Transperitoneal Laparoscopic Ureteroureterostomy with Excision of the Compressed Ureter for Retrocaval Ureter and Review of Literature
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ureterolysis.Pdf
Information about your procedure from The British Association of Urological Surgeons (BAUS) This leaflet contains evidence-based information about your proposed urological procedure. We have consulted specialist surgeons during its preparation, so that it represents best practice in UK urology. You should use it in addition to any advice already given to you. To view the online version of this leaflet, type the text below into your web browser: http://www.baus.org.uk/_userfiles/pages/files/Patients/Leaflets/Ureterolysis.pdf Key Points • Retroperitoneal fibrosis (RPF), also known as chronic periaortitis, forms at the back of your abdominal (tummy) cavity and can block your ureters (the tubes that carry urine from your kidneys to your bladder) • Ureterolysis is used to free your ureters from the blockage caused by the RPF • In most patients, the procedure involves open surgery through a long incision in your abdomen (tummy) but it can sometimes be done by laparoscopic (keyhole) surgery • To prevent further obstruction, we wrap your ureters in omentum (the fatty envelope inside your abdomen) or in a synthetic material • The procedure is usually reserved for patients in whom medical treatment has been unsuccessful • Care of patients with RPF is multi-disciplinary with physicians, expert surgeons and other specialists collaborating in your care What does this procedure involve? Freeing your ureters from scar tissue at the back of your abdomen to relieve the blockage and restore urine drainage from your kidneys. To prevent recurrence, we wrap your ureters in omentum (a sheet of fatty tissue found in your abdomen); if your omentum has been removed or is too small to use, we may wrap the ureters in a synthetic material. -

Robot-Assisted Laparoscopic Ureterolysis: Case Report and Literature Review of the Minimally Invasive Surgical Approach Ste´Fanie A
CASE REPORT Robot-Assisted Laparoscopic Ureterolysis: Case Report and Literature Review of the Minimally Invasive Surgical Approach Ste´fanie A. Seixas-Mikelus, MD, Susan J. Marshall, MD, D. Dawon Stephens, DO, Aaron Blumenfeld, MD, Eric D. Arnone, BA, Khurshid A. Guru, MD ABSTRACT INTRODUCTION Objectives: To evaluate our case of robot-assisted ureter- Ureteral obstruction secondary to extrinsic compression re- olysis (RU), describe our surgical technique, and review sults from both benign and malignant processes. Retroperi- the literature on minimally invasive ureterolysis. toneal fibrosis (RPF) and ureteral endometriosis (UE) are 2 uncommon conditions that cause ureteral obstruction.1–25 Methods: One patient managed with robot-assisted ure- terolysis for idiopathic retroperitoneal fibrosis was identi- First described in 1905 by Albarran and then by Ormond fied. The chart was analyzed for demographics, operative in 1948, RPF is a chronic inflammatory process character- parameters, and immediate postoperative outcome. The ized by deposition of dense fibrous tissue within the surgical technique was assessed and modified. Lastly, a retroperitoneum.26–28 Possible causes of RPF include med- review of the published literature on ureterolysis managed ications, infections, malignancy, inflammatory conditions, with minimally invasive surgery was performed. trauma, prior surgeries, and radiation therapy. About two- thirds of cases are considered idiopathic.10,25 Results: One patient underwent robot-assisted ureteroly- sis at our institution in 2 separate settings. Operative time Endometriosis, defined by the ectopic presence of endo- (OR) decreased from 279 minutes to 191 minutes. Esti- metrium, is another entity that can cause ureteral obstruc- mated blood loss (EBL) was less than 50mL. The patient tion. -

