Usefulness of IL-21, IL-7, and IL-15 Conditioned Media for Expansion of Antigen-Specific CD8+ T Cells from Healthy Donor-Pbmcs Suitable for Immunotherapy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Type I Interferons and the Development of Impaired Vascular Function and Repair in Human and Murine Lupus
Type I Interferons and the Development of Impaired Vascular Function and Repair in Human and Murine Lupus by Seth G Thacker A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy (Immunology) in The University of Michigan 2011 Doctoral Committee: Associate Professor Mariana J. Kaplan, Chair Professor David A. Fox Professor Alisa E. Koch Professor Matthias Kretzler Professor Nicholas W. Lukacs Associate Professor Daniel T. Eitzman © Seth G Thacker 2011 Sharon, this work is dedicated to you. This achievement is as much yours as it is mine. Your support through all six years of this Ph.D. process has been incredible. You put up with my countless miscalculations on when I would finish experiments, and still managed to make me and our kids feel loved and special. Without you this would have no meaning. Sharon, you are the safe harbor in my life. ii Acknowledgments I have been exceptionally fortunate in my time here at the University of Michigan. I have been able to interact with so many supportive people over the years. I would like to express my thanks and admiration for my mentor. Mariana has taught me so much about writing, experimental design and being a successful scientist in general. I could never have made it here without her help. I would also like to thank Mike Denny. He had a hand in the beginning of all of my projects in one way or another, and was always quick and eager to help in whatever way he could. He really made my first year in the lab successful. -

Oral Tolerance: Therapeutic Implications for Autoimmune Diseases
Clinical & Developmental Immunology, June–December 2006; 13(2–4): 143–157 Oral tolerance: Therapeutic implications for autoimmune diseases ANA M. C. FARIA1 & HOWARD L. WEINER2 1Departamento de Bioquı´mica e Imunologia, Instituto de Cieˆncias Biolo´gicas, Universidade Federal de Minas Gerais, Av. Antonio Carlos, 6627, Belo Horizonte, MG 31270-901, Brazil, and 2Harvard Medical School, Center for Neurologic Diseases, Brigham and Women’s Hospital, 77 Avenue Louis Pasteur, Boston, MA 02115, USA Abstract Oral tolerance is classically defined as the suppression of immune responses to antigens (Ag) that have been administered previously by the oral route. Multiple mechanisms of tolerance are induced by oral Ag. Low doses favor active suppression, whereas higher doses favor clonal anergy/deletion. Oral Ag induces Th2 (IL-4/IL-10) and Th3 (TGF-b) regulatory T cells (Tregs) plus CD4þCD25þ regulatory cells and LAPþT cells. Induction of oral tolerance is enhanced by IL-4, IL-10, anti-IL-12, TGF-b, cholera toxin B subunit (CTB), Flt-3 ligand, anti-CD40 ligand and continuous feeding of Ag. In addition to oral tolerance, nasal tolerance has also been shown to be effective in suppressing inflammatory conditions with the advantage of a lower dose requirement. Oral and nasal tolerance suppress several animal models of autoimmune diseases including experimental allergic encephalomyelitis (EAE), uveitis, thyroiditis, myasthenia, arthritis and diabetes in the nonobese diabetic (NOD) mouse, plus non-autoimmune diseases such as asthma, atherosclerosis, colitis and stroke. Oral tolerance has been tested in human autoimmune diseases including MS, arthritis, uveitis and diabetes and in allergy, contact sensitivity to DNCB, nickel allergy. -

