Multiple Acantholytic Dyskeratotic Acanthomas in a Liver- Transplant Recipient
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Glossary for Narrative Writing
Periodontal Assessment and Treatment Planning Gingival description Color: o pink o erythematous o cyanotic o racial pigmentation o metallic pigmentation o uniformity Contour: o recession o clefts o enlarged papillae o cratered papillae o blunted papillae o highly rolled o bulbous o knife-edged o scalloped o stippled Consistency: o firm o edematous o hyperplastic o fibrotic Band of gingiva: o amount o quality o location o treatability Bleeding tendency: o sulcus base, lining o gingival margins Suppuration Sinus tract formation Pocket depths Pseudopockets Frena Pain Other pathology Dental Description Defective restorations: o overhangs o open contacts o poor contours Fractured cusps 1 ww.links2success.biz [email protected] 914-303-6464 Caries Deposits: o Type . plaque . calculus . stain . matera alba o Location . supragingival . subgingival o Severity . mild . moderate . severe Wear facets Percussion sensitivity Tooth vitality Attrition, erosion, abrasion Occlusal plane level Occlusion findings Furcations Mobility Fremitus Radiographic findings Film dates Crown:root ratio Amount of bone loss o horizontal; vertical o localized; generalized Root length and shape Overhangs Bulbous crowns Fenestrations Dehiscences Tooth resorption Retained root tips Impacted teeth Root proximities Tilted teeth Radiolucencies/opacities Etiologic factors Local: o plaque o calculus o overhangs 2 ww.links2success.biz [email protected] 914-303-6464 o orthodontic apparatus o open margins o open contacts o improper -

Case Report Sialadenoma Papilliferum: Clinical Misdiagnosis with a Histological Decree
Hindawi Publishing Corporation Case Reports in Dentistry Volume 2012, Article ID 356271, 4 pages doi:10.1155/2012/356271 Case Report Sialadenoma Papilliferum: Clinical Misdiagnosis with a Histological Decree A. Anuradha,1, 2 V. V. S. Ram Pr asad, 1 Bina Kashyap,1 and Vijay Srinivas1 1 Department of Oral Pathology, Saint Joseph Dental College and Hospital, Duggirala, Eluru, 534004, India 2 Anuradha ENT Hospital, Eluru Road, Gudivada, Krishna 521301, India Correspondence should be addressed to A. Anuradha, [email protected] Received 28 November 2011; Accepted 15 January 2012 Academic Editor: A. Epivatianos Copyright © 2012 A. Anuradha et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Sialadenoma papilliferum is a rare salivary gland tumor clinically resembling papilloma originating probably from the excretory duct. It is characterized by a biphasic growth pattern of exophytic squamous component and endophytic glandular component. We report a rare case of sialadenoma papilliferum in the floor of the mouth with epithelial dysplasia with pertinent review of literature. The present case highlights the importance of keeping sialadenoma papilliferum as a differential diagnosis of exophytic papilliferous oral lesions and the need to explore the etiology and malignant potential of the tumor. 1. Introduction Clinically, the lesion was well circumscribed, white, and 1 cm diameter with a rough papilliferous surface. It was Sialadenoma papilliferum (SP) is a rare, distinctive benign provisionally diagnosed as papilloma and excision of the tumor of salivary gland classified under the ductal papillo- lesion was done under local anesthesia. -

The Tamilnadu Dr. M.G.R. Medical University Chennai, Tamil Nadu
