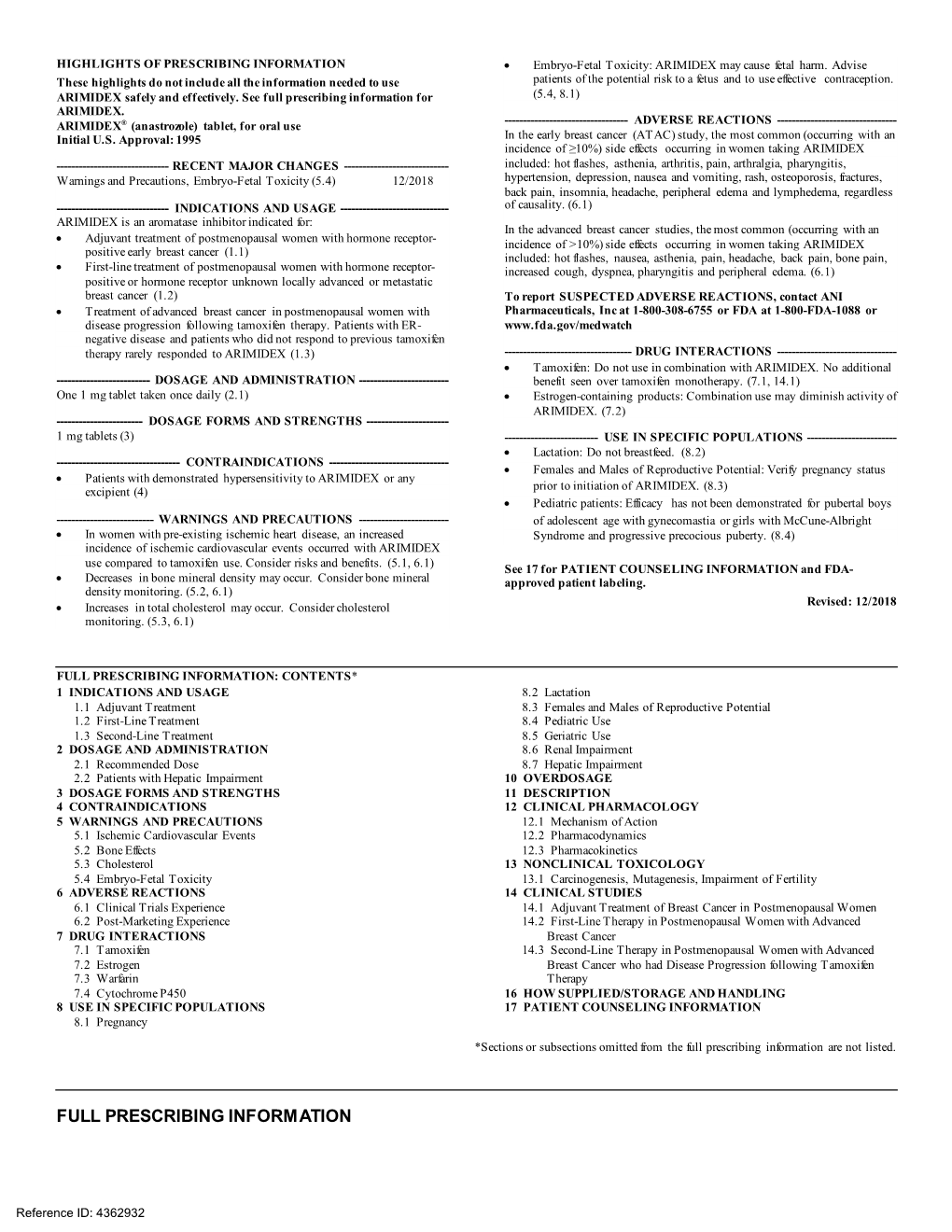
ARIMIDEX® (Anastrozole)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pharmacogenomics of Endocrine Therapy in Breast Cancer
Journal of Human Genetics (2013) 58, 306–312 & 2013 The Japan Society of Human Genetics All rights reserved 1434-5161/13 OPEN www.nature.com/jhg REVIEW Pharmacogenomics of endocrine therapy in breast cancer James N Ingle The most important modality of treatment in the two-thirds of patients with an estrogen receptor (ER)-positive early breast cancer is endocrine therapy. In postmenopausal women, options include the selective ER modulators (SERMs), tamoxifen and raloxifene, and the ‘third-generation’ aromatase inhibitors (AIs), anastrozole, exemestane and letrozole. Under the auspices of the National Institutes of Health Global Alliance for Pharmacogenomics, Japan, the Mayo Clinic Pharmacogenomics Research Network Center and the RIKEN Center for Genomic Medicine have worked collaboratively to perform genome-wide association studies (GWAS) in women treated with both SERMs and AIs. On the basis of the results of the GWAS, scientists at the Mayo Clinic have proceeded with functional genomic laboratory studies. As will be seen in this review, this has led to new knowledge relating to endocrine biology that has provided a clear focus for further research to move toward truly personalized medicine for women with breast cancer. Journal of Human Genetics (2013) 58, 306–312; doi:10.1038/jhg.2013.35; published online 2 May 2013 Keywords: aromatase inhibitors; breast cancer; pharmacogenomics; tamoxifen INTRODUCTION trials were the double-blind, placebo-controlled NSABP P-1 trial of Breast cancer is the most common form of cancer in women both in tamoxifen8, and the double-blind NSABP P-2 trial that compared the United States1 and Japan.2 Endocrine therapy is the most raloxifene with tamoxifen.9,10 Combined, these two studies involved important modality in the two-thirds of patients with an estrogen over 33 000 women, which constituted about 59% of the world’s receptor (ER)-positive early breast cancer. -