How I Do It Open Distal Ureteroureterostomy for Ectopic Ureters in Infants with Duplex Systems and No Vesicoureteral Reflux Under 6 Months of Age ______
SURGICAL TECHNIQUE Vol. 47 (3): 610-614, May - June, 2021 doi: 10.1590/S1677-5538.IBJU.2020.0742 How I do it open distal ureteroureterostomy for ectopic ureters in infants with duplex systems and no vesicoureteral reflux under 6 months of age _______________________________________________ Yuding Wang 1, Luis H. Braga 1 1 Departament of Surgery, McMaster University, Hamilton, Canada ABSTRACT ARTICLE INFO We describe a step by step technique for open distal ureteroureterostomy (UU) in infants Luis H. Braga less than 6 months presenting with duplex collecting system and upper pole ectopic https://orcid.org/0000-0002-3953-7353 ureter in the absence of vesicoureteral reflux (VUR). Keywords: Vesico-Ureteral Reflux; Ureter; Infant BACKGROUND Int Braz J Urol. 2021; 47: 610-4 Approximately 70% of ectopic ureters occur with ureteral duplication, with 80% of cases including contralateral duplication. They are found mainly _____________________ in Caucasian children and are four to seven times more common in females Submitted for publication: August 20, 2020 (1). The typical patient used to present with recurrent UTIs, flank pain from obstruction, or continuous incontinence (2). However, currently, the great ma- jority of these patients are discovered incidentally on routine investigation of _____________________ prenatal hydronephrosis (2). Accepted after revision: It has been common practice to defer surgical intervention of the September 10, 2020 patients diagnosed in the neonatal period until 12 months of age. Possi- ble management options include upper pole heminephrectomy, pyelou- reterostomy, common sheath ureteral reimplantation, upper pole ureteral _____________________ Published as Ahead of Print: clipping, and ipsilateral proximal or distal ureteroureterostomy. The deci- October 20, 2020 sion towards an ablative versus a reconstructive approach has traditionally been influenced by upper pole function, as well as surgeon preference. -

Contd... Supplementary Table 1: Contd
Supplementary Table1: Illustrates the main studies with ureteral endometriosis and their characteristics Author/year Journal Type of Number of Mean Ureteral Histological Management, n (%) study cases (n) age localization, n (%) type, n (%) Huang et al./2017 J Obstet RS 46 37.07 26 (56.5%) left, 22 (47.8%) 11 ureterolysis (23.9%), 28 (60.9%) Gynaecol Res 16 (34.8%) right, intrinsic, ureteroneocystostomy, 4 (8.7%) 4 (8.7%) bilateral 24 (52.2%) end‑to‑end ureteral anastomosis, extrinsic 3 (6.5%) nephrectomy Freire et al./2017 Urology RS 17 38 35.7% left, 14.3% 14.3% extrinsic, 7 distal ureterectomy, right, 10.7% bilateral 14.3% intrinsic 5 distal ureterectomy, and reimplantation (4 Lich‑Gregoir and 1 Lich‑Gregoir with psoas hitch), 3 ureteroureterostomy, 2 laparoscopic nephrectomy Kanno et al./2017 The Journal CR 1 25 100% right NR Laparoscopic segmental ureteral of Minimally resection and submucosal Invasive tunneling ureteroneocystostomy Gynecology with a psoas hitch and Boari flap Darwish et al./2017 J Minim RS 42 34.8 8 (19%) bilateral, 54.5% intrinsic 78% ureterolysis, 8% ureteral Invasive 17 (40.5%) right, resection followed by Gynecol 17 (40.5%) left end‑to‑end anastomosis, 14% ureteral resection and ureteroneocysostomy Alves et al./2017 J Minim RS 198 NR 7 (25%) left, 9 (32.1%) 76.9% intrinsic 100% ureterolysis, 6.06% Invasive right, 12 (42.9%) ureteral resection followed by Gynecol bilateral end‑to‑end anastomosis, 1 (0.5%) ureteroneocystostomy with Boari flap Abo et al./2016 Journal de RS 13 36 NR NR 11 (84.7%) advanced ureterolysis -

Urological Complications in Renal Transplantation
Henry Ford Hospital Medical Journal Manuscript 2015 Urological Complications in Renal Transplantation Riad N. Farah Richard Klugo Thomas Mertz Joseph C. Cerny Follow this and additional works at: https://scholarlycommons.henryford.com/hfhmedjournal Part of the Life Sciences Commons, Medical Specialties Commons, and the Public Health Commons Henry Ford Hosp Med Journal Vol 26, No 3, 1978 Urological Complications in Renal Transplantation Riad N. Farah, MD,* Richard Klugo, MD,* Thomas Mertz, MD,* and Joseph C. Cerny, MD' There were 116 renal transplants performed on 108 patients RAFT survival after renal transplantation depends upon over a five-year period at Henry Ford Hospital with three the vascular and urinary anastomosis as well as control of major urological complications. The rate of 2.6% compares graft rejection. Numerous factors contribute to good results favorably with that reported in other series. Careful pre in transplantation, among which are immediate function of operative urological evaluation together with technically the homograft, high degree of histocompatibility, the avoid precise ureteroneocystostomy are factors that minimize the ance of excessive immunosuppression, and minimal wound incidence of urological complications. and urological complications. There have been several reportsof urological complications following renal transplantation (See Table). Complication rates as high as 25.7%' have been reported with ureteropyelostomy, while the rates for ureteroneocystos tomy range from 15%^ to less than 1%.' In our review of 116 renal transplants we found three urological complications (2.6%). This rate compares favorably wfth that reported in earlier series and underscores the importance ofthe urolo gist in the work-up and management of the transplant recipient. -