The Distribution of Immune Cells in the Uveal Tract of the Normal Eye
THE DISTRIBUTION OF IMMUNE CELLS IN THE UVEAL TRACT OF THE NORMAL EYE PAUL G. McMENAMIN Perth, Western Australia SUMMARY function of these cells in the normal iris, ciliary body Inflammatory and immune-mediated diseases of the and choroid. The role of such cell types in ocular eye are not purely the consequence of infiltrating inflammation, which will be discussed by other inflammatory cells but may be initiated or propagated authors in this issue, is not the major focus of this by immune cells which are resident or trafficking review; however, a few issues will be briefly through the normal eye. The uveal tract in particular considered where appropriate. is the major site of many such cells, including resident tissue macro phages, dendritic cells and mast cells. This MACRO PHAGES review considers the distribution and location of these and other cells in the iris, ciliary body and choroid in Mononuclear phagocytes arise from bone marrow the normal eye. The uveal tract contains rich networks precursors and after a brief journey in the blood as of both resident macrophages and MHe class 11+ monocytes immigrate into tissues to become macro dendritic cells. The latter appear strategically located to phages. In their mature form they are widely act as sentinels for capturing and sampling blood-borne distributed throughout the body. Macrophages are and intraocular antigens. Large numbers of mast cells professional phagocytes and play a pivotal role as are present in the choroid of most species but are effector cells in cell-mediated immunity and inflam virtually absent from the anterior uvea in many mation.1 In addition, due to their active secretion of a laboratory animals; however, the human iris does range of important biologically active molecules such contain mast cells. -
Of T Cell Tolerance
cells Review Strength and Numbers: The Role of Affinity and Avidity in the ‘Quality’ of T Cell Tolerance Sébastien This 1,2,† , Stefanie F. Valbon 1,2,†, Marie-Ève Lebel 1 and Heather J. Melichar 1,3,* 1 Centre de Recherche de l’Hôpital Maisonneuve-Rosemont, Montréal, QC H1T 2M4, Canada; [email protected] (S.T.); [email protected] (S.F.V.); [email protected] (M.-È.L.) 2 Département de Microbiologie, Immunologie et Infectiologie, Université de Montréal, Montréal, QC H3C 3J7, Canada 3 Département de Médecine, Université de Montréal, Montréal, QC H3T 1J4, Canada * Correspondence: [email protected] † These authors contributed equally to this work. Abstract: The ability of T cells to identify foreign antigens and mount an efficient immune response while limiting activation upon recognition of self and self-associated peptides is critical. Multiple tolerance mechanisms work in concert to prevent the generation and activation of self-reactive T cells. T cell tolerance is tightly regulated, as defects in these processes can lead to devastating disease; a wide variety of autoimmune diseases and, more recently, adverse immune-related events associated with checkpoint blockade immunotherapy have been linked to a breakdown in T cell tolerance. The quantity and quality of antigen receptor signaling depend on a variety of parameters that include T cell receptor affinity and avidity for peptide. Autoreactive T cell fate choices (e.g., deletion, anergy, regulatory T cell development) are highly dependent on the strength of T cell receptor interactions with self-peptide. However, less is known about how differences in the strength Citation: This, S.; Valbon, S.F.; Lebel, of T cell receptor signaling during differentiation influences the ‘function’ and persistence of anergic M.-È.; Melichar, H.J. -

The Combination of IL-12 and IL-18 NK/T-NK Cells Derived with IL-2, IL-15
Cytokine Production and Killer Activity of NK/T-NK Cells Derived with IL-2, IL-15, or the Combination of IL-12 and IL-18 This information is current as Bernard R. Lauwerys, Nathalie Garot, Jean-Christophe of September 28, 2021. Renauld and Frédéric A. Houssiau J Immunol 2000; 165:1847-1853; ; doi: 10.4049/jimmunol.165.4.1847 http://www.jimmunol.org/content/165/4/1847 Downloaded from References This article cites 31 articles, 17 of which you can access for free at: http://www.jimmunol.org/content/165/4/1847.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 28, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2000 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. Cytokine Production and Killer Activity of NK/T-NK Cells Derived with IL-2, IL-15, or the Combination of IL-12 and IL-181 Bernard R. Lauwerys,* Nathalie Garot,* Jean-Christophe Renauld,†‡ and Fre´de´ric A. -