Aromatase Inhibitors
FACTS FOR LIFE Aromatase Inhibitors What are aromatase inhibitors? Aromatase Inhibitors vs. Tamoxifen Aromatase inhibitors (AIs) are a type of hormone therapy used to treat some breast cancers. They AIs and tamoxifen are both hormone therapies, are taken in pill form and can be started after but they act in different ways: surgery or radiation therapy. They are only given • AIs lower the amount of estrogen in the body to postmenopausal women who have a hormone by stopping certain hormones from turning receptor-positive tumor, a tumor that needs estrogen into estrogen. If estrogen levels are low to grow. enough, the tumor cannot grow. AIs are used to stop certain hormones from turning • Tamoxifen blocks estrogen receptors on breast into estrogen. In doing so, these drugs lower the cancer cells. Estrogen is still present in normal amount of estrogen in the body. levels, but the breast cancer cells cannot get enough of it to grow. Generic/Brand names of AI’s As part of their treatment plan, some post- Generic name Brand name menopausal women will use AIs alone. Others anastrozole Arimidex will use tamoxifen for 1-5 years and then begin exemestane Aromasin using AIs. letrozole Femara Who can use aromatase inhibitors? Postmenopausal women with early stage and metastatic breast cancer are often treated with AIs. After menopause, the ovaries produce only a small amount of estrogen. AIs stop the body from making estrogen, and as a result hormone receptor-positive tumors do not get fed by estrogen and die. AIs are not given to premenopausal women because their ovaries still produce estrogen. -

