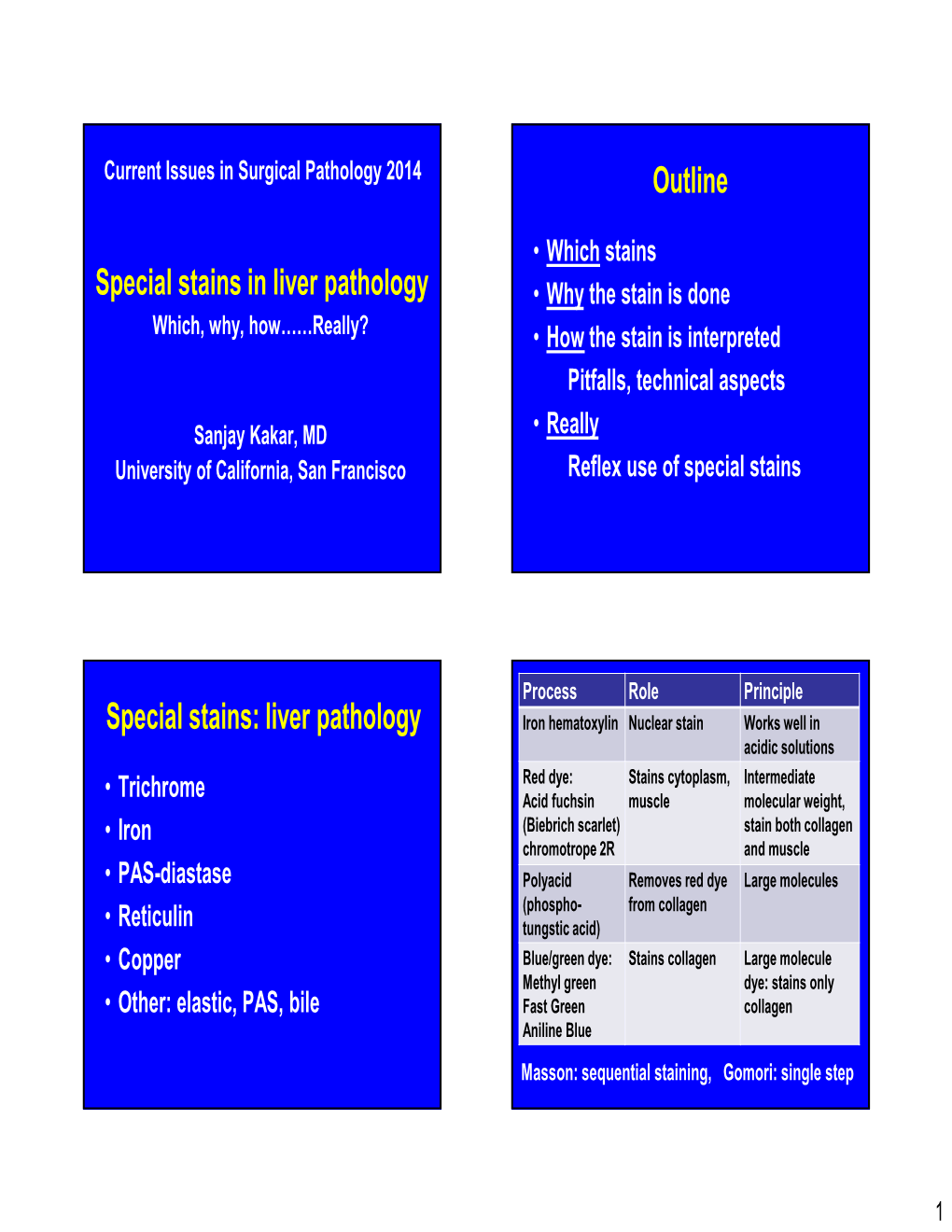
Liver Pathology • Why the Stain Is Done Which, Why, How……Really? • How the Stain Is Interpreted Pitfalls, Technical Aspects
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Medical Directors Arup Medical Directors and Consulting Faculty | 2015
MEDICAL DIRECTORS ARUP MEDICAL DIRECTORS AND CONSULTING FACULTY | 2015 MAY 2015 www.aruplab.com Information in this brochure is current as of May 2015. All content is subject to change. Please contact ARUP Client Services at (800) 522-2787 with any questions or concerns. ARUP LABORATORIES ARUP Laboratories is a national clinical and anatomic pathology reference laboratory and a nonprofit enterprise of the University of Utah and its Department of Pathology. Located in Salt Lake City, Utah, ARUP offers in excess of 3,000 tests and test combinations, ranging from routine screening tests to esoteric molecular and genetic assays. Rather than competing with its clients for physician office business, ARUP chooses instead to support clients’ existing test menus by offering complex and unique tests, with accompanying consultative support, to enhance their abilities to provide local and regional laboratory services. ARUP’s clients include many of the nation’s university teaching hospitals and children’s hospitals, as well as multihospital groups, major commercial laboratories, group purchasing organizations, military and other government facilities, and major clinics. In addition, ARUP is a worldwide leader in innovative laboratory research and development, led by the efforts of the ARUP Institute for Clinical and Experimental Pathology®. Since its formation in 1984 by the Department of Pathology at the University of Utah, ARUP has founded its reputation on reliable and consistent laboratory testing and service. This simple strategy contributes significantly to client satisfaction. When ARUP conducts surveys, clients regularly rate ARUP highly and respond that they would recommend ARUP to others. As the most responsive source of quality information and knowledge, ARUP strives to be the reference laboratory of choice for community healthcare systems. -

Impact of HIV on Gastroenterology/Hepatology
Core Curriculum: Impact of HIV on Gastroenterology/Hepatology AshutoshAshutosh Barve,Barve, M.D.,M.D., Ph.D.Ph.D. Gastroenterology/HepatologyGastroenterology/Hepatology FellowFellow UniversityUniversityUniversity ofofof LouisvilleLouisville Louisville Case 4848 yearyear oldold manman presentspresents withwith aa historyhistory ofof :: dysphagiadysphagia odynophagiaodynophagia weightweight lossloss EGDEGD waswas donedone toto evaluateevaluate thethe problemproblem University of Louisville Case – EGD Report ExtensivelyExtensively scarredscarred esophagealesophageal mucosamucosa withwith mucosalmucosal bridging.bridging. DistalDistal esophagealesophageal nodulesnodules withwithUniversity superficialsuperficial ulcerationulceration of Louisville Case – Esophageal Nodule Biopsy InflammatoryInflammatory lesionlesion withwith ulceratedulcerated mucosamucosa SpecialSpecial stainsstains forfor fungifungi revealreveal