Interleukin-18 in Health and Disease
International Journal of Molecular Sciences Review Interleukin-18 in Health and Disease Koubun Yasuda 1 , Kenji Nakanishi 1,* and Hiroko Tsutsui 2 1 Department of Immunology, Hyogo College of Medicine, 1-1 Mukogawa-cho, Nishinomiya, Hyogo 663-8501, Japan; [email protected] 2 Department of Surgery, Hyogo College of Medicine, 1-1 Mukogawa-cho, Nishinomiya, Hyogo 663-8501, Japan; [email protected] * Correspondence: [email protected]; Tel.: +81-798-45-6573 Received: 21 December 2018; Accepted: 29 January 2019; Published: 2 February 2019 Abstract: Interleukin (IL)-18 was originally discovered as a factor that enhanced IFN-γ production from anti-CD3-stimulated Th1 cells, especially in the presence of IL-12. Upon stimulation with Ag plus IL-12, naïve T cells develop into IL-18 receptor (IL-18R) expressing Th1 cells, which increase IFN-γ production in response to IL-18 stimulation. Therefore, IL-12 is a commitment factor that induces the development of Th1 cells. In contrast, IL-18 is a proinflammatory cytokine that facilitates type 1 responses. However, IL-18 without IL-12 but with IL-2, stimulates NK cells, CD4+ NKT cells, and established Th1 cells, to produce IL-3, IL-9, and IL-13. Furthermore, together with IL-3, IL-18 stimulates mast cells and basophils to produce IL-4, IL-13, and chemical mediators such as histamine. Therefore, IL-18 is a cytokine that stimulates various cell types and has pleiotropic functions. IL-18 is a member of the IL-1 family of cytokines. IL-18 demonstrates a unique function by binding to a specific receptor expressed on various types of cells. -

Engineering Strategies to Enhance TCR-Based Adoptive T Cell Therapy
cells Review Engineering Strategies to Enhance TCR-Based Adoptive T Cell Therapy Jan A. Rath and Caroline Arber * Department of oncology UNIL CHUV, Ludwig Institute for Cancer Research Lausanne, Lausanne University Hospital and University of Lausanne, 1015 Lausanne, Switzerland * Correspondence: [email protected] Received: 18 May 2020; Accepted: 16 June 2020; Published: 18 June 2020 Abstract: T cell receptor (TCR)-based adoptive T cell therapies (ACT) hold great promise for the treatment of cancer, as TCRs can cover a broad range of target antigens. Here we summarize basic, translational and clinical results that provide insight into the challenges and opportunities of TCR-based ACT. We review the characteristics of target antigens and conventional αβ-TCRs, and provide a summary of published clinical trials with TCR-transgenic T cell therapies. We discuss how synthetic biology and innovative engineering strategies are poised to provide solutions for overcoming current limitations, that include functional avidity, MHC restriction, and most importantly, the tumor microenvironment. We also highlight the impact of precision genome editing on the next iteration of TCR-transgenic T cell therapies, and the discovery of novel immune engineering targets. We are convinced that some of these innovations will enable the field to move TCR gene therapy to the next level. Keywords: adoptive T cell therapy; transgenic TCR; engineered T cells; avidity; chimeric receptors; chimeric antigen receptor; cancer immunotherapy; CRISPR; gene editing; tumor microenvironment 1. Introduction Adoptive T cell therapy (ACT) with T cells expressing native or transgenic αβ-T cell receptors (TCRs) is a promising treatment for cancer, as TCRs cover a wide range of potential target antigens [1]. -