CLINICO-PATHOLOGICAL STUDY OF SKIN SURFACE EPIDERMAL AND APPENDAGEAL TUMOURS Dissertation Submitted in partial fulfillment of university regulations for M.D. DEGREE IN DERMATOLOGY, VENEREOLOGY AND LEPROSY BRANCH XII – A THE TAMILNADU DR. M.G.R. MEDICAL UNIVERSITY CHENNAI, TAMIL NADU SEPTEMBER 2006 CERTIFICATE This is to certify that this Dissertation entitled “CLINICO-PATHOLOGICAL STUDY OF SKIN SURFACE EPIDERMAL AND APPENDAGEAL TUMOURS” is a bonafide work done by DR.G.BALAJI, Postgraduate student of Department of Dermatology, Leprosy and Institute of STD, Madras Medical College and Government General Hospital, Chennai – 3 for the award of Degree of M.D.( Dermatology, Venereology and Leprosy ) Branch XII – A during the academic year of 2003-2006. This work has not previously formed in the basis for the award of any degree or diploma. Prof. Dr. B. Parveen, MD., DD., Professor & Head, Dept. of Dermatology and Leprosy, Madras Medical College & Govt. General Hospital, Chennai – 3. Prof. Dr. Kalavathy Ponniraivan, MD., The Dean Madras Medical College & Govt. General Hospital, Chennai – 3. SPECIAL ACKNOWLEDGEMENT I sincerely thank Prof. Dr. Kalavathy Ponniraivan, MD., Dean, Madras Medical College & Govt. General Hospital, Chennai – 3, for granting me permission to use the resources of this institution for my study. ACKNOWLEDGEMENT I sincerely thank Prof. B.Parveen MD.,DD, Professor and Head of Department of Dermatology for her invaluable guidance and encouragement for the successful completion of this study. I express my heart felt gratitude to Dr.N.Gomathy MD.,DD, former Head of department of Dermatology who was instrumental in the initiation of this project, giving constant guidance throughout my work. -

Cutaneous Horn: a Potentially Malignant Entity
Letter to the editor Cutaneous horn: a potentially malignant entity Cutaneous horn: a potentially malignant entity N. F. Fernandes, S. Sinha, W. C. Lambert, and R. A. Schwartz S UMMARY A cutaneous horn is a conical, dense, hyperkeratotic protrusion that often appears similar to the horn of an animal. It is a morphologic designation referring to an unusually cohesive keratinized material, not a true pathologic diagnosis. Cutaneous horns occur in association with, or as a re- sponse to, a wide variety of underlying benign, pre-malignant, and malignant cutaneous diseases. The most important common concern is distinguishing a hyperkeratotic actinic keratosis from a cutaneous squamous cell carcinoma. Keratoacanthoma is another cause, as illustrated herein as a projective cutaneous tumor with a fingernail-like appearance. The treatment of choice for cuta- neous horns is shave excision with subsequent histopathologic evaluation to rule out underlying malignancy and to guide potential further therapy. KEYIntroduction with the characterization of cutaneous horns as a WORDS medical disorder in the late eighteenth century (2). A cutaneous horn is a conical, dense hyperkeratotic cutaneous protrusion that often resembles the horn of an Epidemiology and etiology horn, cornu animal. The earliest documented case of cutaneous cutaneum, horn, or cornu cutaneum, was that of an elderly Welsh Cutaneous horns are nodules composed of hyperkerato- woman in London who was displayed commercially compact keratin that project above the surface of sis, actinic as an anomaly of nature in 1588 (1). There were the skin. They differ from animal horns by the keratosis, several other accounts of cutaneous horns in the absence of a central bone. -

Oral Verruciform Xanthoma: Report of 13 New Cases and Review of the Literature