Effect of Tamoxifen Or Anastrozole on Steroid Sulfatase Activity and Serum Androgen Concentrations in Postmenopausal Women with Breast Cancer
ANTICANCER RESEARCH 31: 1367-1372 (2011) Effect of Tamoxifen or Anastrozole on Steroid Sulfatase Activity and Serum Androgen Concentrations in Postmenopausal Women with Breast Cancer S.J. STANWAY1, C. PALMIERI2, F.Z. STANCZYK3, E.J. FOLKERD4, M. DOWSETT4, R. WARD2, R.C. COOMBES2, M.J. REED1† and A. PUROHIT1 1Oncology Drug Discovery Group, Section of Investigative Medicine, Imperial College London, Hammersmith Hospital, London W12 0NN, U.K.; 2Cancer Research UK Laboratories, Department of Oncology, Hammersmith Hospital, London W12 0NN, U.K.; 3Reproductive Endocrine Research Laboratory, University of Southern California, Keck School of Medicine, Women’s and Children’s Hospital, Los Angeles, CA, U.S.A.; 4Department of Biochemistry, Royal Marsden Hospital, London, SW3 6JJ, U.K. Abstract. Background: In postmenopausal women sulfate and dehydroepiandrosterone levels. Results: Neither estrogens can be formed by the aromatase pathway, which anastrozole nor tamoxifen had any significant effect on STS gives rise to estrone, and the steroid sulfatase (STS) route activity as measured in PBLs. Anastrozole did not affect which can result in the formation of estrogens and serum androstenediol concentrations. Conclusion: androstenediol, a steroid with potent estrogenic properties. Anastrozole and tamoxifen did not inhibit STS activity and Aromatase inhibitors, such as anastrozole, are now in serum androstenediol concentrations were not reduced by clinical use whereas STS inhibitors, such as STX64, are still aromatase inhibition. As androstenediol has estrogenic undergoing clinical evaluation. STX64 was recently shown properties, it is possible that the combination of an to block STS activity and reduce serum androstenediol aromatase inhibitor and STS inhibitor may give a therapeutic concentrations in postmenopausal women with breast cancer. -

Aromatase Inhibitors and Their Use in the Sequential Setting
Endocrine-Related Cancer (1999) 6 259-263 Aromatase inhibitors and their use in the sequential setting R C Coombes, C Harper-Wynne1 and M Dowsett1 Cancer Research Campaign, Department of Cancer Medicine, Division of Medicine, Imperial College School of Medicine, Charing Cross Hospital, Fulham Palace Road, London W6 8RF, UK 1Academic Department of Biochemistry, Royal Marsden Hospital, Fulham Road, London SW3 6JJ, UK (Requests for offprints should be addressed to R C Coombes) Abstract Over the past decade several novel aromatase inhibitors have been introduced into clinical practice. The discovery of these drugs followed on from the observation that the main mechanism of action of aminogluthemide was via inhibition of the enzyme aromatase thereby reducing peripheral levels of oestradiol in postmenopausal patients. The second-generation drug, 4-hydroxyandrostenedione (formestane), was introduced in 1990 and although its use was limited by its need to be given parenterally it was found to be a well-tolerated form of endocrine therapy. Third-generation inhibitors include vorozole, letrozole, anastrozole and exemestane, the former three being non-steroidal inhibitors, the latter being a steroidal inhibitor. All are capable of inhibiting aromatase action by >95% compared with 80% in the case of 4-hydroxyandrostenedione. The sequential use of different generations of aromatase inhibitors in the same patients is discussed. Studies suggest that an optimal sequence of these compounds may well result in longer remission in patients with hormone receptor positive tumours. Endocrine-Related Cancer (1999) 6 259-263 Introduction reduced, although formal trials comparing different dose regimens and using sufficient numbers of patients to The aromatase enzyme is a cytochrome P450-mediated provide the necessary statistical power have not been enzyme complex responsible for the conversion of the adequately carried out. -

Package Leaflet: Information for the User Pg1/2
Codeleserichtung / Reading direction 10 mm Codeleserichtung / Package leaflet: Information for the user Anastrozole 1mg film-coated tablets Read all of this leaflet carefully before you start using this medicine because it contains important information for Reading di you. 75 mm − Keep this leaflet. You may need to read it again. r − If you have any further questions, ask your doctor or pharmacist. ection − This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours. − If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4. What is in this leaflet: 1. What Anastrozole is and what it is used for 2. What you need to know before you take Anastrozole 3. How to take Anastrozole 4. Possible side effects 5. How to store Anastrozole 6. Contents of the pack and other information 1. What Anastrozole is and what it is used for Anastrozole belongs to a group of medicines called aromatase inhibitors. Anastrozole works by interfering with the action of an enzyme called aromatase, which affects the level of certain female sex hormones such as oestrogens. Anastrozole is used in the treatment of advanced breast cancer in post-menopausal women. 2. What you need to know before you take Anastrozole Do not take Anastrozole: − If you are allergic to anastrozole or any of the other ingredients of this medicine (listed in section 6) − If you are pregnant or breast feeding (see the section called ‘Pregnancy and breast-feeding’). -