nonnon-- septateseptate branchingbranching hyphaehyphae consistentconsistent withwith MUCORMUCOR University of Louisville Case TheThe patientpatient waswas HIVHIV positivepositive !!!! University of Louisville HAART (Highly Active Anti Retroviral Therapy) HIV/AIDS Before HAART After HAART University of Louisville HIV/AIDS BeforeBefore HAARTHAART AfterAfter HAARTHAART ImmuneImmune dysfunctiondysfunction ImmuneImmune reconstitutionreconstitution OpportunisticOpportunistic InfectionsInfections ManagementManagement ofof chronicchronic ¾ Prevention diseasesdiseases e.g.e.g. HepatitisHepatitis CC ¾ Management CirrhosisCirrhosis NeoplasmsNeoplasms -

Steatosis in Hepatitis C: What Does It Mean? Tarik Asselah, MD, Nathalie Boyer, MD, and Patrick Marcellin, MD*
Steatosis in Hepatitis C: What Does It Mean? Tarik Asselah, MD, Nathalie Boyer, MD, and Patrick Marcellin, MD* Address Steatosis *Service d’Hépatologie, Hôpital Beaujon, Mechanisms of steatosis 100 Boulevard du Général Leclerc, Clichy 92110, France. Hepatic steatosis develops in the setting of multiple E-mail: [email protected] clinical conditions, including obesity, diabetes mellitus, Current Hepatitis Reports 2003, 2:137–144 alcohol abuse, protein malnutrition, total parenteral Current Science Inc. ISSN 1540-3416 Copyright © 2003 by Current Science Inc. nutrition, acute starvation, drug therapy (eg, corticosteroid, amiodarone, perhexiline, estrogens, methotrexate), and carbohydrate overload [1–4,5••]. Hepatitis C and nonalcoholic fatty liver disease (NAFLD) are In the fed state, dietary triglycerides are processed by the both common causes of liver disease. Thus, it is not surprising enterocyte into chylomicrons, which are secreted into the that they can coexist in the same individual. The prevalence of lymph. The chylomicrons are hydrolyzed into fatty acids by steatosis in patients with chronic hepatitis C differs between lipoprotein lipase. These free fatty acids are transported to the studies, probably reflecting population differences in known liver, stored in adipose tissue, or used as energy sources by risk factors for steatosis, namely overweight, diabetes, and muscles. Free fatty acids are also supplied to the liver in the dyslipidemia. The pathogenic significance of steatosis likely form of chylomicron remnants, which are then hydrolyzed by differs according to its origin, metabolic (NAFLD or non- hepatic triglyceride lipase. During fasting, the fatty acids sup- alcoholic steatohepatitis) or virus related (due to hepatitis C plied to the liver are derived from hydrolysis (mediated by a virus genotype 3). -

Corneal Endotheliitis with Cytomegalovirus Infection of Persisted
