Human B Lymphocytes and Autocrine
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Type I Interferons and the Development of Impaired Vascular Function and Repair in Human and Murine Lupus
Type I Interferons and the Development of Impaired Vascular Function and Repair in Human and Murine Lupus by Seth G Thacker A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy (Immunology) in The University of Michigan 2011 Doctoral Committee: Associate Professor Mariana J. Kaplan, Chair Professor David A. Fox Professor Alisa E. Koch Professor Matthias Kretzler Professor Nicholas W. Lukacs Associate Professor Daniel T. Eitzman © Seth G Thacker 2011 Sharon, this work is dedicated to you. This achievement is as much yours as it is mine. Your support through all six years of this Ph.D. process has been incredible. You put up with my countless miscalculations on when I would finish experiments, and still managed to make me and our kids feel loved and special. Without you this would have no meaning. Sharon, you are the safe harbor in my life. ii Acknowledgments I have been exceptionally fortunate in my time here at the University of Michigan. I have been able to interact with so many supportive people over the years. I would like to express my thanks and admiration for my mentor. Mariana has taught me so much about writing, experimental design and being a successful scientist in general. I could never have made it here without her help. I would also like to thank Mike Denny. He had a hand in the beginning of all of my projects in one way or another, and was always quick and eager to help in whatever way he could. He really made my first year in the lab successful. -

Levels of Interleukin-2, Interferon- , and Interleukin-4 In
Levels of Interleukin-2, Interferon-␥, and Interleukin-4 in Bronchoalveolar Lavage Fluid From Patients With Mycoplasma Pneumonia: Implication of Tendency Toward Increased Immunoglobulin E Production Young Yull Koh, MD*; Yang Park, MD*; Hoan Jong Lee, MD*; and Chang Keun Kim, MD‡ ABSTRACT. Objective. In connection with the possi- ABBREVIATIONS. IgE, immunoglobulin E; TH1, T helper type 1; ble relationship between Mycoplasma infection and the TH2, T helper type 2; IFN, interferon; IL, interleukin; BAL, bron- onset of asthma, several studies have shown not only a choalveolar lavage; FB, fiber-optic bronchoscopy; SD, standard high level of serum total immunoglobulin E (IgE) but deviation. also the production of IgE specific to Mycoplasma or common allergens during the course of Mycoplasma in- fection. It has been suggested that the balance of T helper esults of several studies over the past decade type 1 (TH1)/T helper type 2 (TH2) immune response have provided evidence linking Mycoplasma may regulate the synthesis of IgE. The objective of this Rinfection with asthma exacerbation and have study was to investigate the pattern of cytokine response raised the possibility that Mycoplasma infection is a (TH1 or TH2) during an episode of acute lower respira- factor in the pathogenesis of asthma. An acute exac- tory tract infection caused by Mycoplasma pneumoniae. erbation of wheezing in asthmatic participants in Study Design. Using a bronchoalveolar lavage (BAL) association with Mycoplasma infection has been well- with flexible bronchoscopy procedure, this study deter- 1,2 mined the levels of interleukin (IL)-2, interferon (IFN)-␥ documented. In addition, Mycoplasma pneumoniae (TH1), and IL-4 (TH2) in the supernatant of BAL fluid as has been found in the lower airways of chronic, well as the BAL cellular profiles of patients with Myco- stable asthmatics with a greater frequency than in -These results were com- control participants,3 suggesting a pathogenic mech .(14 ؍ plasma pneumonia (n pared with those of patients with pneumococcal pneu- anism in chronic asthma. -