Use of Aromatase Inhibitors in Breast Carcinoma
Endocrine-Related Cancer (1999) 6 75-92 Use of aromatase inhibitors in breast carcinoma R J Santen and H A Harvey1 Department of Medicine, University of Virginia Health Sciences Center, Charlottesville, Virginia 22908, USA 1Department of Medicine, Penn State College of Medicine, Hershey, Pennsylvania 17033, USA (Requests for offprints should be addressed to R J Santen) Abstract Aromatase, a cytochrome P-450 enzyme that catalyzes the conversion of androgens to estrogens, is the major mechanism of estrogen synthesis in the post-menopausal woman. We review some of the recent scientific advances which shed light on the biologic significance, physiology, expression and regulation of aromatase in breast tissue. Inhibition of aromatase, the terminal step in estrogen biosynthesis, provides a way of treating hormone-dependent breast cancer in older patients. Aminoglutethimide was the first widely used aromatase inhibitor but had several clinical drawbacks. Newer agents are considerably more selective, more potent, less toxic and easier to use in the clinical setting. This article reviews the clinical data supporting the use of the potent, oral competitive aromatase inhibitors anastrozole, letrozole and vorozole and the irreversible inhibitors 4-OH andro- stenedione and exemestane. The more potent compounds inhibit both peripheral and intra-tumoral aromatase. We discuss the evidence supporting the notion that aromatase inhibitors lack cross- resistance with antiestrogens and suggest that the newer, more potent compounds may have a particular application in breast cancer treatment in a setting of adaptive hypersensitivity to estrogens. Currently available aromatase inhibitors are safe and effective in the management of hormone- dependent breast cancer in post-menopausal women failing antiestrogen therapy and should now be used before progestational agents. -

Use of Aromatase Inhibitors to Treat Endometriosis-Related Pain Symptoms
Ferrero et al. Reproductive Biology and Endocrinology 2011, 9:89 http://www.rbej.com/content/9/1/89 REVIEW Open Access Use of aromatase inhibitors to treat endometriosis-related pain symptoms: a systematic review Simone Ferrero1,2*, David J Gillott2, Pier L Venturini1 and Valentino Remorgida1 Abstract This systematic review aims to assess the efficacy of aromatase inhibitors (AIs) in treating pain symptoms caused by endometriosis. A comprehensive literature search was conducted to identify all the published studies evaluating the efficacy of type II nonsteroidal aromatase inhibitors (anastrozole and letrozole) in treating endometriosis-related pain symptoms. The MEDLINE, EMBASE, PubMed, and SCOPUS databases and the Cochrane System Reviews were searched up to October 2010. This review comprises of the results of 10 publications fitting the inclusion criteria; these studies included a total of 251 women. Five studies were prospective non-comparative, four were randomized controlled trials (RCTs) and one was a prospective patient preference trial. Seven studies examined the efficacy of AIs in improving endometriosis-related pain symptoms, whilst three RCTs investigated the use of AIs as post-operative therapy in preventing the recurrence of pain symptoms after surgery for endometriosis. All the observational studies demonstrated that AIs combined with either progestogens or oral contraceptive pill reduce the severity of pain symptoms and improve quality of life. One patient preference study demonstrated that letrozole combined with norethisterone acetate is more effective in reducing pain and deep dyspareunia than norethisterone acetate alone. However, letrozole causes a higher incidence of adverse effects and does not improve patients’ satisfaction or influence recurrence of symptoms after discontinuation of treatment. -