Correspondence 1105 Sir, resulted in gradual decreases of KPs, but graft oedema Corneal endotheliitis with cytomegalovirus infection of persisted. Vision decreased to 20/2000. corneal stroma The patient underwent a second keratoplasty combined with cataract surgery in August 2007. Although involvement of cytomegalovirus (CMV) in The aqueous humour was tested for polymerase corneal endotheliitis was recently reported, the chain reaction to detect HSV, VZV, or CMV; a positive pathogenesis of this disease remains uncertain.1–8 Here, result being obtained only for CMV-DNA. Pathological we report a case of corneal endotheliitis with CMV examination demonstrated granular deposits in the infection in the corneal stroma. deep stroma, which was positive for CMV by immunohistochemistry (Figures 2a and b). The cells showed a typical ‘owl’s eye’ morphology (Figure 2c). Case We commenced systemic gancyclovir at 10 mg per day A 44-year-old man was referred for a gradual decrease in for 7 days, followed by topical 0.5% gancyclovir eye vision with a history of recurrent iritis with unknown drops six times a day. With the postoperative follow-up aetiology. The corrected visual acuity in his right eye was period of 20 months, the graft remained clear without 20/200. Slit lamp biomicroscopy revealed diffuse corneal KPs (Figure 1d). The patient has been treated with oedema with pigmented keratic precipitates (KPs) gancyclovir eye drops t.i.d. to date. His visual acuity without anterior chamber cellular reaction (Figure 1a). improved to 20/20, and endothelial density was The patient had undergone penetrating keratoplasty in 2300/mm2. Repeated PCR in aqueous humour for August 2006, and pathological examination showed non- CMV yielded a negative result in the 10th week. -

In Colorectal Cancer
Article Evaluation of Adjuvant Chemotherapy-Associated Steatosis (CAS) in Colorectal Cancer Michelle C. M. Lee 1,2 , Jacob J. Kachura 3, Paraskevi A. Vlachou 1,2, Raissa Dzulynsky 1, Amy Di Tomaso 3, Haider Samawi 1,2, Nancy Baxter 1,2 and Christine Brezden-Masley 1,3,4,* 1 St. Michael’s Hospital, 30 Bond St, Toronto, ON M5B 1W8, Canada; [email protected] (M.C.M.L.); [email protected] (P.A.V.); [email protected] (R.D.); [email protected] (H.S.); [email protected] (N.B.) 2 Medical Sciences Building, 1 King’s College Circle, University of Toronto, Toronto, ON M5S 1A8, Canada 3 Mount Sinai Hospital, 1284-600 University Avenue, Toronto, ON M5G 1X5, Canada; [email protected] (J.J.K.); [email protected] (A.D.T.) 4 Lunenfeld-Tanenbaum Research Institute, 600 University Ave, Toronto, ON M5G 1X5, Canada * Correspondence: [email protected]; Tel.: +416-586-8605; Fax: +416-586-8659 Abstract: Chemotherapy-associated steatosis is poorly understood in the context of colorectal can- cer. In this study, Stage II–III colorectal cancer patients were retrospectively selected to evaluate the frequency of chemotherapy-associated steatosis and to determine whether patients on statins throughout adjuvant chemotherapy develop chemotherapy-associated steatosis at a lower frequency. Baseline and incident steatosis for up to one year from chemotherapy start date was assessed based on radiology. Of 269 patients, 76 (28.3%) had steatosis at baseline. Of the remaining 193 cases, patients receiving adjuvant chemotherapy (n = 135) had 1.57 (95% confidence interval [CI], 0.89 to 2.79) times the adjusted risk of developing steatosis compared to patients not receiving chemotherapy (n = 58). -

Life Science Journal, 2011;8(4)