Modulation of the Inflammatory Response After Spinal Cord Injury
ADVERTIMENT. Lʼaccés als continguts dʼaquesta tesi queda condicionat a lʼacceptació de les condicions dʼús establertes per la següent llicència Creative Commons: http://cat.creativecommons.org/?page_id=184 ADVERTENCIA. El acceso a los contenidos de esta tesis queda condicionado a la aceptación de las condiciones de uso establecidas por la siguiente licencia Creative Commons: http://es.creativecommons.org/blog/licencias/ WARNING. The access to the contents of this doctoral thesis it is limited to the acceptance of the use conditions set by the following Creative Commons license: https://creativecommons.org/licenses/?lang=en MODULATION OF THE INFLAMMATORY RESPONSE AFTER SPINAL CORD INJURY Presented by Jesús Amo Aparicio ACADEMIC DISSERTATION To obtain the degree of PhD in Neuroscience by the Universitat Autònoma de Barcelona 2019 Directed by Dr. Rubèn López Vales Tutorized by Dr. Xavier Navarro Acebes INDEX SUMMARY Page 7 INTRODUCTION Page 13 - Spinal cord Page 15 - Spinal cord injury Page 17 - Incidence and causes Page 18 - Types of SCI Page 18 - Biological events after SCI Page 20 - Studying SCI Page 24 - Animal models Page 24 - Lesion models Page 24 - Current therapies for SCI Page 25 - Basic principles of the immune system Page 27 - Innate immune response Page 27 - Adaptive immune response Page 28 - Inflammatory response Page 29 - Inflammatory response after SCI Page 30 - Modulation of injury environment Page 36 - Interleukin 1 Page 36 - Interleukin 37 Page 40 - Interleukin 13 Page 44 OBJECTIVES Page 47 MATERIALS AND METHODS Page 51 -

IL-1Β Induces the Rapid Secretion of the Antimicrobial Protein IL-26 From
Published June 24, 2019, doi:10.4049/jimmunol.1900318 The Journal of Immunology IL-1b Induces the Rapid Secretion of the Antimicrobial Protein IL-26 from Th17 Cells David I. Weiss,*,† Feiyang Ma,†,‡ Alexander A. Merleev,x Emanual Maverakis,x Michel Gilliet,{ Samuel J. Balin,* Bryan D. Bryson,‖ Maria Teresa Ochoa,# Matteo Pellegrini,*,‡ Barry R. Bloom,** and Robert L. Modlin*,†† Th17 cells play a critical role in the adaptive immune response against extracellular bacteria, and the possible mechanisms by which they can protect against infection are of particular interest. In this study, we describe, to our knowledge, a novel IL-1b dependent pathway for secretion of the antimicrobial peptide IL-26 from human Th17 cells that is independent of and more rapid than classical TCR activation. We find that IL-26 is secreted 3 hours after treating PBMCs with Mycobacterium leprae as compared with 48 hours for IFN-g and IL-17A. IL-1b was required for microbial ligand induction of IL-26 and was sufficient to stimulate IL-26 release from Th17 cells. Only IL-1RI+ Th17 cells responded to IL-1b, inducing an NF-kB–regulated transcriptome. Finally, supernatants from IL-1b–treated memory T cells killed Escherichia coli in an IL-26–dependent manner. These results identify a mechanism by which human IL-1RI+ “antimicrobial Th17 cells” can be rapidly activated by IL-1b as part of the innate immune response to produce IL-26 to kill extracellular bacteria. The Journal of Immunology, 2019, 203: 000–000. cells are crucial for effective host defense against a wide and neutrophils. -

The Cross-Talk Between Neurons and Microglia Through Interleukin-4 After Ischemic Injury
