Download Download
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

Skeletal Dysplasias
Skeletal Dysplasias North Carolina Ultrasound Society Keisha L.B. Reddick, MD Wilmington Maternal Fetal Medicine Development of the Skeleton • 6 weeks – vertebrae • 7 weeks – skull • 8 wk – clavicle and mandible – Hyaline cartilage • Ossification – 7-12 wk – diaphysis appears – 12-16 wk metacarpals and metatarsals – 20+ wk pubis, calus, calcaneus • Visualization of epiphyseal ossification centers Epidemiology • Overall 9.1 per 1000 • Lethal 1.1 per 10,000 – Thanatophoric 1/40,000 – Osteogenesis Imperfecta 0.18 /10,000 – Campomelic 0.1 /0,000 – Achondrogenesis 0.1 /10,000 • Non-lethal – Achondroplasia 15 in 10,000 Most Common Skeletal Dysplasia • Thantophoric dysplasia 29% • Achondroplasia 15% • Osteogenesis imperfecta 14% • Achondrogenesis 9% • Campomelic dysplasia 2% Definition/Terms • Rhizomelia – proximal segment • Mezomelia –intermediate segment • Acromelia – distal segment • Micromelia – all segments • Campomelia – bowing of long bones • Preaxial – radial/thumb or tibial side • Postaxial – ulnar/little finger or fibular Long Bone Segments Counseling • Serial ultrasound • Genetic counseling • Genetic testing – Amniocentesis • Postnatal – Delivery center – Radiographs Assessment • Which segment is affected • Assessment of distal extremities • Any curvatures, fracture or clubbing noted • Are metaphyseal changes present • Hypoplastic or absent bones • Assessment of the spinal canal • Assessment of thorax. Skeletal Dysplasia Lethal Non-lethal • Thanatophoric • Achondroplasia • OI type II • OI type I, III, IV • Achondrogenesis • Hypochondroplasia -

Current Overview of Osteogenesis Imperfecta
medicina Review Current Overview of Osteogenesis Imperfecta Mari Deguchi *, Shunichiro Tsuji , Daisuke Katsura , Kyoko Kasahara, Fuminori Kimura and Takashi Murakami Department of Obstetrics & Gynecology, Shiga University of Medical Science, Otsu 520-2192, Shiga, Japan; [email protected] (S.T.); [email protected] (D.K.); [email protected] (K.K.); [email protected] (F.K.); [email protected] (T.M.) * Correspondence: [email protected] Abstract: Osteogenesis imperfecta (OI), or brittle bone disease, is a heterogeneous disorder charac- terised by bone fragility, multiple fractures, bone deformity, and short stature. OI is a heterogeneous disorder primarily caused by mutations in the genes involved in the production of type 1 collagen. Severe OI is perinatally lethal, while mild OI can sometimes not be recognised until adulthood. Severe or lethal OI can usually be diagnosed using antenatal ultrasound and confirmed by various imaging modalities and genetic testing. The combination of imaging parameters obtained by ultrasound, computed tomography (CT), and magnetic resource imaging (MRI) can not only detect OI accurately but also predict lethality before birth. Moreover, genetic testing, either noninvasive or invasive, can further confirm the diagnosis prenatally. Early and precise diagnoses provide parents with more time to decide on reproductive options. The currently available postnatal treatments for OI are not curative, and individuals with severe OI suffer multiple fractures and bone deformities throughout their lives. In utero mesenchymal stem cell transplantation has been drawing attention as a promising therapy for severe OI, and a clinical trial to assess the safety and efficacy of cell therapy is currently ongoing. -