Life Science Journal, 2011;8(4) http://www.lifesciencesite.com Histopathological and Immunohistochemical Studies on the Adrenal Medullary Tumors in Egyptian Patients Samia, M. Sanad1, Mahmoud, A. El-Baz2, Omar, I. Ghonemy3 and Hassan, F. Abo El-Nazar4 1Zoology Department, Faculty of Science, Zagazig University, Egypt 2Pathology Department, Faculty of Medicine, Mansoura University, Egypt 3Zoology Department, Faculty of Science, Benha University, Egypt 4Urology and Nephrology Center, Mansoura University, Egypt [email protected] Abstract: The present study provides guide lines for the diagnosis of adrenal medullary tumors in Egyptian patients. This retrospective study included, 73 cases of adrenal medullary tumors (39 pheochromocytoma, 13 neuroblastoma, 12 ganglioneuroblastoma and 9 ganglioneuroma) admitted to Mansoura Urology and Nephrology Center, Egypt.. All tumors were studied histologically and immunohistochemically. In pheochromocytomas, 33 patients became normal after 24 hours, the other 6 died from distant metastases. 6 patients with neuroblastoma and ganglioneuroblastoma were still living after adrenalectomy, while the other 19 patients received chemotherapy and were non-living after 24 months. Nine patients with ganglioneuroma were still living after adrenalectomy. All prepared slides were stained with periodic-acid Schiff’ reaction (PAS) and reticulin stains. Hyaline globules which were (PAS) positive were pheochromocytomas, while, they were not detected in neuroblastoma groups. All tumors were positive for reticulin stain. All cases of adrenal medulalry tumors were examined immunohistochemically using antibodies against chromogranin A, S-100 protein and neuron-specific enolase . Chromogranin A was expressed in all cases (39/39) pheochromocytoma, 5/13 neuroblastoma, 7/12 ganglioneuroblastoma and 7/9 ganglioneuroma. S-100 protein was expressed in 32/39 pheochromocytoma, 9/13 neuroblastomas, and all cases of ganglioneuroblastoma and ganglioneuroma. -

Understanding Your Pathology Report: Benign Breast Conditions
cancer.org | 1.800.227.2345 Understanding Your Pathology Report: Benign Breast Conditions When your breast was biopsied, the samples taken were studied under the microscope by a specialized doctor with many years of training called a pathologist. The pathologist sends your doctor a report that gives a diagnosis for each sample taken. Information in this report will be used to help manage your care. The questions and answers that follow are meant to help you understand medical language you might find in the pathology report from a breast biopsy1, such as a needle biopsy or an excision biopsy. In a needle biopsy, a hollow needle is used to remove a sample of an abnormal area. An excision biopsy removes the entire abnormal area, often with some of the surrounding normal tissue. An excision biopsy is much like a type of breast-conserving surgery2 called a lumpectomy. What does it mean if my report uses any of the following terms: adenosis, sclerosing adenosis, apocrine metaplasia, cysts, columnar cell change, columnar cell hyperplasia, collagenous spherulosis, duct ectasia, columnar alteration with prominent apical snouts and secretions (CAPSS), papillomatosis, or fibrocystic changes? All of these are terms that describe benign (non-cancerous) changes that the pathologist might see under the microscope. They do not need to be treated. They are of no concern when found along with cancer. More information about many of these can be found in Non-Cancerous Breast Conditions3. What does it mean if my report says fat necrosis? Fat necrosis is a benign condition that is not linked to cancer risk. -