The Texas Medical Center Library DigitalCommons@TMC The University of Texas MD Anderson Cancer Center UTHealth Graduate School of The University of Texas MD Anderson Cancer Biomedical Sciences Dissertations and Theses Center UTHealth Graduate School of (Open Access) Biomedical Sciences 8-2018 The Cross-Talk Between Neurons and Microglia Through Interleukin-4 After Ischemic Injury Shun-Ming Ting Follow this and additional works at: https://digitalcommons.library.tmc.edu/utgsbs_dissertations Part of the Medicine and Health Sciences Commons Recommended Citation Ting, Shun-Ming, "The Cross-Talk Between Neurons and Microglia Through Interleukin-4 After Ischemic Injury" (2018). The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences Dissertations and Theses (Open Access). 892. https://digitalcommons.library.tmc.edu/utgsbs_dissertations/892 This Thesis (MS) is brought to you for free and open access by the The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences at DigitalCommons@TMC. It has been accepted for inclusion in The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences Dissertations and Theses (Open Access) by an authorized administrator of DigitalCommons@TMC. For more information, please contact [email protected]. THE CROSS-TALK BETWEEN NEURONS AND MICROGLIA THROUGH INTERLEUKIN-4 AFTER ISCHEMIC INJURY by Shun-Ming Ting, M.S. APPROVED: ______________________________ Jaroslaw Aronowski, Ph.D. Advisory -

IL-7) and IL-7 Splice Variants Affect Differentiation of Human Neural Progenitor Cells
Genes and Immunity (2010) 11, 11–20 & 2010 Macmillan Publishers Limited All rights reserved 1466-4879/10 $32.00 www.nature.com/gene ORIGINAL ARTICLE Interleukin-7 (IL-7) and IL-7 splice variants affect differentiation of human neural progenitor cells M Moors1,4, NK Vudattu2,, J Abel1, U Kra¨mer1, L Rane2, N Ulfig3, S Ceccatelli4, V Seyfert-Margolies5, E Fritsche1 and MJ Maeurer2 1Group of Toxicology, Group of Epidemiology, Institut fu¨r Umweltmedizinische Forschung, Du¨sseldorf, Germany; 2Microbiology, Tumor and Cell Biology and Smittskyddsinstitutet, Stockholm, Sweden; 3Department of Anatomy, University of Rostock, Rostock, Germany; 4Division of Neurotoxicology, Department of Neuroscience, Karolinska Institutet, Sweden and 5Department of Medicine, University of California, San Francisco, CA, USA Alternative splicing of pre-mRNA increases proteomic diversity, a crucial mechanism in defining tissue identity. We demonstrate differentially spliced interleukin (IL)-7 in distinct anatomic areas in the adult, in developing human brains and in normal human neuronal progenitor (NHNP) cells. IL-7c (c, the canonical form spanning all six exons) or its variants IL-7d5, d4 or d4/5 were cloned and expressed as recombinant proteins. IL-7 and splice variants were able to shift the differentiation of NHNP cells as compared with the diluent control (Po0.01) defined by anti-b (III)-tubulin and glial fibrillary acidic protein expression, with different degrees (IL-7c4d4/54IL-7d5); IL-7d4 exhibited a significantly weaker potency. Differentiation was confirmed by transcriptome analysis of IL-7c-stimulated neural NHNP cells, resulting in 58 differentially expressed genes; some of these are involved in neural differentiation, for example, the developmentally regulated transcription factor kru¨ppel-like factor 12, musashi 2, a translational regulator of cell fate or the sonic hedgehog receptor patch 1. -
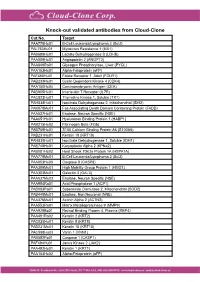
Knock-Out Validated Antibodies from Cloud-Clone Cat.No
