brown, Sarah M Published in: Applied Animal Behaviour Science DOI: 10.1016/j.applanim.2019.104879 Print publication: 01/12/2019 Document Version Peer reviewed version Link to publication Citation for pulished version (APA): Hammond, TJH., Bombail, V., Nielsen, B. L., Meddle, S. L., Lawrence, AB., & Brown, S. M. (2019). Relationships between play and responses to tickling in male juvenile rats. Applied Animal Behaviour Science, 221, [104879]. https://doi.org/10.1016/j.applanim.2019.104879 General rights Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. • Users may download and print one copy of any publication from the public portal for the purpose of private study or research. • You may not further distribute the material or use it for any profit-making activity or commercial gain • You may freely distribute the URL identifying the publication in the public portal ? Take down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. Download date: 05. Oct. 2021 Journal Pre-proof Relationships between play and responses -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

GLOSSARY of MEDICAL and ANATOMICAL TERMS
GLOSSARY of MEDICAL and ANATOMICAL TERMS Abbreviations: • A. Arabic • abb. = abbreviation • c. circa = about • F. French • adj. adjective • G. Greek • Ge. German • cf. compare • L. Latin • dim. = diminutive • OF. Old French • ( ) plural form in brackets A-band abb. of anisotropic band G. anisos = unequal + tropos = turning; meaning having not equal properties in every direction; transverse bands in living skeletal muscle which rotate the plane of polarised light, cf. I-band. Abbé, Ernst. 1840-1905. German physicist; mathematical analysis of optics as a basis for constructing better microscopes; devised oil immersion lens; Abbé condenser. absorption L. absorbere = to suck up. acervulus L. = sand, gritty; brain sand (cf. psammoma body). acetylcholine an ester of choline found in many tissue, synapses & neuromuscular junctions, where it is a neural transmitter. acetylcholinesterase enzyme at motor end-plate responsible for rapid destruction of acetylcholine, a neurotransmitter. acidophilic adj. L. acidus = sour + G. philein = to love; affinity for an acidic dye, such as eosin staining cytoplasmic proteins. acinus (-i) L. = a juicy berry, a grape; applied to small, rounded terminal secretory units of compound exocrine glands that have a small lumen (adj. acinar). acrosome G. akron = extremity + soma = body; head of spermatozoon. actin polymer protein filament found in the intracellular cytoskeleton, particularly in the thin (I-) bands of striated muscle. adenohypophysis G. ade = an acorn + hypophyses = an undergrowth; anterior lobe of hypophysis (cf. pituitary). adenoid G. " + -oeides = in form of; in the form of a gland, glandular; the pharyngeal tonsil. adipocyte L. adeps = fat (of an animal) + G. kytos = a container; cells responsible for storage and metabolism of lipids, found in white fat and brown fat. -

Required List of Bones and Markings
REQUIRED LIST OF BONES AND MARKINGS Axial Skeleton Skull Cranial Bones (8) Frontal Bone (1) Supraorbital foramina Supraorbital ridges or margins Parietal Bones (2) Temporal Bones (2) External auditory meatus Mastoid process Styloid process Zygomatic process Mandibular fossa Foramen lacerum Carotid foramen Jugular foramen Stylomastoid foramen Internal auditory meatus Occipital Bone (1) Foramen magnum Occipital condyles Ethmoid Bone (1) Cribriform plate Olfactory foramina in cribriform plate Crista galli Perpendicular plate (forms superior part of nasal septum) Middle nasal concha Superior nasal concha Sphenoid Bone (1) Foramen ovale Foramen rotundum Sella turcica Greater wing Lesser wing Optic foramen Inferior orbital fissure Superior orbital fissure Pterygoid processes Skull (cont’d) Facial Bones (14) Lacrimal Bones (2) Lacrimal fossa Nasal Bones (2) Inferior Nasal Conchae (2) Vomer (1) (forms inferior portion of nasal septum) Zygomatic Bones (2) Temporal process (forms zygomatic arch with zygomatic process of temporal bone) Maxillae (2) Alveoli Palatine process (forms anterior part of hard palate) Palatine Bones (2) (form posterior part of hard palate) Mandible (1) Alveoli Body Mental foramen Ramus Condylar process (mandibular condyle) Coronoid process Miscellaneous (Skull) Paranasal sinuses are located in the ethmoid bone, sphenoid bone, frontal bone, and maxillae Zygomatic arch (“cheekbone”) is composed of the zygomatic process of the temporal bone and the temporal process of the zygomatic bone 2 pairs of nasal conchae (superior and middle) are part of the ethmoid bone. 1 pair (inferior) are separate facial bones. All the scroll-like conchae project into the lateral walls of the nasal cavity. Hard palate (“roof of mouth”) is composed of 2 palatine processes of the maxillae and the 2 palatine bones (total of 4 fused bones). -