Symmetrical Peripheral Gangrene Associated with Low Output Cardiac Failure
Tower Health Scholar Commons @ Tower Health Reading Hospital Internal Medicine Residency Internal Medicine Residency 7-17-2019 Symmetrical Peripheral Gangrene Associated with Low Output Cardiac Failure. Sijan Basnet Reading Hospital-Tower Health Priya Rajagopalan Thomas Jefferson University Hospital Rashmi Dhital Reading Hospital-Tower Health Ataul Qureshi Thomas Jefferson University Hospital Follow this and additional works at: http://scholarcommons.towerhealth.org/ gme_int_med_resident_program_read Part of the Cardiology Commons Recommended Citation Basnet, S., Rajagopalan, P., Dhital, R., & Qureshi, A. (2019). Symmetrical Peripheral Gangrene Associated with Low Output Cardiac Failure.. Medicina (Kaunas, Lithuania), 55 (7) https://doi.org/10.3390/ medicina55070383. This Article is brought to you for free and open access by the Internal Medicine Residency at Scholar Commons @ Tower Health. It has been accepted for inclusion in Reading Hospital Internal Medicine Residency by an authorized administrator of Scholar Commons @ Tower Health. For more information, please contact [email protected]. medicina Case Report Symmetrical Peripheral Gangrene Associated with y Low Output Cardiac Failure Sijan Basnet 1,* , Priya Rajagopalan 2, Rashmi Dhital 1 and Ataul Qureshi 2 1 Department of Medicine, Reading Hospital and Medical Center, West Reading, PA 19611, USA 2 Thomas Jefferson University Hospital, 1025 Walnut Street, Philadelphia, PA 19107, USA * Correspondence: [email protected]; Tel.: +484-628-8255 The abstract was accepted for poster presentation at “Heart Failure Society of America 2018 Annual y Meeting” and was published in Journal of Cardiac Failure. Received: 15 January 2019; Accepted: 15 July 2019; Published: 17 July 2019 Abstract: Symmetrical peripheral gangrene (SPG) is a rare entity characterized by ischemic changes of the distal extremities with maintained vascular integrity. -

Simple Technique to Identify Haemosiderin in Immunoperoxidase Stained Sections
J Clin Pathol: first published as 10.1136/jcp.37.10.1190 on 1 October 1984. Downloaded from 1190 Technical methods Phosphate buffer at pH 8*0 gave the sharpest 2 Rozenszajn L, Leibovich M, Shoham D, Epstein J. The esterase staining reactions, although there was little differ- activity in megaloblasts, leukaemic and normal haemopoietic cells. Br J Haematol 1968; 14:605-19. ence at pH 7-0 or pH 7-5. As the buffer pH was 3Hayhoe FGJ, Quaglino D. Haematological cytochemistry. Edin- increased above pH 8-0 staining with both substrates burgh: Churchill Livingstone, 1980. became progressively weaker, especially above pH 4Li CY, Lam KW, Yam LT. Esterases in human leucocytes. J 9.0. Below pH 7-0 staining with a-naphthyl butyrate Histochem Cytochem 1973;21:1-12. Yam LT, Li CY, Crosby WH. Cytochemical identification of became weaker, and below pH 5*0 staining with monocytes and granulocytes. Am J Clin Pathol 1971;55:283- naphthol AS-D chloroacetate began to disappear. 