Knock-out validated antibodies from Cloud-Clone Cat.No. Target PAA778Hu01 B-Cell Leukemia/Lymphoma 2 (Bcl2) PAL763Hu01 Myxovirus Resistance 1 (MX1) PAB698Hu01 Lactate Dehydrogenase B (LDHB) PAA009Hu01 Angiopoietin 2 (ANGPT2) PAA849Ra01 Glycogen Phosphorylase, Liver (PYGL) PAA153Hu01 Alpha-Fetoprotein (aFP) PAF460Hu01 Folate Receptor 1, Adult (FOLR1) PAB233Hu01 Cyclin Dependent Kinase 4 (CDK4) PAA150Hu04 Carcinoembryonic Antigen (CEA) PAB905Hu01 Interleukin 7 Receptor (IL7R) PAC823Hu01 Thymidine Kinase 1, Soluble (TK1) PAH838Hu01 Isocitrate Dehydrogenase 2, mitochondrial (IDH2) PAK078Mu01 Fas Associating Death Domain Containing Protein (FADD) PAA537Hu01 Enolase, Neuron Specific (NSE) PAA651Hu01 Hyaluronan Binding Protein 1 (HABP1) PAB215Hu02 Fibrinogen Beta (FGb) PAB769Hu01 S100 Calcium Binding Protein A6 (S100A6) PAB231Hu01 Keratin 18 (KRT18) PAH839Hu01 Isocitrate Dehydrogenase 1, Soluble (IDH1) PAE748Hu01 Karyopherin Alpha 2 (KPNa2) PAB081Hu02 Heat Shock 70kDa Protein 1A (HSPA1A) PAA778Mu01 B-Cell Leukemia/Lymphoma 2 (Bcl2) PAA853Hu03 Caspase 8 (CASP8) PAA399Mu01 High Mobility Group Protein 1 (HMG1) PAA303Mu01 Galectin 3 (GAL3) PAA537Mu02 Enolase, Neuron Specific (NSE) PAA994Ra01 Acid Phosphatase 1 (ACP1) PAB083Ra01 Superoxide Dismutase 2, Mitochondrial (SOD2) PAB449Mu01 Enolase, Non Neuronal (NNE) PAA376Mu01 Actinin Alpha 2 (ACTN2) PAA553Ra01 Matrix Metalloproteinase 9 (MMP9) PAA929Bo01 Retinol Binding Protein 4, Plasma (RBP4) PAA491Ra02 Keratin 2 (KRT2) PAC025Hu01 Keratin 8 (KRT8) PAB231Mu01 Keratin 18 (KRT18) PAC598Hu03 Vanin 1 (VNN1) -

Phase I Study of Recombinant Human Interleukin-7 Administration in Subjects with Refractory Malignancy
Published OnlineFirst January 12, 2010; DOI: 10.1158/1078-0432.CCR-09-1303 Cancer Therapy: Clinical Clinical Cancer Research Phase I Study of Recombinant Human Interleukin-7 Administration in Subjects with Refractory Malignancy Claude Sportès1, Rebecca R. Babb1, Michael C. Krumlauf1, Frances T. Hakim1, Seth M. Steinberg2, Catherine K. Chow5, Margaret R. Brown6, Thomas A. Fleisher6, Pierre Noel6, Irina Maric6, Maryalice Stetler-Stevenson3, Julie Engel7, Renaud Buffet7, Michel Morre7, Robert J. Amato8, Andrew Pecora9, Crystal L. Mackall4, and Ronald E. Gress1 Abstract Purpose: Interleukin-7 (IL-7) has critical and nonredundant roles in T-cell development, hematopoi- esis, and postdevelopmental immune functions as a prototypic homeostatic cytokine. Based on a large body of preclinical evidence, it may have multiple therapeutic applications in immunodeficiency states, either physiologic (immunosenescence), pathologic (HIV), or iatrogenic (postchemotherapy and posthe- matopoietic stem cell transplant), and may have roles in immune reconstitution or enhancement of im- munotherapy. We report here on the toxicity and biological activity of recombinant human IL-7 (rhIL-7) in humans. Design: Subjects with incurable malignancy received rhIL-7 subcutaneously every other day for 2 weeks in a phase I interpatient dose escalation study (3, 10, 30, and 60 μg/kg/dose). The objectives were safety and dose-limiting toxicity determination, identification of a range of biologically active doses, and char- acterization of biological and, possibly, antitumor effects. Results: Mild to moderate constitutional symptoms, reversible spleen and lymph node enlargement, and marked increase in peripheral CD3+, CD4+, and CD8+ lymphocytes were seen in a dose-dependent and age-independent manner in all subjects receiving ≥10 μg/kg/dose, resulting in a rejuvenated circulat- ing T-cell profile, resembling that seen earlier in life. -

Evolutionary Divergence and Functions of the Human Interleukin (IL) Gene Family Chad Brocker,1 David Thompson,2 Akiko Matsumoto,1 Daniel W