Urology Privilege
SAN GORGONIO MEMORIAL HOSPITAL PRIVILEGE DELINEATION LIST UROLOGY NAME OF APPLICANT:____________________________________ DATE:________________ YEAR OF BOARD CERTIFICATION/RECERTIFICATION___________________________ PRIVILEGES QUALIFICATIONS/CRITERIA CATEGORY CATEGORY I USUAL AND CUSTOMARY PRIVILEGES (Procedures considered included in minimal formal training.) QUALIFICATIONS: 1. Successful completion of an accredited Urology residency training program, AND, 2. Board qualified/certified by the American Board of Urology with specific training and recent experience in privileges requested, OR, (in lieu of Board Certification) 3. Demonstrate comparable competency to perform the privileges requested based on proctoring reports, reference letters, activity/operative reports or other documentation acceptable to the Surgical Service, AND have been practicing in Urology for the past 5 years. 4. Privileges will be proctored per Surgical Service Rules and Regulations. MODERATE SEDATION I.V. MEDICATIONS FOR SPECIAL PROCEDURES (All medications with potential loss of protective reflexes regardless of route of administration) QUALIFICATIONS: Physicians with Urology privileges, by virtue of their specialty training are qualified for Moderate Sedation privileges as requested below, but must continue to demonstrate current competency as outlined in the Medical Staff Rules and Regulations. R # Done D P/O G CATEGORY 1 - USUAL AND CUSTOMARY PRIVELEGES 24 mos CORE PRIVILEGES: For the initial evaluation and management of patients of all ages for admission, work-up, pre and post-operative care, and ordering and prescribing medications per DEA certificate ENDOSCOPY: 1. Urethroscopy 2. Cystoscopy 3. Ureteroscopy 4. Nephroscopy RENAL: 5. Flank exploration, nephrectomy and/or partial 6. Removal of stones 7. Reconstruction 8. Trauma repair 9. Pyelotomy, Pyelolithotomy, Pyeloplasty 10. Retroperitoneal lymph node dissection 11. Nephroureterectomy 12. -

Summary of Services and Availability (By Location)
UPMC | University of Pittsburgh Medical Center For Reference Only UROLOGY 2013 Summary of Services and Availability (by location) Each location has sufficient space, equipment, staffing and financial resources in place or available in sufficient time as required to support each requested privilege. On an ongoing basis, the organization consistently determines the resources necessary for each requested privilege related to the facility's scope of service. Please review the following Summary of Services and Availability by Location prior to making your selections. If a facility is specifically identified below as NOT having a privilege/service available, you will NOT be considered for that privilege at that individual facility. Any request made that is identified as not available at an individual site will be considered Not Applicable for that site(s), and will be identified as such on your final approved Delineation of Privileges form. “x” means Privilege is Available at that location. “C” means contractual arrangement restricts granting this privilege. “N/A” means Privilege Not Available at that location. Facility Codes: UHOC= UPMC St. Margaret Harmar Outpatient Center Privilege UHOC Core privileges X Consultation Privileges N/A SURGERY OF THE KIDNEY, ADRENAL, URETER, AND BLADDER Biopsy, all techniques X Nephrotomy/pyelotomy/ureterotomy/ cystotomy for X stent placement, stone extraction, drainage abscess, biopsy, fulgeration, insertion of radioactive material Percutaneous nephroscopy, and other percutaneous X catheter techniques Nephrectomy, -
Laparoscopic Ureterolysis Without Omentoplasty in the Management of the Uropathy Secondary to Idiopathic Retroperitoneal Fibrosi
CASE REPORT Laparoscopic Ureterolysis without Omentoplasty in the Management of the Uropathy Secondary to Idiopathic Retroperitoneal Fibrosis Miguel A Bergero1, Patricio A Garcia Marchiñena2, Guillermo Gueglio3, Carlos David4, Fernando Dipatto5, Alberto Jurado6 ABSTRACT Introduction: Obstructive uropathy (OU) secondary to idiopathic retroperitoneal fibrosis (IRF) is an infrequent disease, and the standard treatment has not been established. However, ureterolysis with ureteral intraperitonealization is an effective therapeutic alternative. We present the successful management of OU secondary to an IRF by laparoscopic ureterolysis without omentoplasty (LUWO). Materials and methods: A retrospective descriptive study of 5 patients with IRF treated with LUWO was performed. Results: The average age was 60.4 years. The average creatinine was 3.86 mg/dL. There were no intraoperative or major postoperative complications. In a follow-up period of 31.2 months, all patients are asymptomatic, with an average creatinine level of 1.52 without dialysis requirement. No patients required corticosteroid therapy after surgery. Conclusion: Laparoscopic ureterolysis without omentoplasty is a safe and feasible option to treat the OU caused by IRF that provides good results in the medium-term follow-up, as we describe it in our series of cases. Keywords: Hydronephrosis, Laparoscopy, Retroperitoneal fibrosis, Ureteral obstruction. World Journal of Laparoscopic Surgery (2019): 10.5005/jp-journals-10033-1377 INTRODUCTION 1,4,5Department of Urology, Sanatorio Privado San Geronimo, Santa Fe, Obstructive uropathy (OU) related to idiopathic retroperitoneal Argentina fibrosis (IRF) is a rare disease characterized by retroperitoneal 2,3,6Department of Urology, Hospital Italiano de Buenos Aires, Buenos fibrosis. The pathology has theorized to be an inflammatory Aires, Argentina response to oxidized low-density lipoproteins.1,2 Because IRF has Corresponding Author: Miguel A Bergero, Department of Urology, 3–5 a very low prevalence, no treatments have been standardized. -