Lumbarisation of the First Sacral Vertebra a Rare Form of Lumbosacral Transitional Vertebra
Int. J. Morphol., 33(1):48-50, 2015. Lumbarisation of the First Sacral Vertebra a Rare Form of Lumbosacral Transitional Vertebra Lumbarización de la Primera Vertebra Sacra: Rara Forma de Una Vertebra de Transición Lumbosacral Mallikarjun Adibatti* & Asha, K.** ADIBATTI, M. & ASHA, K. Lumbarisation of the first sacral vertebra a rare form of lumbosacral transitional vertebra. Int. J. Morphol., 33(1):48-50, 2015. SUMMARY: In the lumbosacral region, anatomical variations occur with changes in the number of sacral vertebra either by deletion of first sacral vertebra or by the union of fifth lumbar or first coccygeal vertebra with sacrum. Lumbasacral transitional vertebrae (LSTV) is the most common congenital anomalies of the lumbosacral region. It most commonly involves the fifth lumbar vertebra showing signs of fusion to the sacrum known as sacralisation or the first sacral vertebra shows signs of transition to a lumbar configuration commonly known as lumbarisation. Complete transition can result in numerical abnormalities of the lumbar and sacral vertebral segments. Lumbarisation of first sacral vertebra is seen with a very low incidence of 2%. Knowledge of presence of such vertebral variation will be helpful for the clinicians to diagnose and treat patients with low back pain. Although sacralisation of fifth lumbar vertebrae is most commonly seen when compared to lumbarisation of first sacral vertebrae, we report here a case of lumbarisation of first sacral vertebrae for its rarity among the LSTV and clinical implications. KEY WORDS: Vertebrae; Sacrum; Sacralisation; Lumbarisation; Transitional vertebrae. INTRODUCTION RESULTS The sacrum is formed by the fusion of five sacral During routine Osteology classes, we observed the vertebras. -

FEM-Based Compression Fracture Risk Assessment in Osteoporotic Lumbar Vertebra L1
Article FEM-Based Compression Fracture Risk Assessment in Osteoporotic Lumbar Vertebra L1 Algirdas Maknickas 1,* , Vidmantas Alekna 2 , Oleg Ardatov 1 , Olga Chabarova 3 , Darius Zabulionis 4 , Marija Tamulaitiene˙ 2 and Rimantas Kaˇcianauskas 1,4 1 Institute of Mechanics, Vilnius Gediminas Technical University, 03224 Vilnius, Lithuania 2 Faculty of Medicine, Vilnius University, 03101 Vilnius, Lithuania 3 Department of Applied Mechanics, Vilnius Gediminas Technical University, 10223 Vilnius, Lithuania 4 Department of Information Systems, Vilnius Gediminas Technical University, 10223 Vilnius, Lithuania * Correspondence: [email protected] Received: 27 June 2019; Accepted: 24 July 2019; Published: 26 July 2019 Abstract: This paper presents a finite element method (FEM)-based fracture risk assessment in patient-specific osteoporotic lumbar vertebra L1. The influence of osteoporosis is defined by variation of parameters such as thickness of the cortical shell, the bone volume–total volume ratio (BV/TV), and the trabecular bone score (TBS). The mechanical behaviour of bone is defined using the Ramberg–Osgood material model. This study involves the static and nonlinear dynamic calculations of von Mises stresses and follows statistical processing of the obtained results in order to develop the patient-specific vertebra reliability. In addition, different scenarios of parameters show that the reliability of the proposed model of human vertebra highly decreases with low levels of BV/TV and is critical due to the thinner cortical bone, suggesting high trauma risk by reason of osteoporosis. Keywords: bone tissue; elastoplasticity; finite element method; fracture risk; osteoporosis; trabeculae; trabecular bone score; vertebra 1. Introduction Spinal bones can be affected by several diseases, but spinal brittleness is mainly caused by osteoporosis. -