Med Oral Patol Oral Cir Bucal. 2018 Jul 1;23 (4):e429-35. Oral verruciform xanthoma Journal section: Oral Medicine and Pathology doi:10.4317/medoral.22342 Publication Types: Review http://dx.doi.org/doi:10.4317/medoral.22342 Oral verruciform xanthoma: Report of 13 new cases and review of the literature Paris Tamiolakis 1, Vasileios I. Theofilou 1, Konstantinos I. Tosios 2, Alexandra Sklavounou-Andrikopoulou 3 1 DDS, Postgraduate Student, Department of Oral Medicine and Oral Pathology, School of Dentistry, National and Kapodistrian University of Athens, Greece, 2 Thivon Str, 115 27 Athens, Greece 2 DDS, PhD, Assistant Professor, Department of Oral Medicine and Oral Pathology, School of Dentistry, National and Kapodis- trian University of Athens, Greece, 2 Thivon Str, 115 27 Athens, Greece 3 DDS, MSc, PhD, Professor, Head of Department of Oral Medicine and Oral Pathology, School of Dentistry, National and Ka- podistrian University of Athens, Greece, 2 Thivon Str, 115 27 Athens, Greece Correspondence: Department of Oral Medicine and Oral Pathology School of Dentistry National and Kapodistrian University of Athens Greece, 2 Thivon Str, 11527, Goudi, Athens, Greece [email protected] Tamiolakis P, Theofilou VI, Tosios KI, Sklavounou-Andrikopoulou A. Oral verruciform xanthoma: Report of 13 new cases and review of the literature. Med Oral Patol Oral Cir Bucal. 2018 Jul 1;23 (4):e429-35. http://www.medicinaoral.com/medoralfree01/v23i4/medoralv23i4p429.pdf Received: 05/01/2018 Accepted: 09/05/2018 Article Number: 22342 http://www.medicinaoral.com/ © Medicina Oral S. L. C.I.F. B 96689336 - pISSN 1698-4447 - eISSN: 1698-6946 eMail: [email protected] Indexed in: Science Citation Index Expanded Journal Citation Reports Index Medicus, MEDLINE, PubMed Scopus, Embase and Emcare Indice Médico Español Abstract Background: Oral verruciform xanthoma (OVX) is a rare lesion. -

Expert-Level Diagnosis of Nonpigmented Skin Cancer by Combined Convolutional Neural Networks
Supplementary Online Content Tschandl P, Rosendahl C, Akay BN, et al. Expert-level diagnosis of nonpigmented skin cancer by combined convolutional neural networks. JAMA Dermatol. Published online November 28, 2018. doi:10.1001/jamadermatol.2018.4378 eFigure. Sensitivities (Blue) and Specificities (Orange) at Different Threshold Cutoffs (Green) of the Combined Classifier Evaluated on the Validation Set eAppendix. Neural Network Training eTable 1. Complete List of Diagnoses and Their Frequencies Within the Test-Set eTable 2. Education of Users According to Their Experience Group eTable 3. Percent of Correct Prediction of the Malignancy Status for Specific Diagnoses of a CNN Using Either Close-up or Dermatoscopic Images This supplementary material has been provided by the authors to give readers additional information about their work. © 2018 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 09/25/2021 eFigure. Sensitivities (Blue) and Specificities (Orange) at Different Threshold Cutoffs (Green) of the Combined Classifier Evaluated on the Validation Set A threshold cut at 0.2 (black) is found for a minimum of 51.3% specificity. © 2018 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 09/25/2021 eAppendix. Neural Network Training We compared multiple architecture and training hyperparameter combinations in a grid-search fashion, and used only the single best performing network for dermoscopic and close-up images, based on validation accuracy, for further analyses. We trained four different CNN architectures (InceptionResNetV2, InceptionV3, Xception, ResNet50) and used model definitions and ImageNet pretrained weights as available in the Tensorflow (version 1.3.0)/ Keras (version 2.0.8) frameworks. -