Ultrasonic Demonstration of Fetal Skeletal Dysplasia Case Reports
222 SAMJ VOLUME 67 9 FEBRUARY 1985 Ultrasonic demonstration of fetal skeletal dysplasia Case reports L1NNIE M. MULLER, B. J. CREMIN Toshiba linear array scanners (with 3,5 mHz transducers) and a Philips SDU 7000 Sector/Static scanner. A routine obstetric Summary scan does not involve complete examination of all limbs, but Reports on prenatal diagnosis in cases of skeletal when a bony abnormality is noted a skeletal survey is dysplasia have mostly been in high-risk mothers attempted. Real-time ultrasound offers a flexible technique, with a suspect genetic background where the fetal and when the infant is in the prone vertex position the linear lesion could probably be predetermined. We deal array has the advantage of a wider range of skeletal visualiza with routine ultrasonographic appraisal of the fetal tion. skeleton when dysplasia is not initially suspected, A complete skeletal survey consists of an evaluation of the and relate our experience of the lethal forms of this bones of the skull, spine, thorax and limbs and of correlating these other fetal structures. We first measured the biparietal condition. During the 4-year period 1981 - 1984,6 cases of skeletal dysplasia, including thanatophoric diameter (BPD) and then noted the echogenic characteristics dysplasia, achondrogenesis, the Ellis-van Creveld of the skull and facial contours. A comprehensive evaluation of syndrome (chondro-ectodermal dysplasia) and the spine is possible from 17 weeks' gestation onwards. In a osteogenesis imperfecta, were detected; the ultra longitudinal plane the posterior elements form segmented sonographic findings are discussed. bands of echoes that conform to the fetal kyphosis, but it is not always possible to visualize the whole spine. -

Prevalence and Incidence of Rare Diseases: Bibliographic Data
Number 1 | January 2019 Prevalence and incidence of rare diseases: Bibliographic data Prevalence, incidence or number of published cases listed by diseases (in alphabetical order) www.orpha.net www.orphadata.org If a range of national data is available, the average is Methodology calculated to estimate the worldwide or European prevalence or incidence. When a range of data sources is available, the most Orphanet carries out a systematic survey of literature in recent data source that meets a certain number of quality order to estimate the prevalence and incidence of rare criteria is favoured (registries, meta-analyses, diseases. This study aims to collect new data regarding population-based studies, large cohorts studies). point prevalence, birth prevalence and incidence, and to update already published data according to new For congenital diseases, the prevalence is estimated, so scientific studies or other available data. that: Prevalence = birth prevalence x (patient life This data is presented in the following reports published expectancy/general population life expectancy). biannually: When only incidence data is documented, the prevalence is estimated when possible, so that : • Prevalence, incidence or number of published cases listed by diseases (in alphabetical order); Prevalence = incidence x disease mean duration. • Diseases listed by decreasing prevalence, incidence When neither prevalence nor incidence data is available, or number of published cases; which is the case for very rare diseases, the number of cases or families documented in the medical literature is Data collection provided. A number of different sources are used : Limitations of the study • Registries (RARECARE, EUROCAT, etc) ; The prevalence and incidence data presented in this report are only estimations and cannot be considered to • National/international health institutes and agencies be absolutely correct. -

WES Gene Package Multiple Congenital Anomalie.Xlsx
Whole Exome Sequencing Gene package Multiple congenital anomalie, version 5, 1‐2‐2018 Technical information DNA was enriched using Agilent SureSelect Clinical Research Exome V2 capture and paired‐end sequenced on the Illumina platform (outsourced). The aim is to obtain 8.1 Giga base pairs per exome with a mapped fraction of 0.99. The average coverage of the exome is ~50x. Duplicate reads are excluded. Data are demultiplexed with bcl2fastq Conversion Software from Illumina. Reads are mapped to the genome using the BWA‐MEM algorithm (reference: http://bio‐bwa.sourceforge.net/). Variant detection is performed by the Genome Analysis Toolkit HaplotypeCaller (reference: http://www.broadinstitute.org/gatk/). The detected variants are filtered and annotated with Cartagenia software and classified with Alamut Visual. It is not excluded that pathogenic mutations are being missed using this technology. At this moment, there is not enough information about the sensitivity of this technique with respect to the detection of deletions and duplications of more than 5 nucleotides and of somatic mosaic mutations (all types of sequence changes). HGNC approved Phenotype description including OMIM phenotype ID(s) OMIM median depth % covered % covered % covered gene symbol gene ID >10x >20x >30x A4GALT [Blood group, P1Pk system, P(2) phenotype], 111400 607922 101 100 100 99 [Blood group, P1Pk system, p phenotype], 111400 NOR polyagglutination syndrome, 111400 AAAS Achalasia‐addisonianism‐alacrimia syndrome, 231550 605378 73 100 100 100 AAGAB Keratoderma, palmoplantar, -