Surgical Site Infection Surveillance in Northern Ireland OPCS Code Lists
Surgical site infection surveillance (N. Ireland), codes for procedures and microorganism list November 4, 2014 Surgical Site Infection Surveillance in Northern Ireland OPCS code lists for relevant procedures and list of microorganisms Last updated 4 November 2014 1 | Public Health Agency (Northern Ireland) Surgical site infection surveillance (N. Ireland), codes for procedures and microorganism list November 4, 2014 This page is blank 2 | Public Health Agency (Northern Ireland) Surgical site infection surveillance (N. Ireland), codes for procedures and microorganism list November 4, 2014 Contents Section 1 – Surgical Site Infection Surveillance ......................................................................................................................................................................................................... 4 1.0 Contact Details ................................................................................................................................................................................................................................................. 4 1.1 Major procedure categories and description (detailed codes for each procedure category are listed in Section 2) ................................................................................... 5 Section 2 – OPCS procedure categories for surgical site infection surveillance ....................................................................................................................................................... 8 2.1.1 -

Ureteroneocystostomy Herniation Leading to Obstructive Uropathy 10 Years Postrenal Transplant: a Rare Case Report
[Downloaded free from http://www.urologyannals.com on Monday, January 25, 2021, IP: 158.232.3.16] Case Report Ureteroneocystostomy herniation leading to obstructive uropathy 10 years postrenal transplant: A rare case report Shailesh Chandra Sahay, Dilip Bhalla1, Pawan Kesarwani, Madan Sethi1 Departments of Urology and 1Nephrology, Max Superspeciality Hospital, Patparganj, Delhi, India Abstract Herniation of the urinary bladder is observed in around 1%–4% of cases. Bladder herniation rarely presents with obstructive uropathy; however, bladder herniation carrying ureteroneocystostomy and leading to obstructive uropathy of the graft is even rare. Here, we present a case of a 36-year-old male with deranged renal function test who had undergone renal transplant 10 years back. Computed tomography scan revealed bladder herniation with ureteroneocystostomy and hydronephrosis. He was surgically explored by Gibson incision and ureterolysis, and hernioplasty was performed. Although the cause of herniation was ureteroneocystostomy, it was managed immediately without any need for percutaneous nephrostomy. Keywords: Bladder hernia, transplant kidney, ureteroneocystostomy Address for correspondence: Dr. Shailesh Chandra Sahay, Room No 1029, Department of Urology, Max Superspeciality Hospital, Patparganj, Delhi, India. E‑mail: [email protected] Received: 04.01.2019, Accepted: 04.10.2019, Published: 07.11.2019. INTRODUCTION scan of the lower abdomen revealed hydroureter till its insertion in the bladder with an inguinal hernia and bladder Herniation of the urinary bladder is not rare; however, as its content [Figure 1b]. The urine culture was sterile, and around 1%–4% inguinal hernias may involve urinary the total leukocyte count was 8700 cells/µL. Cystoscopy bladder. Bladder herniation rarely presents with obstructive and exploratory laparotomy were planned. -