Pms-ANASTROZOLE
PRODUCT MONOGRAPH Prpms-ANASTROZOLE Anastrozole Tablets 1 mg Non-Steroidal Aromatase Inhibitor PHARMASCIENCE INC. Date of Revision: 6111 Royalmount Ave., Suite 100 June 9, 2015 Montréal, Québec, H4P 2T4 www.pharmascience.com Submission Control No.: 184951 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION .........................................................3 SUMMARY PRODUCT INFORMATION ........................................................................3 INDICATIONS AND CLINICAL USE ..............................................................................3 CONTRAINDICATIONS ...................................................................................................3 WARNINGS AND PRECAUTIONS ..................................................................................4 ADVERSE REACTIONS ....................................................................................................7 DRUG INTERACTIONS ..................................................................................................17 DOSAGE AND ADMINISTRATION ..............................................................................19 OVERDOSAGE ................................................................................................................20 ACTION AND CLINICAL PHARMACOLOGY ............................................................20 STORAGE AND STABILITY ..........................................................................................23 SPECIAL HANDLING INSTRUCTIONS .......................................................................23 -

Anastrozole Versus Tamoxifen Treatment in Postmenopausal
Cancer Therapy: Clinical Anastrozole versus Tamoxifen Treatment in Postmenopausal Women with Endocrine-Responsive Breast Cancer and Tamoxifen-Induced Endometrial Pathology Bernd Gerber,1, 2 Annette Krause,1, 2 Toralf Reimer,2 Ionas Mylonas,1, 2 Josef Makovitzky,3 Gu« nther Kundt,4 and Wolfgang Janni1 Abstract Purpose:Toinvestigate the effect of switching from adjuvant tamoxifen to anastrozole (Arimidex) treatment in postmenopausal women with endocrine-responsive breast cancer and histologically proven tamoxifen-induced benign endometrial pathology. Experimental Design: Two hundred twenty-six postmenopausal women who had received adjuvant tamoxifen 20 mg/d (z12 months , V48 months) and developed abnormal vaginal bleed- ing and/or an asymptomatic endometrial thickness >10 mm [measured by transvaginal ultrasound (TVUS)] were subjected to hysteroscopy and dilation and curettage (D&C). Thereafter, 171 patients were randomized in a phase III study to continue tamoxifen treatment (n = 88) or switch to anastrozole1mg/d (n = 83).Patients were monitored for V42 months usingTVUS at 6-monthly intervals. Results: At study entry, there were no significant differences in vaginal bleeding, endometrial thickness, and histologic findings between the two treatment groups. Throughout the treatment period, there was no significant difference in recurrent vaginal bleeding between groups [anastro- zole, 4 of 83 (4.8%); tamoxifen, 9 of 88 (10.2%); P = 0.18]. Six months after randomization, the mean endometrial thickness for patients who switched to anastrozole was significantly reduced compared with those who continued tamoxifen treatment (P < 0.0001). Significantly fewer anas- trozole patients required a repeat hysteroscopy and D&C compared with those on tamoxifen [4of83(4.8%)and29of88(33.0%),respectively;P < 0.0001]. -

Estradiol for the Mitigation of Adverse Effects of Androgen Deprivation Therapy
248 N Russell et al. Estradiol and androgen 24:8 R297–R313 Review deprivation therapy Estradiol for the mitigation of adverse effects of androgen deprivation therapy Nicholas Russell1,2, Ada Cheung1,2 and Mathis Grossmann1,2 Correspondence should be addressed 1 Department of Endocrinology, Austin Health, Heidelberg, Victoria, Australia to N Russell 2 Department of Medicine (Austin Health), The University of Melbourne, Heidelberg, Victoria, Australia Email [email protected] Abstract Prostate cancer (PCa) is the second most commonly diagnosed cancer in men. Key Words Conventional endocrine treatment for PCa leads to global sex steroid deprivation. f endocrine therapy The ensuing severe hypogonadism is associated with well-documented adverse effects. f prostate Recently, it has become apparent that many of the biological actions attributed to f estrogen androgens in men are in fact not direct, but mediated by estradiol. Available evidence f androgen supports a primary role for estradiol in vasomotor stability, skeletal maturation and f testosterone maintenance, and prevention of fat accumulation. Hence there has been interest in revisiting estradiol as a treatment for PCa. Potential roles for estradiol could be in lieu of conventional androgen deprivation therapy or as low-dose add-back treatment while continuing androgen deprivation therapy. These strategies may limit some of the side Endocrine-Related Cancer Endocrine-Related effects associated with conventional androgen deprivation therapy. However, although available data are reassuring, the potential for cardiovascular risk and pro-carcinogenic Endocrine-Related Cancer effects on PCa via estrogen receptor signalling must be considered. (2017) 24, R297–R313 Introduction Prostate cancer (PCa) is the second most commonly and extragonadal androgen synthesis inhibitors. -