UPDATE ON GENE COMPLETIONS AND ANNOTATIONS Evolutionary divergence and functions of the human interleukin (IL) gene family Chad Brocker,1 David Thompson,2 Akiko Matsumoto,1 Daniel W. Nebert3* and Vasilis Vasiliou1 1Molecular Toxicology and Environmental Health Sciences Program, Department of Pharmaceutical Sciences, University of Colorado Denver, Aurora, CO 80045, USA 2Department of Clinical Pharmacy, University of Colorado Denver, Aurora, CO 80045, USA 3Department of Environmental Health and Center for Environmental Genetics (CEG), University of Cincinnati Medical Center, Cincinnati, OH 45267–0056, USA *Correspondence to: Tel: þ1 513 821 4664; Fax: þ1 513 558 0925; E-mail: [email protected]; [email protected] Date received (in revised form): 22nd September 2010 Abstract Cytokines play a very important role in nearly all aspects of inflammation and immunity. The term ‘interleukin’ (IL) has been used to describe a group of cytokines with complex immunomodulatory functions — including cell proliferation, maturation, migration and adhesion. These cytokines also play an important role in immune cell differentiation and activation. Determining the exact function of a particular cytokine is complicated by the influence of the producing cell type, the responding cell type and the phase of the immune response. ILs can also have pro- and anti-inflammatory effects, further complicating their characterisation. These molecules are under constant pressure to evolve due to continual competition between the host’s immune system and infecting organisms; as such, ILs have undergone significant evolution. This has resulted in little amino acid conservation between orthologous proteins, which further complicates the gene family organisation. Within the literature there are a number of overlapping nomenclature and classification systems derived from biological function, receptor-binding properties and originating cell type. -

Expression of Interleukin-4 but Not of Interleukin-10 from a Replicative Herpes Simplex Virus Type 1 Viral Vector Precludes Experimental Allergic Encephalomyelitis
Gene Therapy (2001) 8, 769–777 2001 Nature Publishing Group All rights reserved 0969-7128/01 $15.00 www.nature.com/gt RESEARCH ARTICLE Expression of interleukin-4 but not of interleukin-10 from a replicative herpes simplex virus type 1 viral vector precludes experimental allergic encephalomyelitis E Broberg1,2,3, N Seta¨la¨ 1,3,MRo¨ytta¨4, A Salmi1, J-P Era¨linna1,5,BHe6, B Roizman6 and V Hukkanen1,2 Departments of 1Virology, 4Pathology, 5Neurology and 2MediCity Research Laboratory, University of Turku, Turku; 3Turku Graduate School of Biomedical Sciences, Turku, Finland; and 6The Marjorie B Kovler Viral Oncology Laboratories, University of Chicago, Chicago, IL, USA We have used interleukin (IL)-4 and -10-producing HSV-1 any infection, mice infected with backbone virus R3659 and ␥ 134.5 deletion viruses in gene therapy of a BALB/c model mock-infected mice. Weights and symptoms of the mice of experimental allergic encephalomyelitis (EAE), a T cell- were recorded daily and the tissue specimens were col- mediated demyelinating disease of the central nervous sys- lected at specific time-points. The results indicate that the tem. It is known that in EAE of mice the Th2-type cytokines intracranial infection with IL-4-producing virus (1) precludes are down-regulated and the Th1-type cytokines up-regulated EAE symptoms, (2) protects the spinal cord from massive during the onset and relapse of the disease. Therefore, we leukocyte infiltrations and (3) prevents demyelination and tested two HSV-1 recombinants expressing the Th2-type axonal loss. The IL-10-expressing virus R8308 did not have cytokines IL-4 and IL-10. -