90. 6 Armitage RJ, Linch DC, Worman CP, Cawley JC. The morphol- This work was supported by a Medical Research ogy and cytochemistry of human T-cell subpopulations defined by monoclonal antibodies and Fc receptors. Br J Haematol Council project grant. I thank Professor FGJ 1983;51:605-13. Hayhoe for valuable advice. References Requests for reprints to: Dr DM Swirsky, Department of Gomori G. Chloroacyl esters as histochemical substrates. J His- Haematological Medicine, University Clinical School, Hills tochem Cytochem 1953;1:469-70. Road, Cambridge CB2 2QL, England. Simple technique to identify identification of the two compounds on the same haemosiderin in slide. -

IHC) Outreach Services
Immunohistochemistry (IHC) Outreach Services Note t ype of fixative used if not neutral buffered f ormalin. Note t ype of tissue/specim en Unless specified otherwise, positive and negative controls react satisfactoril y. Antibody Classif ications: – IVD (In Vitro Diagnosis) – No disclaimer required. – ASR (Anal yte Specific Reagent) – m ust use a disclaimer on the report (See Belo w) ASR required disclaimer T his test was developed a nd its perform ance characteristics determ ined b y Marshf ield Labs. It has not been cleared or approved b y th e U.S. Food and Drug Adm inistration. T he FDA has determ ined that such clearance or approval is not necessar y. T his test is used f or clinical purposes. It should not be regarded as investigational or f or research. T his laborator y is certif ied under the Clinical Laborator y Im provem ent Am endm ents (CLIA) as qualified to perf orm high-complexity testing. Available Chrom ogen – All m ark ers have been validated with 3,3’-Diam inobenzidine T etrah ydrochloride (DAB) which results in a bro wn/black precipitate. DAB is the routine chrom ogen. In addition, som e m ark ers have also been validated using the Fast Red (RED), which results in a re d precipitate. If available wit h both chrom ogens and one is not selected, the def ault will be t he DAB chrom ogen. Antibod y Common Applications Staining Characteristics/Cla ssification If Other Than IVD Actin (muscle specific) Smooth, skeletal & cardiac muscle Cytoplasmic Actin (smooth muscle) Smooth muscle and myoepithelial cells Cytoplasmic and membrane Adrenocorticotropin (ACTH) Pituitary neoplasms Cytoplasmic Alpha-1-Fetoprotein (AFP) Hepatoma, germ cell tumors Cytoplasmic ALK Protein ALK1 positive lymphomas Cytoplasmic and/or nuclear Alpha-1-Antitrypsin Demonstrates A-1-AT in liver Cytoplasmic (A-1-AT) Bcl-2 Oncoprotein Follicular lymphoma and soft tissue Cytoplasmic tumors Bcl-6 Follicular lymphoma Nuclear Ber-EP4, Epithelial Antigen Adenocarcinoma vs. -

Immunohistochemistry Immunohistochemistry