Vertebral Column
Vertebral Column • Backbone consists of Cervical 26 vertebrae. • Five vertebral regions – Cervical vertebrae (7) Thoracic in the neck. – Thoracic vertebrae (12) in the thorax. – Lumbar vertebrae (5) in the lower back. Lumbar – Sacrum (5, fused). – Coccyx (4, fused). Sacrum Coccyx Scoliosis Lordosis Kyphosis Atlas (C1) Posterior tubercle Vertebral foramen Tubercle for transverse ligament Superior articular facet Transverse Transverse process foramen Facet for dens Anterior tubercle • Atlas- ring of bone, superior facets for occipital condyles. – Nodding movement signifies “yes”. Axis (C2) Spinous process Lamina Vertebral foramen Transverse foramen Transverse process Superior articular facet Odontoid process (dens) •Axis- dens or odontoid process is body of atlas. – Pivotal movement signifies “no”. Typical Cervical Vertebra (C3-C7) • Smaller bodies • Larger spinal canal • Transverse processes –Shorter – Transverse foramen for vertebral artery • Spinous processes of C2 to C6 often bifid • 1st and 2nd cervical vertebrae are unique – Atlas & axis Typical Cervical Vertebra Spinous process (bifid) Lamina Vertebral foramen Inferior articular process Superior articular process Transverse foramen Pedicle Transverse process Body Thoracic Vertebrae (T1-T12) • Larger and stronger bodies • Longer transverse & spinous processes • Demifacets on body for head of rib • Facets on transverse processes (T1-T10) for tubercle of rib Thoracic Vertebra- superior view Spinous process Transverse process Facet for tubercle of rib Lamina Superior articular process -

View of the Micro-CT Data, Where the Blue and Green Marked the Spongy Structure Caused by the Cancellous Bone
Liu et al. EURASIP Journal on Image and Video EURASIP Journal on Image Processing (2019) 2019:60 https://doi.org/10.1186/s13640-019-0456-1 and Video Processing RESEARCH Open Access Mice endplate segmentation from micro-CT data through graph-based trabecula recognition Shi-Jian Liu1†, Zheng Zou2†, Jeng-Shyang Pan1,3,4* and Sheng-Hui Liao5 Abstract Though segmentation of spinal column from medical images have been intensively studied for decade, most of the works were concentrated on the segmentation of the vertebral body and arch, instead of the endplate. Recently, the increasing study on degeneration analysis of vertebra and intervertebral disc (IVD) make endplate segmentation as important as others. While the accurately segmentation of mice endplate from micro computed tomography (CT) images is challenging. The major difficulties include potential high system payload and poor run-time efficiency resulting from high-resolution micro-CT data, highly complicated and variable shape of the vertebra tissues, and the ambiguous segmentation boundary due to the similarity of spongy structures inside both the endplate and its adjacent vertebral body. To solve the problems, the core idea of the proposed method is to identify trabeculae between the endplate and the body through a graph-based strategy. In addition, in order to reduce the data complexity, an endplate-targeted region of interest (ROI) extraction method is introduced according to the analysis of spatial relationship and variety of bone density of vertebra. Furthermore, shape priori of endplate in both two-dimensional and three-dimensional are extracted to assist in the segmentation. Finally, an iterative cutting procedure is implemented to produce the final result. -

Cervical Vertebrae 1 Cervical Vertebrae
Cervical vertebrae 1 Cervical vertebrae Cervical vertebrae or Cervilar Position of human cervical vertebrae (shown in red). It consists of 7 bones, from top to bottom, C1, C2, C3, C4, C5, C6 and C7. A human cervical vertebra Latin Vertebrae cervicales [1] Gray's p.97 [2] MeSH Cervical+vertebrae [3] TA A02.2.02.001 [4] FMA FMA:72063 In vertebrates, cervical vertebrae (singular: vertebra) are those vertebrae immediately inferior to the skull. Thoracic vertebrae in all mammalian species are defined as those vertebrae that also carry a pair of ribs, and lie caudal to the cervical vertebrae. Further caudally follow the lumbar vertebrae, which also belong to the trunk, but do not carry ribs. In reptiles, all trunk vertebrae carry ribs and are called dorsal vertebrae. In many species, though not in mammals, the cervical vertebrae bear ribs. In many other groups, such as lizards and saurischian dinosaurs, the cervical ribs are large; in birds, they are small and completely fused to the vertebrae. The transverse processes of mammals are homologous to the cervical ribs of other amniotes. Cervical vertebrae 2 In humans, cervical vertebrae are the smallest of the true vertebrae, and can be readily distinguished from those of the thoracic or lumbar regions by the presence of a foramen (hole) in each transverse process, through which passes the vertebral artery. The remainder of this article focuses upon human anatomy. Structure By convention, the cervical vertebrae are numbered, with the first one (C1) located closest to the skull and higher numbered vertebrae (C2-C7) proceeding away from the skull and down the spine. -