Orphanet Report Series Rare Diseases Collection
Marche des Maladies Rares – Alliance Maladies Rares Orphanet Report Series Rare Diseases collection DecemberOctober 2013 2009 List of rare diseases and synonyms Listed in alphabetical order www.orpha.net 20102206 Rare diseases listed in alphabetical order ORPHA ORPHA ORPHA Disease name Disease name Disease name Number Number Number 289157 1-alpha-hydroxylase deficiency 309127 3-hydroxyacyl-CoA dehydrogenase 228384 5q14.3 microdeletion syndrome deficiency 293948 1p21.3 microdeletion syndrome 314655 5q31.3 microdeletion syndrome 939 3-hydroxyisobutyric aciduria 1606 1p36 deletion syndrome 228415 5q35 microduplication syndrome 2616 3M syndrome 250989 1q21.1 microdeletion syndrome 96125 6p subtelomeric deletion syndrome 2616 3-M syndrome 250994 1q21.1 microduplication syndrome 251046 6p22 microdeletion syndrome 293843 3MC syndrome 250999 1q41q42 microdeletion syndrome 96125 6p25 microdeletion syndrome 6 3-methylcrotonylglycinuria 250999 1q41-q42 microdeletion syndrome 99135 6-phosphogluconate dehydrogenase 67046 3-methylglutaconic aciduria type 1 deficiency 238769 1q44 microdeletion syndrome 111 3-methylglutaconic aciduria type 2 13 6-pyruvoyl-tetrahydropterin synthase 976 2,8 dihydroxyadenine urolithiasis deficiency 67047 3-methylglutaconic aciduria type 3 869 2A syndrome 75857 6q terminal deletion 67048 3-methylglutaconic aciduria type 4 79154 2-aminoadipic 2-oxoadipic aciduria 171829 6q16 deletion syndrome 66634 3-methylglutaconic aciduria type 5 19 2-hydroxyglutaric acidemia 251056 6q25 microdeletion syndrome 352328 3-methylglutaconic -