!"#$%&'"()(*+$(,$-#)&.(-&/$ 0--1.("23'(4"#-23'5+$$ 65.&17$7#$)&$8(14"&57295#$:;<$=";$ >+(.<$85&.4#$ Immunohistochemistry Immunohistochemistry It’s all about chosing the adapted anbody(ies) Immunohistochemistry It’s all about chosing the adapted anbody(ies) for the selected task(s) AnAbodies • « Melanocyc » anbodies – S100 – MelanA – HMB45 – PNL2 – MiTF Specificity vs Sensivity – SOX10 – … • « Anomaly-specific » anbodies – BRAF V600E – NRAS Q61R – ALK – ROS1 – NTRK1 – MET – P16 – BAP1 – PDL1 – … • Other anbodies – D2-40 – CD68 HMB45 – … AnAbodies • « Melanocyc » anbodies – S100 – MelanA – HMB45 – PNL2 – MiTF – SOX10 – … • « Anomaly-specific » anbodies – BRAF V600E – NRAS Q61R – ALK – ROS1 – NTRK1 – MET – P16 – BAP1 – PDL1 – … • Other anbodies – D2-40 – CD68 NTRK1 – … AnAbodies • « Melanocyc » anbodies – S100 – MelanA – HMB45 – PNL2 – MiTF – SOX10 – … • « Anomaly-specific » anbodies – BRAF V600E – NRAS Q61R – ALK – ROS1 – NTRK1 – MET – P16 – BAP1 – PDL1 – … • Other anbodies (DD mainly) – D2-40 – CD68 – … Why perform IHC? • Confirm melanocyc lineage • Visualize the melanocytes • Benign vs Malignant • Molecular characterizaon A. Confirm melanocyc lineage • Unpigmented dermal or ulcerated tumor (No recognizable junconal melanocytes) • Unpigmented metastases • Desmoplasc melanoma A1. Confirm melanocyc lineage Unpigmented dermal or ulcerated tumor M, 65 Back 6Ha$[(.T5-$-#)&.(4+A4$)2.#&*#$ b.%2*-#.'#7$7#5-&)$(5$1)4#5&'#7$'1-(5$$ b.%2*-#.'#7$.#3'$(,$#%2'"#)2(27$4#))3$ A1. Confirm melanocyc lineage Unpigmented dermal or ulcerated tumor S100 Protein 6Ha$[(.T5-$-#)&.(4+A4$)2.#&*#$ -

RHCL 2019 Price List
University of Texas MD Anderson Cancer Center Research Histology Core Laboratory Service Price List Service Provided Service Fee BONE SECTION Bone Section $6.50 per slide Additional bone section same slide $0.75 each section FROZEN SECTIONING Frozen Block Mount $4.50 each Frozen section $5.75 per slide Additional frozen sections on same slide + $0.75 per section* Additional frozen sections on same slide from additional blocks/map instructions + $1.00 per section* Cryomold $1.00 each OCT-Mold $3.00 each H&E STAINING H&E (-) Non Plus Slide $4.50 per slide H&E (+) Plus Slide $5.25 per slide H&E Stain Only $3.75 per slide H&E Stain Only (Plastic) on (+) slide $7.75 per slide H&E Stain (Manual) $8.00 per slide H&E Stain (Micron Interval) $6.25 each H&E Stain (Microdissection) $5.50 per slide Hematoxylin or Eosin Only $3.75per slide Additional H&E section on same slide +$0.50 per section * Additional H&E sections on same slide from additional blocks/map instructions +$1.00 per section* Deparaffinization $2.00 each IHC STAINING Immuno Manual Stain $35.00 per slide Immuno Stain $31.25 per slide Immuno Stain (Investigator AB) $25.00 per slide Immuno Stain (Plastic) $38.25 per slide Immuno Stain (Plastic Investigator AB) $35.25 per slide Immuno Stain (Manual) $28.00 per slide Immuno Stain – IHC $28.00 per slide Immuno Control Tissue $5.50 per slide Additional Titers $65.00 each Assay Development $468.75 each Fluorescent Counter Stain $15.00 per slide IMAGE ANALYSIS Scan Scope 20X (1-50) $8.00 per slide Scan Scope 20X (51-150) $7.00 per slide Scan