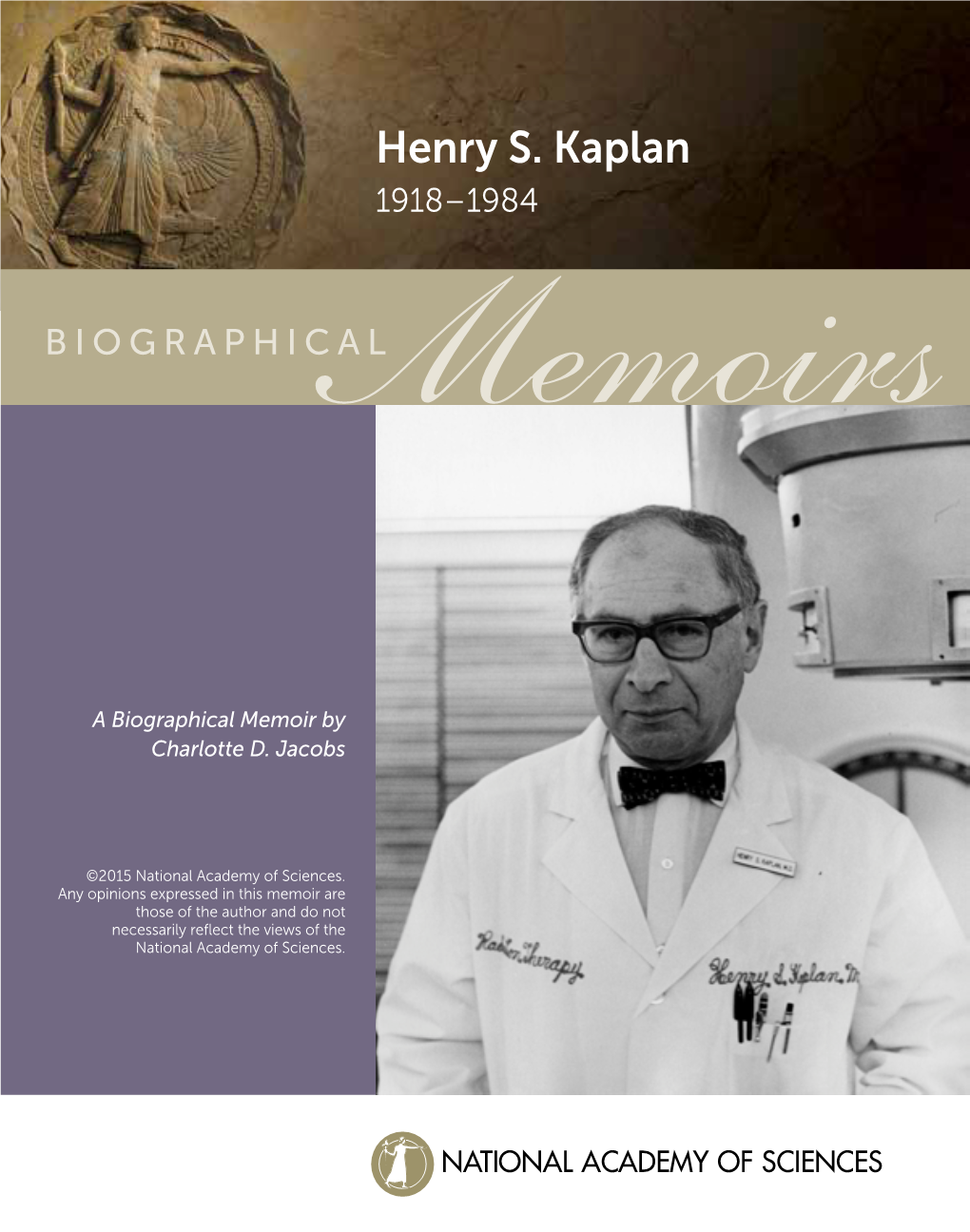
Henry S. Kaplan 1918–1984
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CURRICULUM VITAE Sarah S. Donaldson, M.D. IDENTIFYING DATA Born
CURRICULUM VITAE Sarah S. Donaldson, M.D. IDENTIFYING DATA Born - Portland, Oregon Nationality - American ACADEMIC HISTORY Colleges and Universities University of Oregon; Eugene, Oregon 9/56-6/58 University of Oregon School of Nursing; Portland, Oregon 9/58-6/61 Portland State College; Portland, Oregon 9/62-6/64 Dartmouth Medical School; Hanover, New Hampshire 9/64-6/66 Harvard Medical School; Boston, Massachusetts 9/66-6/68 Degrees with Dates Received B.S., R.N. 6/61 B.M.S. 6/66 M.D. 6/68 Scholarships and Honors Student Nurse of the Year 1961 Scholarship to Dartmouth Medical School 1964-66 Scholarship to Harvard Medical School 1966-68 Anna Fuller Award 1973-74 American College of Radiology, Fellowship (FACR) 9/1/87 Lucy Wortham James Clinical Research Award from the Society of Surgical Oncology 5/88 Riley Cancer Research for Children Distinguished Lecturer 1991 Catharine and Howard Avery Professor in the School of Medicine 1991 Dartmouth College Presidential Medal for Outstanding Leadership and Achievement 11/91 Edward A. Langdon Lecturer, UCLA Medical School 1992 6/2/2016 (VD) Sarah S. Donaldson, M.D. Page 2 The Henry S. Kaplan Memorial Prize for Teaching 1993, 2010 Canadian Association of Radiation Oncologists (CARO) 1993 Lecturer 1993 Franz Buschke Distinguished Lecturer 1994 XXIst Annual Myron Karon Memorial Lecturer 1995 Radiation Oncology Orator for Radiological Society 1995 of North America First Annual Robert C. Storrs Lecture 1996 First Distinguished Women in Medicine and Science Lecturer Northwestern University Medical School -