2 Achondrogenesis, Type IB A
Achondrogenesis,Type IB 579 2 Achondrogenesis,Type IB A Fraccaro type Extremities • Extremely short tubular bones, with squared, Severely shortened long bones with loss of longitudi- trapezoid, or stellate appearance nal orientation; unossified fibulas; deficient ossifica- • Wide and cupped ends of the long bones, with lat- tion of vertebral bodies, pelvis, and sacrum eral spurs • Unossified fibulas Frequency: 1 in 50,000 births. Skull • Ossified or only mildly underossified calvarium Genetics Autosomal recessive (OMIM 600972), caused by mutations in the DTDST gene at 5q32-q33 Bibliography Clinical Features Beluffi G. Achondrogenesis, type I. Rofo Fortschr Geb Rönt- • Fetal hydrops, polyhydramnios genstr Nuklearmed 1977; 127: 341–4 • Borochowitz Z, Lachman R, Adominan GE, Spear G, Jones K, Premature birth, stillbirth or death within min- Rimoin DL. Achondrogenesis type I: delineation of further utes in large proportion of cases heterogeneity and identification of two distinct subgroups. • Marked micromelic dwarfism J Pediatr 1988; 112: 23–31 • Normocephaly, but head appearing large because Jaeger HJ, Schmitz-Stolbrink A, Hulde J, Novak M, Roggen- of small body kamp K, Mathias K. The boneless neonate: a severe form of • achondrogenesis type I. Pediatr Radiol 1994; 24: 319–21 Severe midface hypoplasia Maroteaux P, Lamy M: Le diagnostic des nanismes chrondro- • Low nasal bridge dystrophiques chez les nouveau-nés. Arch Fr Pediatr 1968; • Micrognathia 25: 241–62 • Short neck Spranger JW, Langer LO, Wiedemann HR. Bone dysplasias. An • Short trunk, barrel-shaped chest atlas of constitutional disorders of skeletal development. • W.B. Saunders Company, Philadelphia, 1974, pp. 24–5 Overdistended abdomen Superti-Furga A, Hastbacka J, Wilcox WR, Cohn DH, van der • Edema of soft tissues Harten HJ, Rossi A, Blau N, Rimoin DL, Steinmann B, Lan- • Prenatal detection of micromelia by ultrasound der ES, Gitzelmann R. -
Psykisk Utviklingshemming Og Forsinket Utvikling
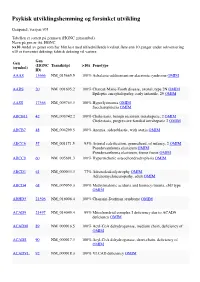
Psykisk utviklingshemming og forsinket utvikling Genpanel, versjon v03 Tabellen er sortert på gennavn (HGNC gensymbol) Navn på gen er iht. HGNC >x10 Andel av genet som har blitt lest med tilfredstillende kvalitet flere enn 10 ganger under sekvensering x10 er forventet dekning; faktisk dekning vil variere. Gen Gen (HGNC Transkript >10x Fenotype (symbol) ID) AAAS 13666 NM_015665.5 100% Achalasia-addisonianism-alacrimia syndrome OMIM AARS 20 NM_001605.2 100% Charcot-Marie-Tooth disease, axonal, type 2N OMIM Epileptic encephalopathy, early infantile, 29 OMIM AASS 17366 NM_005763.3 100% Hyperlysinemia OMIM Saccharopinuria OMIM ABCB11 42 NM_003742.2 100% Cholestasis, benign recurrent intrahepatic, 2 OMIM Cholestasis, progressive familial intrahepatic 2 OMIM ABCB7 48 NM_004299.5 100% Anemia, sideroblastic, with ataxia OMIM ABCC6 57 NM_001171.5 93% Arterial calcification, generalized, of infancy, 2 OMIM Pseudoxanthoma elasticum OMIM Pseudoxanthoma elasticum, forme fruste OMIM ABCC9 60 NM_005691.3 100% Hypertrichotic osteochondrodysplasia OMIM ABCD1 61 NM_000033.3 77% Adrenoleukodystrophy OMIM Adrenomyeloneuropathy, adult OMIM ABCD4 68 NM_005050.3 100% Methylmalonic aciduria and homocystinuria, cblJ type OMIM ABHD5 21396 NM_016006.4 100% Chanarin-Dorfman syndrome OMIM ACAD9 21497 NM_014049.4 99% Mitochondrial complex I deficiency due to ACAD9 deficiency OMIM ACADM 89 NM_000016.5 100% Acyl-CoA dehydrogenase, medium chain, deficiency of OMIM ACADS 90 NM_000017.3 100% Acyl-CoA dehydrogenase, short-chain, deficiency of OMIM ACADVL 92 NM_000018.3 100% VLCAD -

Osteogenesis Imperfecta: Recent Findings Shed New Light on This Once Well-Understood Condition Donald Basel, Bsc, Mbbch1, and Robert D
COLLABORATIVE REVIEW Genetics in Medicine Osteogenesis imperfecta: Recent findings shed new light on this once well-understood condition Donald Basel, BSc, MBBCh1, and Robert D. Steiner, MD2 TABLE OF CONTENTS Overview ...........................................................................................................375 Differential diagnosis...................................................................................380 Clinical manifestations ................................................................................376 In utero..........................................................................................................380 OI type I ....................................................................................................376 Infancy and childhood................................................................................380 OI type II ...................................................................................................377 Nonaccidental trauma (child abuse) ....................................................380 OI type III ..................................................................................................377 Infantile hypophosphatasia ....................................................................380 OI type IV..................................................................................................377 Bruck syndrome .......................................................................................380 Newly described types of OI .....................................................................377 -

Prenatal Diagnosis, Management and Outcomes of Skeletal Dysplasia
logy & Ob o st ec e tr n i Alouini et al., Gynecol Obstet (Sunnyvale) 2019, y c s G 9:4 Gynecology & Obstetrics ISSN: 2161-0932 Research Article Open Access Prenatal Diagnosis, Management and Outcomes of Skeletal Dysplasia Souhail Alouini1*, Jean Gabriel Martin1, Pascal Megier1 and Olga Esperandieu2 1Department of Obstetrics and Gynecology, Maternal-Foetal Medicine Unit Regional Hospital Center of Orleans, 45000, Orléans, France 2Department of Anatomie et Cytologie Pathologiques, Regional Hospital Center Of Orleans, 45000, Orléans, France *Corresponding author: Souhail Alouini, Department of Obstetrics and Gynecologic Surgery, Regional Hospital Center of Orleans, 14 Avenue de l’hospital, Orleans, 45100, France, Tel: +33688395759; E-mail: [email protected] Received date: March 02, 2019; Accepted date: May 02, 2019; Published date: May 09, 2019 Copyright: © 2019 Alouini S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Objective: To evaluate prenatal ultrasound findings of Skeletal Dysplasia (SD) and examine the contribution of radiological, histological and genetic exams. Methods: Retrospective study including all cases of SD managed in a tertiary maternity center between 1996 and 2010. Results: Eight cases of SD were diagnosed (1.4/10,000 births) by ultrasonography (USE). Three (38%) cases of SD were discovered in the first trimester, and five in the second trimester. We found short femurs in all cases. Anomalies consisted of the thickness of the femoral diaphysis, broad epiphysis, short and squat long bones, costal fractures, thinned coasts, anomalies of the profile and vertebrae, and a short and narrow thorax. -