IL-7) and IL-7 Splice Variants Affect Differentiation of Human Neural Progenitor Cells
Genes and Immunity (2010) 11, 11–20 & 2010 Macmillan Publishers Limited All rights reserved 1466-4879/10 $32.00 www.nature.com/gene ORIGINAL ARTICLE Interleukin-7 (IL-7) and IL-7 splice variants affect differentiation of human neural progenitor cells M Moors1,4, NK Vudattu2,, J Abel1, U Kra¨mer1, L Rane2, N Ulfig3, S Ceccatelli4, V Seyfert-Margolies5, E Fritsche1 and MJ Maeurer2 1Group of Toxicology, Group of Epidemiology, Institut fu¨r Umweltmedizinische Forschung, Du¨sseldorf, Germany; 2Microbiology, Tumor and Cell Biology and Smittskyddsinstitutet, Stockholm, Sweden; 3Department of Anatomy, University of Rostock, Rostock, Germany; 4Division of Neurotoxicology, Department of Neuroscience, Karolinska Institutet, Sweden and 5Department of Medicine, University of California, San Francisco, CA, USA Alternative splicing of pre-mRNA increases proteomic diversity, a crucial mechanism in defining tissue identity. We demonstrate differentially spliced interleukin (IL)-7 in distinct anatomic areas in the adult, in developing human brains and in normal human neuronal progenitor (NHNP) cells. IL-7c (c, the canonical form spanning all six exons) or its variants IL-7d5, d4 or d4/5 were cloned and expressed as recombinant proteins. IL-7 and splice variants were able to shift the differentiation of NHNP cells as compared with the diluent control (Po0.01) defined by anti-b (III)-tubulin and glial fibrillary acidic protein expression, with different degrees (IL-7c4d4/54IL-7d5); IL-7d4 exhibited a significantly weaker potency. Differentiation was confirmed by transcriptome analysis of IL-7c-stimulated neural NHNP cells, resulting in 58 differentially expressed genes; some of these are involved in neural differentiation, for example, the developmentally regulated transcription factor kru¨ppel-like factor 12, musashi 2, a translational regulator of cell fate or the sonic hedgehog receptor patch 1. -
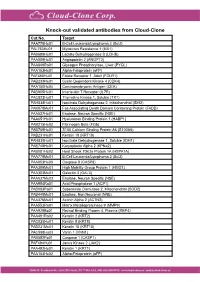
Knock-Out Validated Antibodies from Cloud-Clone Cat.No
Knock-out validated antibodies from Cloud-Clone Cat.No. Target PAA778Hu01 B-Cell Leukemia/Lymphoma 2 (Bcl2) PAL763Hu01 Myxovirus Resistance 1 (MX1) PAB698Hu01 Lactate Dehydrogenase B (LDHB) PAA009Hu01 Angiopoietin 2 (ANGPT2) PAA849Ra01 Glycogen Phosphorylase, Liver (PYGL) PAA153Hu01 Alpha-Fetoprotein (aFP) PAF460Hu01 Folate Receptor 1, Adult (FOLR1) PAB233Hu01 Cyclin Dependent Kinase 4 (CDK4) PAA150Hu04 Carcinoembryonic Antigen (CEA) PAB905Hu01 Interleukin 7 Receptor (IL7R) PAC823Hu01 Thymidine Kinase 1, Soluble (TK1) PAH838Hu01 Isocitrate Dehydrogenase 2, mitochondrial (IDH2) PAK078Mu01 Fas Associating Death Domain Containing Protein (FADD) PAA537Hu01 Enolase, Neuron Specific (NSE) PAA651Hu01 Hyaluronan Binding Protein 1 (HABP1) PAB215Hu02 Fibrinogen Beta (FGb) PAB769Hu01 S100 Calcium Binding Protein A6 (S100A6) PAB231Hu01 Keratin 18 (KRT18) PAH839Hu01 Isocitrate Dehydrogenase 1, Soluble (IDH1) PAE748Hu01 Karyopherin Alpha 2 (KPNa2) PAB081Hu02 Heat Shock 70kDa Protein 1A (HSPA1A) PAA778Mu01 B-Cell Leukemia/Lymphoma 2 (Bcl2) PAA853Hu03 Caspase 8 (CASP8) PAA399Mu01 High Mobility Group Protein 1 (HMG1) PAA303Mu01 Galectin 3 (GAL3) PAA537Mu02 Enolase, Neuron Specific (NSE) PAA994Ra01 Acid Phosphatase 1 (ACP1) PAB083Ra01 Superoxide Dismutase 2, Mitochondrial (SOD2) PAB449Mu01 Enolase, Non Neuronal (NNE) PAA376Mu01 Actinin Alpha 2 (ACTN2) PAA553Ra01 Matrix Metalloproteinase 9 (MMP9) PAA929Bo01 Retinol Binding Protein 4, Plasma (RBP4) PAA491Ra02 Keratin 2 (KRT2) PAC025Hu01 Keratin 8 (KRT8) PAB231Mu01 Keratin 18 (KRT18) PAC598Hu03 Vanin 1 (VNN1) -

Commentary Clonal Anergy of B Cells
Commentary Clonal Anergy of B Cells: A Flexible, Reversible, and Quantitative Concept By G.J.V. Nossal From The Walter and Eliza Hall Institute of Medical Research, Post Office, The Royal Melbourne Hospital, Victoria 3050, Australia t the conclusion of the 1986 Immunology Congress in termed clonal anergy (7). Support for clonal anergy among A Toronto, the late Georges K6hler presented a sum- T lymphocytes also gradually emerged (8, 9). mary lecture which was, unfortunately, poorly attended. It Enter transgenic mouse technology. As far as B cell tol- dealt with the impact of the new genetics on immunology, erance was concerned, the first results were disappointing. Downloaded from http://rupress.org/jem/article-pdf/183/5/1953/1108328/1953.pdf by guest on 29 September 2021 and, among other wise things, he said that transgenic tech- Antigen-transgenic mice were either non-tolerant or vari- nology was set to revolutionize the way we studied immu- ably tolerant (10, 11). However, antigen-transgenic animals nologic tolerance (1). The greatest barrier to uncovering were not the main game, as they left the investigator with the details of what happened to anti-self cells in the repertoire the task of studying the minority of (unidentifiable) reactive was the heterogeneity oflymphocytes. Cells potentially re- lymphocytes. Things really took off when B (12, 13) or T active with a given self antigen were so rare that most at- (14) cell receptor transgenic mice were used. From the tempts to study their fate retied on inferential rather than viewpoint of the present story (15), the critical model was direct methods. -