Myths About Stanford's Interactions with Industry Timothy Lenoir
Myths about Stanford’s Interactions with Industry Timothy Lenoir Department of History Stanford University Draft: September 6, 2004 Stanford is typically featured as a paradigm example among universities generating innovations that lead to new technology-based firms; and indeed, Stanford entrepreneurial activity is generally regarded as virtually synonymous with the birth of Silicon Valley. This is the stuff of legend, but it is based in fact: In a study conducted in 2000 Tom Byers and colleagues argued that Stanford alumni and faculty account for more than 1800 technology based firms in the Silicon Valley responsible for 37 percent of all high-tech employment in the region1; and in his contribution to the Silicon Valley Edge, Jim Gibbons, himself a Silicon Valley legend, argued that Stanford technology startups, including Hewlett-Packard, accounted for 60 percent of Silicon Valley revenues in 1988 and 1996 if Hewlett-Packard is included in the accounting and slightly over 50 percent if HP is left out of the mix.2 But such accounts can be misleading. While it is undoubtedly correct that Stanford has been a significant factor in the formation of Silicon Valley undue emphasis on Stanford’s contributions can contribute to the myth that Stanford’s interaction with industry is a one way relationship. A second, equally distorted description of Stanford’s relation to industry is the view that in the wake of a continuous decline in federal funding for academic research over the past decade Stanford has somehow become the captive of industry funding, and that in the aftermath of Bayh-Dole and the gold rush on biotechnology patents, Stanford has become a “kept university” seeking to turn its intellectual property into a cash cow to keep up in the research game. -

Henry S. Kaplan 1918-1984 2739
Obituary OBITUARY Henry S. Kaplan 1918-1984 Dr. Henry S. Kaplan died on February 4,1984, at the age of Charles F. Kettering Prize, the French Griffuel Prize, and numer 65, of cancer of the lung. A nonsmoker, he succumbed to the ous others. disease which he dedicated his life to understand and treat. His Shortly before his death, he was asked what he hoped he contributions to cancer research and therapy, spanning almost would be most remembered for. He responded: a 40-year period, are unparalleled in their importance and diver "I'd like to be remembered for my accomplishments that stand the test of time such as the work on Hodgkin's disease and sity during this era. Bom in Chicago on April 24, 1918, his interest in medicine malignant lymphomas. That is an area where there will be began at age 15 when his father died of lung cancer. He continued further improvement, but I think we contributed a graduated from the University of Chicago at age 20 and Chica foundation stone which today is leading to the cure world-wide go's Rush Medical College at age 22. By age 25, he had of hundreds of thousands of patients." "It's hard for me to know whether my work on mouse virus or completed his housestaff training at the Michael Reese Hospital and a residency in radiology at the University of Minnesota. He radiation-induced lymphomas will be remembered or not. I hap pen to think it's very interesting, but I have the feeling people held positions at Yale University and the National Cancer Institute tend to gloss over it." before being appointed as Professor and Chairman of the De "I'd like to be remembered as the co-developer of the medical partment of Radiology at Stanford University in 1948. -

Clinicalcancerprogram
The Clinical CancerProgram at YALE by david s. fischer, md THE SMILOW CANCER HOSPITAL AT YALE-NEW HAVEN sterling hall of medicine on 200th anniversary of yale school of medicine david s. fischer, md david the smilow cancer hospital at yale-new haven 2009 Notice: Every effort has been made to ensure that the facts in this publication are correct, but since some of this is oral history, errors will occur in spite of attempts to verify the facts in published accounts. In a few instances, published accounts were apparently in error according to reports of multiple individuals who had contemporary personal knowledge of the events. The interpretation of events is subjective and individuals may view them differently. The opinions and interpretations herein are the responsibility of the author and not of the individuals consulted or those who reviewed all or portions of the manuscript. Y printing and publishing services Frank Savino, Publication Operations Andrea Porto, Graphic Designer, Prepress Operator John Heine, Design and Prepress Copyright 2012 by David S. Fischer, MD ISBN 978-0-9797398-6-6 The Clinical Cancer Program at Yale Table of Contents Introduction 1 Founding of Yale College 2 The Medical Community in Colonial Times 5 Yale School of Medicine (YSM) 6 Abraham Flexner 9 Dean Milton C. Winternitz, MD 11 Deans of the Yale School of Medicine 13 Rectors of the Collegiate School 13 Presidents of Yale College (after 1887, University) 14 World War II and Nitrogen Mustard 14 Yale’s Contributions to the War Effort 16 Financial Problems at the Medical School 17 Yale New-Haven Hospital (YNHH) 19 Other Hospitals 21 Beginning Interest in Cancer 23 The Cancer Committee 24 Members of the Cancer Committee in 2008 26 Department of Pharmacology 27 Chairs of the Department of Pharmacology 28 Arnold D.