Illuminating the Source of in Vivo Interleukin-7
DOI 10.4110/in.2011.11.1.1 REVIEW ARTICLE pISSN 1598-2629 eISSN 2092-6685 Seeing Is Believing: Illuminating the Source of In Vivo Interleukin-7 Grace Yoonhee Kim1,2,3, Changwan Hong1 and Jung-Hyun Park1* 1Experimental Immunology Branch, National Cancer Institute, National Institutes of Health, Bethesda, MD, 2Howard Hughes Medical Institute-NIH Research Scholars Program, Bethesda, MD, 3The Johns Hopkins University School of Medicine, Baltimore, MD, USA Interleukin-7 (IL-7) is an essential cytokine for T cells. INTRODUCTION However, IL-7 is not produced by T cells themselves such that T cells are dependent on extrinsic IL-7. In fact, in the ab- Originally described as a pre-B cell growth factor expressed sence of IL-7, T cell development in the thymus as well as in bone marrow stromal cells (1), interleukin-7 (IL-7) was survival of naive T cells in the periphery is severely impaired. subsequently identified as an essential and non-redundant cy- Furthermore, modulating IL-7 availability in vivo either by ge- tokine in T cells (2,3). In fact, IL-7 plays a critical role in netic means or other experimental approaches determines every aspect of T cell biology, including early T cell develop- the size, composition and function of the T cell pool. ment in the thymus, CD4/CD8 lineage choice during positive Consequently, understanding IL-7 expression is critical for understanding T cell immunity. Until most recently, however, selection as well as maintaining the survival and homeostasis the spatiotemporal expression of in vivo IL-7 has remained of naïve and memory T cells in the periphery (2-6). -

Enhancement by Interleukin 4 of Interleukin 2- Or Antibody-Induced Proliferation of Lymphocytes from Interleukin 2-Treated Cancer Patients1
ICANCER RESEARCH 50. 1160-1 164. Februar} 15. 1990) Enhancement by Interleukin 4 of Interleukin 2- or Antibody-induced Proliferation of Lymphocytes from Interleukin 2-treated Cancer Patients1 Jonathan Treisman, Carl M. Higuchi, John A. Thompson, Steven Gillis, Catherine G. Lindgren, Donald E. Kern, Stanley R. Ridell, Philip D. Greenberg, and Alexander I efer Department of Medicine, Division of Medical Oncolog); University of Washington School of Medicine, Seattle. Has/tinglan 9X195 fJ. T., C. M. H.,J. A. T., C, G. L., D. E. K., S. R. R., P. D. G., A. F.]; and Immunex Corporation, Seattle, H'ashington 98101 [S. G.J ABSTRACT IL-2-activated cells for therapy are usually generated by ob taining PBMC from cancer patients shortly after systemic IL- Systemic interleukin 2 (IL-2) and IL-2-activated lymphocytes have 2 therapy and culturing them with IL-2 in vitro. The cells thus induced tumor regression in some cancer patients. The IL-2-activated cells have usually been generated by obtaining peripheral blood mono- generated for infusion are phenotypically and functionally het nuclear cells (PB1V1C)from cancer patients shortly after systemic IL-2 erogeneous and contain cells with LAK activity (5, 7), as well therapy and culturing them with IL-2 in vitro. In an effort to augment as other cells which may mediate or contribute to antitumor the ex vivogeneration of such cells preactivated in vivo, we examined the responses (8). In an effort to enhance the generation of such proliferative responses of PBIVIC from IL-2-treated cancer patients to cells i/i vitro, several agents which induce a proliferative re several proliferative signals including IL-2, interleukin 4 (II -4).