Vulvar Verruciform Xanthoma Ten Cases Associated with Lichen Sclerosus, Lichen Planus, Or Other Conditions
OBSERVATION ONLINE FIRST Vulvar Verruciform Xanthoma Ten Cases Associated With Lichen Sclerosus, Lichen Planus, or Other Conditions Charlotte Fite, MD; Franc¸oise Plantier, MD; Nicolas Dupin, MD, PhD; Marie-Franc¸oise Avril, MD; Micheline Moyal-Barracco, MD Background: Verruciform xanthoma (VX) is a rare be- acanthosis without atypia, and elongated rete ridges. nign tumor that usually involves the oral cavity. Since Xanthomatous cells were aggregated in the papillary the first report of this tumor in 1971, only 9 cases have dermis. been reported on the vulva, and 3 of these were associ- ated with another vulvar condition. We describe the clini- Conclusions: Vulvar VX is a benign tumor with mis- copathologic features of 10 patients with vulvar VX and leading clinical features. All 10 cases were associated with focus on their associated conditions. a vulvar condition, mainly a lichen sclerosus. There- fore, VX might represent a reaction pattern induced by Observation: The mean age of the patients was 68 years different conditions, mainly characterized by damage to (range, 51-80 years). The VX lesions were asymptom- the dermoepidermal junction. When confronted with the atic, yellowish-orange verrucous plaques. The diagno- diagnosis of vulvar VX, clinicians may look for an asso- sis was clinically suspected in 2 cases; other suggested ciated vulvar condition. diagnoses were condyloma or squamous cell carci- noma. All of the patients had an associated vulvar con- dition: lichen sclerosus (6 patients), lichen planus (2 Arch Dermatol. 2011;147(9):1087-1092. patients), Paget disease, or radiodermatitis. Under mi- Published online May 16, 2011. croscopy, the VX lesions displayed parakeratosis, doi:10.1001/archdermatol.2011.113 ERRUCIFORM XANTHOMA location, histologic findings, history of dyslip- (VX) is a rare benign tu- idemia, treatment, follow-up, and associated mor which was first vulvar conditions. -
Epidermolytic Acanthoma: a Case Report Ginsberg AS, Rajagopalan A, Terlizzi JP
ISSN 2307-8960 (online) World Journal of Clinical Cases World J Clin Cases 2020 September 26; 8(18): 3920-4279 Published by Baishideng Publishing Group Inc World Journal of W J C C Clinical Cases Contents Semimonthly Volume 8 Number 18 September 26, 2020 OPINION REVIEW 3920 Special features of SARS-CoV-2 in daily practice Charitos IA, Ballini A, Bottalico L, Cantore S, Passarelli PC, Inchingolo F, D'Addona A, Santacroce L EVIDENCE REVIEW 3934 Gastrointestinal insights during the COVID-19 epidemic Nie K, Yang YY, Deng MZ, Wang XY REVIEW 3942 From infections to autoimmunity: Diagnostic challenges in common variable immunodeficiency Więsik-Szewczyk E, Jahnz-Różyk K 3956 One disease, many faces-typical and atypical presentations of SARS-CoV-2 infection-related COVID-19 disease Philips CA, Mohan N, Ahamed R, Kumbar S, Rajesh S, George T, Mohanan M, Augustine P MINIREVIEWS 3971 Application of artificial neural networks in detection and diagnosis of gastrointestinal and liver tumors Mao WB, Lyu JY, Vaishnani DK, Lyu YM, Gong W, Xue XL, Shentu YP, Ma J 3978 Hepatic epithelioid hemangioendothelioma: Update on diagnosis and therapy Kou K, Chen YG, Zhou JP, Sun XD, Sun DW, Li SX, Lv GY ORIGINAL ARTICLE Clinical and Translational Research 3988 Streptococcus agalactiae: Identification methods, antimicrobial susceptibility, and resistance genes in pregnant women Santana FAF, de Oliveira TVL, Filho MBDS, da Silva LSC, de Brito BB, de Melo FF, Souza CL, Marques LM, Oliveira MV 3999 Twelve-month evaluation of the atraumatic restorative treatment approach -