Obstruction of the Urinary Tract 2567
Chapter 540 ◆ Obstruction of the Urinary Tract 2567 Table 540-1 Types and Causes of Urinary Tract Obstruction LOCATION CAUSE Infundibula Congenital Calculi Inflammatory (tuberculosis) Traumatic Postsurgical Neoplastic Renal pelvis Congenital (infundibulopelvic stenosis) Inflammatory (tuberculosis) Calculi Neoplasia (Wilms tumor, neuroblastoma) Ureteropelvic junction Congenital stenosis Chapter 540 Calculi Neoplasia Inflammatory Obstruction of the Postsurgical Traumatic Ureter Congenital obstructive megaureter Urinary Tract Midureteral structure Jack S. Elder Ureteral ectopia Ureterocele Retrocaval ureter Ureteral fibroepithelial polyps Most childhood obstructive lesions are congenital, although urinary Ureteral valves tract obstruction can be caused by trauma, neoplasia, calculi, inflam- Calculi matory processes, or surgical procedures. Obstructive lesions occur at Postsurgical any level from the urethral meatus to the calyceal infundibula (Table Extrinsic compression 540-1). The pathophysiologic effects of obstruction depend on its level, Neoplasia (neuroblastoma, lymphoma, and other retroperitoneal or pelvic the extent of involvement, the child’s age at onset, and whether it is tumors) acute or chronic. Inflammatory (Crohn disease, chronic granulomatous disease) ETIOLOGY Hematoma, urinoma Ureteral obstruction occurring early in fetal life results in renal dys- Lymphocele plasia, ranging from multicystic kidney, which is associated with ure- Retroperitoneal fibrosis teral or pelvic atresia (see Fig. 537-2 in Chapter 537), to various -
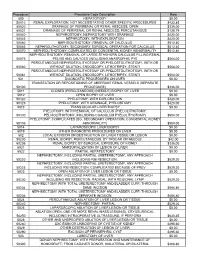
Procedure Procedure Code Description Rate 500
Procedure Procedure Code Description Rate 500 HEPATOTOMY $0.00 50010 RENAL EXPLORATION, NOT NECESSITATING OTHER SPECIFIC PROCEDURES $433.85 50020 DRAINAGE OF PERIRENAL OR RENAL ABSCESS; OPEN $336.00 50021 DRAINAGE OF PERIRENAL OR RENAL ABSCESS; PERCUTANIOUS $128.79 50040 NEPHROSTOMY, NEPHROTOMY WITH DRAINAGE $420.00 50045 NEPHROTOMY, WITH EXPLORATION $420.00 50060 NEPHROLITHOTOMY; REMOVAL OF CALCULUS $512.40 50065 NEPHROLITHOTOMY; SECONDARY SURGICAL OPERATION FOR CALCULUS $512.40 50070 NEPHROLITHOTOMY; COMPLICATED BY CONGENITAL KIDNEY ABNORMALITY $512.40 NEPHROLITHOTOMY; REMOVAL OF LARGE STAGHORN CALCULUS FILLING RENAL 50075 PELVIS AND CALYCES (INCLUDING ANATROPHIC PYE $504.00 PERCUTANEOUS NEPHROSTOLITHOTOMY OR PYELOSTOLITHOTOMY, WITH OR 50080 WITHOUT DILATION, ENDOSCOPY, LITHOTRIPSY, STENTI $504.00 PERCUTANEOUS NEPHROSTOLITHOTOMY OR PYELOSTOLITHOTOMY, WITH OR 50081 WITHOUT DILATION, ENDOSCOPY, LITHOTRIPSY, STENTI $504.00 501 DIAGNOSTIC PROCEDURES ON LIVER $0.00 TRANSECTION OR REPOSITIONING OF ABERRANT RENAL VESSELS (SEPARATE 50100 PROCEDURE) $336.00 5011 CLOSED (PERCUTANEOUS) (NEEDLE) BIOPSY OF LIVER $0.00 5012 OPEN BIOPSY OF LIVER $0.00 50120 PYELOTOMY; WITH EXPLORATION $420.00 50125 PYELOTOMY; WITH DRAINAGE, PYELOSTOMY $420.00 5013 TRANSJUGULAR LIVER BIOPSY $0.00 PYELOTOMY; WITH REMOVAL OF CALCULUS (PYELOLITHOTOMY, 50130 PELVIOLITHOTOMY, INCLUDING COAGULUM PYELOLITHOTOMY) $504.00 PYELOTOMY; COMPLICATED (EG, SECONDARY OPERATION, CONGENITAL KIDNEY 50135 ABNORMALITY) $504.00 5014 LAPAROSCOPIC LIVER BIOPSY $0.00 5019 OTHER DIAGNOSTIC PROCEDURES