Craniosynostosis Precision Panel Overview Indications Clinical Utility
Craniosynostosis Precision Panel Overview Craniosynostosis is defined as the premature fusion of one or more cranial sutures, often resulting in abnormal head shape. It is a developmental craniofacial anomaly resulting from a primary defect of ossification (primary craniosynostosis) or, more commonly, from a failure of brain growth (secondary craniosynostosis). As well, craniosynostosis can be simple when only one suture fuses prematurely or complex/compound when there is a premature fusion of multiple sutures. Complex craniosynostosis are usually associated with other body deformities. The main morbidity risk is the elevated intracranial pressure and subsequent brain damage. When left untreated, craniosynostosis can cause serious complications such as developmental delay, facial abnormality, sensory, respiratory and neurological dysfunction, eye anomalies and psychosocial disturbances. In approximately 85% of the cases, this disease is isolated and nonsyndromic. Syndromic craniosynostosis usually present with multiorgan complications. The Igenomix Craniosynostosis Precision Panel can be used to make a directed and accurate diagnosis ultimately leading to a better management and prognosis of the disease. It provides a comprehensive analysis of the genes involved in this disease using next-generation sequencing (NGS) to fully understand the spectrum of relevant genes involved. Indications The Igenomix Craniosynostosis Precision Panel is indicated for those patients with a clinical diagnosis or suspicion with or without the following manifestations: ‐ Microcephaly ‐ Scaphocephaly (elongated head) ‐ Anterior plagiocephaly ‐ Brachycephaly ‐ Torticollis ‐ Frontal bossing Clinical Utility The clinical utility of this panel is: - The genetic and molecular confirmation for an accurate clinical diagnosis of a symptomatic patient. - Early initiation of treatment in the form surgical procedures to relieve fused sutures, midface advancement, limited phase of orthodontic treatment and combined 1 orthodontics/orthognathic surgery treatment. -

Boomerang Dysplasia
Boomerang dysplasia Description Boomerang dysplasia is a disorder that affects the development of bones throughout the body. Affected individuals are born with inward- and upward-turning feet (clubfeet) and dislocations of the hips, knees, and elbows. Bones in the spine, rib cage, pelvis, and limbs may be underdeveloped or in some cases absent. As a result of the limb bone abnormalities, individuals with this condition have very short arms and legs. Pronounced bowing of the upper leg bones (femurs) gives them a "boomerang" shape. Some individuals with boomerang dysplasia have a sac-like protrusion of the brain ( encephalocele). They may also have an opening in the wall of the abdomen (an omphalocele) that allows the abdominal organs to protrude through the navel. Affected individuals typically have a distinctive nose that is broad with very small nostrils and an underdeveloped partition between the nostrils (septum). Individuals with boomerang dysplasia typically have an underdeveloped rib cage that affects the development and functioning of the lungs. As a result, affected individuals are usually stillborn or die shortly after birth from respiratory failure. Frequency Boomerang dysplasia is a rare disorder; its exact prevalence is unknown. Approximately 10 affected individuals have been identified. Causes Mutations in the FLNB gene cause boomerang dysplasia. The FLNB gene provides instructions for making a protein called filamin B. This protein helps build the network of protein filaments (cytoskeleton) that gives structure to cells and allows them to change shape and move. Filamin B attaches (binds) to another protein called actin and helps the actin to form the branching network of filaments that makes up the cytoskeleton.