Seborrheic Keratosis
Benign Epidermal and Dermal Tumors REAGAN ANDERSON, DO- PROGRAM DIRECTOR, COLORADO DERMATOLOGY INSTITUTE, RVU PGY3 RESIDENTS- JONATHAN BIELFIELD, GEORGE BRANT PGY2 RESIDENT- MICHELLE ELWAY Seborrheic Keratosis Common benign growth seen after third/fourth decade of life Ubiquitous among older individuals Tan to black, macular, papular, or verrucous lesion Occur everywhere except palms, soles, and mucous membranes Can simulate melanocytic neoplasms Pathogenesis: Sun exposure- Australian study found higher incidence in the head/neck Alteration in distribution of epidermal growth factors Somatic activating mutations in fibroblast growth factor receptor and phosphoinositide-3-kinase Seborrheic Keratosis Sign of Leser-Trelat: Rare cutaneous marker of internal malignancy • Gastric/colonic adenocarcinoma, breast carcinoma, and lymphoma m/c • Abrupt increase in number/size of SKs that can occur before, during, or after an internal malignancy is detected • 40% pruritus • M/C location is the back • Malignant acanthosis nigricans may also appear in 20% of patients • Should resolve when primary tumor is treated, and reappear with recurrence/mets Seborrheic Keratosis 6 Histologic types Acanthotic Hyperkeratotic Reticulated Irritated Clonal Melanoacanthoma Borst-Jadassohn phenomenon Well-demarcated nests of keratinocytes within the epidermis Seborrheic Keratoses Treatment Reassurance Irritated SKs (itching, catching on clothes, inflamed) Cryotherapy, curettage, shave excision Pulsed CO2, erbium:YAG lasers Electrodessication Flegel -

Statistical Analysis Plan
Cover Page for Statistical Analysis Plan Sponsor name: Novo Nordisk A/S NCT number NCT03061214 Sponsor trial ID: NN9535-4114 Official title of study: SUSTAINTM CHINA - Efficacy and safety of semaglutide once-weekly versus sitagliptin once-daily as add-on to metformin in subjects with type 2 diabetes Document date: 22 August 2019 Semaglutide s.c (Ozempic®) Date: 22 August 2019 Novo Nordisk Trial ID: NN9535-4114 Version: 1.0 CONFIDENTIAL Clinical Trial Report Status: Final Appendix 16.1.9 16.1.9 Documentation of statistical methods List of contents Statistical analysis plan...................................................................................................................... /LQN Statistical documentation................................................................................................................... /LQN Redacted VWDWLVWLFDODQDO\VLVSODQ Includes redaction of personal identifiable information only. Statistical Analysis Plan Date: 28 May 2019 Novo Nordisk Trial ID: NN9535-4114 Version: 1.0 CONFIDENTIAL UTN:U1111-1149-0432 Status: Final EudraCT No.:NA Page: 1 of 30 Statistical Analysis Plan Trial ID: NN9535-4114 Efficacy and safety of semaglutide once-weekly versus sitagliptin once-daily as add-on to metformin in subjects with type 2 diabetes Author Biostatistics Semaglutide s.c. This confidential document is the property of Novo Nordisk. No unpublished information contained herein may be disclosed without prior written approval from Novo Nordisk. Access to this document must be restricted to relevant parties.This -

UC Davis Dermatology Online Journal
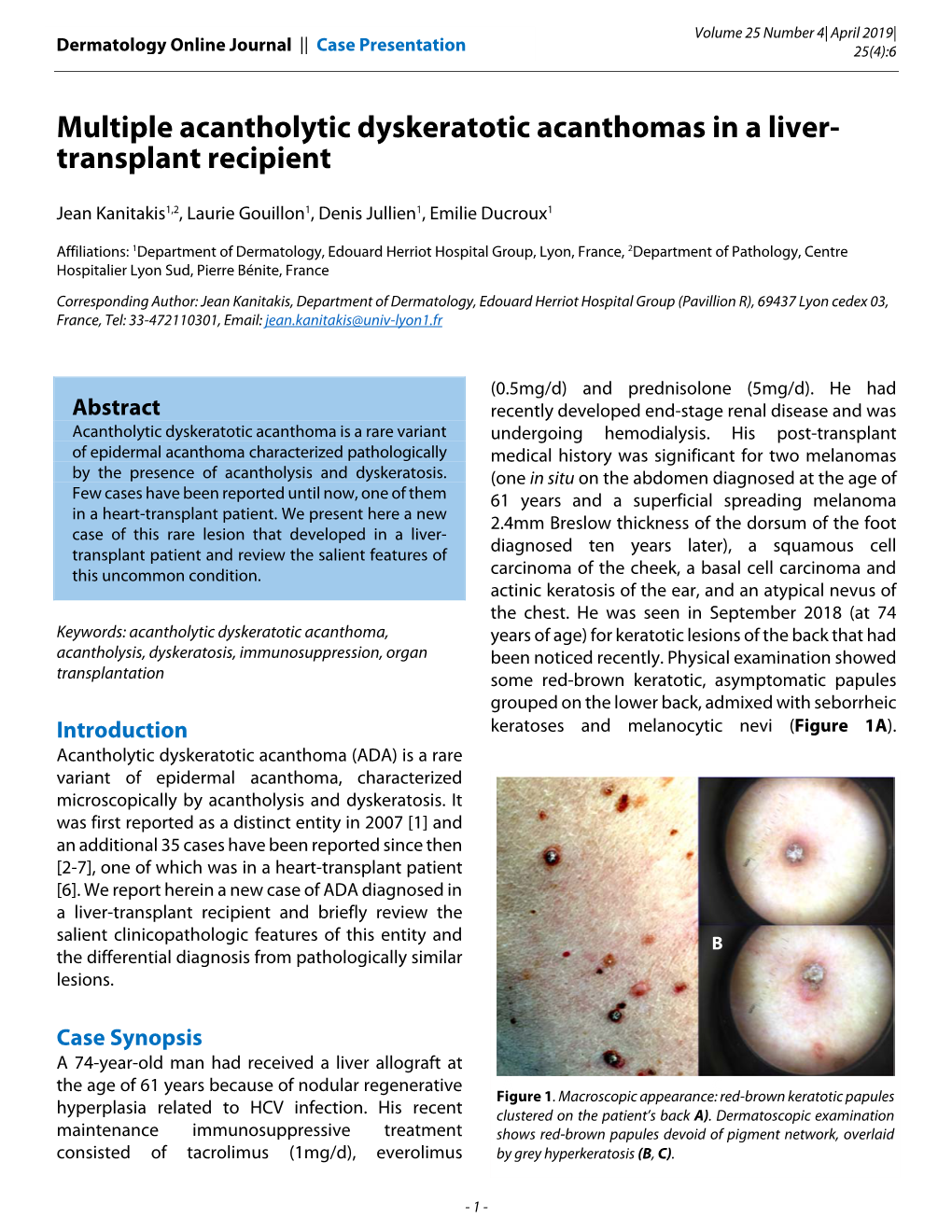