Degenerative Spondylolisthesis
AN INTRODUCTION TO DEGENERATIVE SPONDYLOLISTHESIS This booklet is designed to inform you about lumbar degenerative spondylolisthesis. It is not meant to replace any personal conversations that you might wish to have with your physician or other member of your healthcare team. Not all the information here will apply to your individual treatment or its outcome. The information is intended to answer some of your questions and serve as a stimulus for you to ask appropriate questions about spinal alignment and spine surgery. About the Spine CERVICAL The human spine is comprised of the cervical (neck) spine, the thoracic (chest) spine, the lumbar (lower back) spine, and sacral THORACIC bones. The entire spine is made up of 24 bones, called vertebrae. These vertebrae are connected by several joints, which allow you to LUMBAR bend, twist, and carry loads. The main joint between two vertebrae is called an intervertebral disc. The disc is comprised of two parts, a tough and fibrous outer layer (annulus fibrosis) and a soft, gelatinous center (nucleus pulposus). These two parts work in conjunction to allow the spine to move, and also provide shock absorption. INTERVERTEBRAL ANNULUS DISC FIBROSIS SPINAL NERVES NUCLEUS PULPOSUS What is Degenerative Spondylolisthesis? Degenerative spondylolisthesis is a condition where the intervertebral disc degenerates resulting in a loss of disc height and instability, causing one vertebra to slip forward over another vertebra below it. The word spondylolisthesis is comprised of two parts: spondylo meaning spine, and listhesis meaning slippage. This condition can cause impingement of the spinal nerves and/or fatigue of the back muscles, and may result in lower back and/or leg pain. -

Lumbar Degenerative Disease Part 1
International Journal of Molecular Sciences Article Lumbar Degenerative Disease Part 1: Anatomy and Pathophysiology of Intervertebral Discogenic Pain and Radiofrequency Ablation of Basivertebral and Sinuvertebral Nerve Treatment for Chronic Discogenic Back Pain: A Prospective Case Series and Review of Literature 1, , 1,2, 1 Hyeun Sung Kim y * , Pang Hung Wu y and Il-Tae Jang 1 Nanoori Gangnam Hospital, Seoul, Spine Surgery, Seoul 06048, Korea; [email protected] (P.H.W.); [email protected] (I.-T.J.) 2 National University Health Systems, Juronghealth Campus, Orthopaedic Surgery, Singapore 609606, Singapore * Correspondence: [email protected]; Tel.: +82-2-6003-9767; Fax.: +82-2-3445-9755 These authors contributed equally to this work. y Received: 31 January 2020; Accepted: 20 February 2020; Published: 21 February 2020 Abstract: Degenerative disc disease is a leading cause of chronic back pain in the aging population in the world. Sinuvertebral nerve and basivertebral nerve are postulated to be associated with the pain pathway as a result of neurotization. Our goal is to perform a prospective study using radiofrequency ablation on sinuvertebral nerve and basivertebral nerve; evaluating its short and long term effect on pain score, disability score and patients’ outcome. A review in literature is done on the pathoanatomy, pathophysiology and pain generation pathway in degenerative disc disease and chronic back pain. 30 patients with 38 levels of intervertebral disc presented with discogenic back pain with bulging degenerative intervertebral disc or spinal stenosis underwent Uniportal Full Endoscopic Radiofrequency Ablation application through either Transforaminal or Interlaminar Endoscopic Approaches. Their preoperative characteristics are recorded and prospective data was collected for Visualized Analogue Scale, Oswestry Disability Index and MacNab Criteria for pain were evaluated. -

''Laughing'' Rats and the Evolutionary Antecedents of Human Joy?
Physiology & Behavior 79 (2003) 533–547 ‘‘Laughing’’ rats and the evolutionary antecedents of human joy? Jaak Pankseppa,b,*, Jeff Burgdorf a aDepartment of Psychology, J.P. Scott Center for Neuroscience, Mind and Behavior, Bowling Green State University, Bowling Green, OH 43403, USA bFalk Center for Molecular Therapeutics, Northwestern University Research Park, 1801 Maple Avenue, Suite 4306, Evanston, IL 60201, USA Received 4 April 2003; accepted 17 April 2003 Abstract Paul MacLean’s concept of epistemics—the neuroscientific study of subjective experience—requires animal brain research that can be related to predictions concerning the internal experiences of humans. Especially robust relationships come from studies of the emotional/ affective processes that arise from subcortical brain systems shared by all mammals. Recent affective neuroscience research has yielded the discovery of play- and tickle-induced ultrasonic vocalization patterns ( 50-kHz chirps) in rats may have more than a passing resemblance to primitive human laughter. In this paper, we summarize a dozen reasons for the working hypothesis that such rat vocalizations reflect a type of positive affect that may have evolutionary relations to the joyfulness of human childhood laughter commonly accompanying social play. The neurobiological nature of human laughter is discussed, and the relevance of such ludic processes for understanding clinical disorders such as attention deficit hyperactivity disorders (ADHD), addictive urges and mood imbalances are discussed. D 2003 Published