Pilot Study Evaluating the Pharmacokinetics, Pharmacodynamics, and Safety of the Combination of Exemestane and Tamoxifen
Vol. 10, 1943–1948, March 15, 2004 Clinical Cancer Research 1943 Pilot Study Evaluating the Pharmacokinetics, Pharmacodynamics, and Safety of the Combination of Exemestane and Tamoxifen Edgardo Rivera,1 Vicente Valero,1 pharmacokinetics or pharmacodynamics and that the com- Deborah Francis,1 Aviva G. Asnis,2 bination is well-tolerated and active. Further clinical inves- Larry J. Schaaf,2 Barbara Duncan,2 and tigation is warranted. Gabriel N. Hortobagyi1 1Department of Breast Medical Oncology, The University of Texas INTRODUCTION 2 M. D. Anderson Cancer Center, Houston, Texas, and Pharmacia Breast cancer growth frequently is promoted by estrogen, Corporation, Peapack, New Jersey and approximately one-third of tumors respond to estrogen deprivation therapy (1). In current clinical practice, two main ABSTRACT single-agent strategies are used to deprive breast cancer cells of Purpose: We conducted a pilot study assessing the ef- estrogen. A selective estrogen receptor modulator (SERM), such fects of the selective estrogen receptor modulator, tamox- as tamoxifen, is given to block binding of the hormone to the ifen, on the pharmacokinetics, pharmacodynamics, and cancer cells. Alternately, in postmenopausal women, an inhib- safety of the steroidal, irreversible aromatase inhibitor (AI), itor of the enzyme, aromatase, is administered to suppress their exemestane, when the two were coadministered in post- main source of estrogen synthesis, conversion of androgens by menopausal women with metastatic breast cancer. this enzyme. Experimental Design: Patients with documented or un- One aromatase inhibitor (AI) that has been studied exten- known hormone receptor sensitivity were eligible. Patients sively and shown activity as a single agent in postmenopausal received oral exemestane at 25-mg once daily. -

Use of Endocrine Therapy for Breast Cancer Risk Reduction: Asco Clinical Practice Guideline Update
USE OF ENDOCRINE THERAPY FOR BREAST CANCER RISK REDUCTION: ASCO CLINICAL PRACTICE GUIDELINE UPDATE Agent Recommendation Evidence Rating Should be discussed as an option to reduce the risk of invasive BC, specifically estrogen (ER)-positive breast cancer, in premenopausal women who are ≥ 35 years of age with a 5-year projected absolute BC risk ≥ 1.66% or with LCIS. Risk reduction benefit continue for at least 10 years. Is not recommended for use in women with a history of deep vein thrombosis, pulmonary embolus, stroke, transient ischemic attack, or during prolonged immobilization. Type: Evidence-based Is not recommended for women who are pregnant, women who may become pregnant, or nursing Evidence quality: High Tamoxifen mothers. Strength of Is not recommended in combination with hormone therapy. recommendation: Strong Follow-up should include a timely work-up of abnormal vaginal bleeding. Discussions with patients and health care providers should include both the risks and benefits of tamoxifen in the preventive setting. DOSAGE: 20 mg/d orally for 5 years. Should be discussed as an option to reduce the risk of invasive BC, specifically estrogen (ER)-positive breast cancer, in postmenopausal women who are ≥ 35 years of age with a 5-year projected absolute BC risk ≥ 1.66% or with LCIS. Type: Evidence-based Evidence quality: High Raloxifene May be used longer than 5 years in women with osteoporosis, in whom BC risk reduction is a secondary Strength of benefit. recommendation: Strong Should not be used for BC risk reduction in premenopausal women. Is not recommended for use in women with a history of deep vein thrombosis, pulmonary embolus, stroke, or transient ischemic attack, or during prolonged immobilization.