BAFF Suppresses IL-15 Expression in B Cells
BAFF Suppresses IL-15 Expression in B Cells Ning Ma, Chen Xing, He Xiao, Youdi He, Gencheng Han, Guojiang Chen, Chunmei Hou, Bernadette Marrero, Yujuan Wang, Shengquan Zhang, Beifen Shen, Yan Li and Renxi This information is current as Wang of September 28, 2021. J Immunol 2014; 192:4192-4201; Prepublished online 26 March 2014; doi: 10.4049/jimmunol.1302132 http://www.jimmunol.org/content/192/9/4192 Downloaded from Supplementary http://www.jimmunol.org/content/suppl/2014/03/26/jimmunol.130213 Material 2.DCSupplemental http://www.jimmunol.org/ References This article cites 39 articles, 14 of which you can access for free at: http://www.jimmunol.org/content/192/9/4192.full#ref-list-1 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision by guest on September 28, 2021 • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology BAFF Suppresses IL-15 Expression in B Cells Ning Ma,*,†,1 Chen Xing,*,1 He Xiao,*,1 Youdi He,‡ Gencheng Han,* Guojiang Chen,* Chunmei Hou,* Bernadette Marrero,x Yujuan Wang,{ Shengquan Zhang,‖ Beifen Shen,* Yan Li,* and Renxi Wang* Clinical trials have shown that BAFF inhibitors do not reduce memory B cell levels but can reduce the number of mature B cells. -

Phase I Study of Recombinant Human Interleukin-7 Administration in Subjects with Refractory Malignancy
Published OnlineFirst January 12, 2010; DOI: 10.1158/1078-0432.CCR-09-1303 Cancer Therapy: Clinical Clinical Cancer Research Phase I Study of Recombinant Human Interleukin-7 Administration in Subjects with Refractory Malignancy Claude Sportès1, Rebecca R. Babb1, Michael C. Krumlauf1, Frances T. Hakim1, Seth M. Steinberg2, Catherine K. Chow5, Margaret R. Brown6, Thomas A. Fleisher6, Pierre Noel6, Irina Maric6, Maryalice Stetler-Stevenson3, Julie Engel7, Renaud Buffet7, Michel Morre7, Robert J. Amato8, Andrew Pecora9, Crystal L. Mackall4, and Ronald E. Gress1 Abstract Purpose: Interleukin-7 (IL-7) has critical and nonredundant roles in T-cell development, hematopoi- esis, and postdevelopmental immune functions as a prototypic homeostatic cytokine. Based on a large body of preclinical evidence, it may have multiple therapeutic applications in immunodeficiency states, either physiologic (immunosenescence), pathologic (HIV), or iatrogenic (postchemotherapy and posthe- matopoietic stem cell transplant), and may have roles in immune reconstitution or enhancement of im- munotherapy. We report here on the toxicity and biological activity of recombinant human IL-7 (rhIL-7) in humans. Design: Subjects with incurable malignancy received rhIL-7 subcutaneously every other day for 2 weeks in a phase I interpatient dose escalation study (3, 10, 30, and 60 μg/kg/dose). The objectives were safety and dose-limiting toxicity determination, identification of a range of biologically active doses, and char- acterization of biological and, possibly, antitumor effects. Results: Mild to moderate constitutional symptoms, reversible spleen and lymph node enlargement, and marked increase in peripheral CD3+, CD4+, and CD8+ lymphocytes were seen in a dose-dependent and age-independent manner in all subjects receiving ≥10 μg/kg/dose, resulting in a rejuvenated circulat- ing T-cell profile, resembling that seen earlier in life.