UC Davis Dermatology Online Journal Title Multiple acantholytic dyskeratotic acanthomas in a liver-transplant recipient Permalink https://escholarship.org/uc/item/24v5t78z Journal Dermatology Online Journal, 25(4) Authors Kanitakis, Jean Gouillon, Laurie Jullien, Denis et al. Publication Date 2019 DOI 10.5070/D3254043575 License https://creativecommons.org/licenses/by-nc-nd/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Volume 25 Number 4| April 2019| Dermatology Online Journal || Case Presentation 25(4):6 Multiple acantholytic dyskeratotic acanthomas in a liver- transplant recipient Jean Kanitakis1,2, Laurie Gouillon1, Denis Jullien1, Emilie Ducroux1 Affiliations: 1Department of Dermatology, Edouard Herriot Hospital Group, Lyon, France, 2Department of Pathology, Centre Hospitalier Lyon Sud, Pierre Bénite, France Corresponding Author: Jean Kanitakis, Department of Dermatology, Edouard Herriot Hospital Group (Pavillion R), 69437 Lyon cedex 03, France, Tel: 33-472110301, Email: [email protected] (0.5mg/d) and prednisolone (5mg/d). He had Abstract recently developed end-stage renal disease and was Acantholytic dyskeratotic acanthoma is a rare variant undergoing hemodialysis. His post-transplant of epidermal acanthoma characterized pathologically medical history was significant for two melanomas by the presence of acantholysis and dyskeratosis. (one in situ on the abdomen diagnosed at the age of Few cases have been reported until now, one of them 61 years and a superficial spreading melanoma in a heart-transplant patient. We present here a new 2.4mm Breslow thickness of the dorsum of the foot case of this rare lesion that developed in a liver- diagnosed ten years later), a squamous cell transplant patient and review the salient features of this uncommon condition. -

Conference 15 28 January 2009
The Armed Forces Institute of Pathology Department of Veterinary Pathology Conference Coordinator: Todd M. Bell, DVM WEDNESDAY SLIDE CONFERENCE 2008-2009 Conference 15 28 January 2009 Conference Moderator: Michael H. Goldschmidt, BVMS, MRCVS, DACVP of only one or two layers of partly flattened keratinocytes, CASE I – T8944-07 (AFIP 3102252) interpreted as severe epidermal atrophy (Fig. 1-2), and is covered by a layer of lamellar eosinophilic material Signalment: 2-year-old female neutered Siamese cat, (lamellar orthokeratotic hyperkeratosis). Superficial and feline, (Felis catus) periadnexal dermis show a perivascular to interstitial infiltrate composed of moderate numbers of lymphocytes, History: The cat was presented to the clinician with less macrophages, neutrophils and mast cells, and a few a 9 month history of prednisolone treatment due to a eosinophils and plasma cells. Around vessels of the diagnosis of food hypersensitivity. The skin of the dorsum superficial vascular plexus there are moderate numbers resembled wet tissue paper and was sensitive to touch. of extravasated erythrocytes (haemorrhage). Dermal From the left and right thigh, blood vessels were directed collagen is extremely attenuated and shows a pale towards the lesion (figures). The practitioner excised a 13 staining in H&E stained sections. Adnexal structures x 4 x 0.3 cm skin sample, which showed several tears and demonstrate a complete lack of anagen hair follicles, and detachment of the dermis from the panniculus (Fig. 1-1). the perifollicular fibrous sheaths of many telogen follicles The sample was fixed in formalin and routinely processed are thickened. Sebaceous glands are decreased in size and for histopathological evaluation.