Endemicity of Lymphatic Filariasis in Three Local Government Areas in Imo State, Nigeria
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

Citizens Wealth Platform 2017
2017 FEDERAL CAPITAL BUDGET PULLOUT Of the States in the SOUTH-EAST Geo-Political Zone C P W Citizens Wealth Platform Citizen Wealth Platform (CWP) (Public Resources Are Made To Work And Be Of Benefit To All) 2017 FEDERAL CAPITAL BUDGET of the States in the SOUTH EAST Geo-Political Zone Compiled by VICTOR EMEJUIWE For Citizens Wealth Platform (CWP) (Public Resources Are Made To Work And Be Of Benefit To All) 2017 SOUTH EAST FEDERAL CAPITAL BUDGET PULLOUT Page 2 First Published in August 2017 By Citizens Wealth Platform C/o Centre for Social Justice 17 Yaounde Street, Wuse Zone 6, Abuja Email: [email protected] Website: www.csj-ng.org Tel: 08055070909. Blog: csj-blog.org. Twitter:@censoj. Facebook: Centre for Social Justice, Nigeria 2017 SOUTH EAST FEDERAL CAPITAL BUDGET PULLOUT Page 3 Table of Contents Foreword 5 Abia State 6 Anambra State 26 Embonyi State 46 Enugu State 60 Imo State 82 2017 SOUTH EAST FEDERAL CAPITAL BUDGET PULLOUT Page 4 Foreword In the spirit of the mandate of the Citizens Wealth Platform to ensure that public resources are made to work and be of benefit to all, we present the South East Capital Budget Pullout for the financial year 2017. This has been our tradition in the last six years to provide capital budget information to all Nigerians. The pullout provides information on federal Ministries, Departments and Agencies, names of projects, amount allocated and their location. The Economic Recovery and Growth Plan (ERGP) is the Federal Government’s blueprint for the resuscitation of the economy and its revival from recession. -

River Basins of Imo State for Sustainable Water Resources
nvironm E en l & ta i l iv E C n g Okoro et al., J Civil Environ Eng 2014, 4:1 f o i n l Journal of Civil & Environmental e a e n r r i DOI: 10.4172/2165-784X.1000134 n u g o J ISSN: 2165-784X Engineering Review Article Open Access River Basins of Imo State for Sustainable Water Resources Management BC Okoro1*, RA Uzoukwu2 and NM Chimezie2 1Department of Civil Engineering, Federal University of Technology, Owerri, Imo State, Nigeria 2Department of Civil Engineering Technology, Federal Polytechnic Nekede, Owerri, Imo State, Nigeria Abstract The river basins of Imo state, Nigeria are presented as a natural vital resource for sustainable water resources management in the area. The study identified most of all the known rivers in Imo State and provided information like relief, topography and other geographical features of the major rivers which are crucial to aid water management for a sustainable water infrastructure in the communities of the watershed. The rivers and lakes are classified into five watersheds (river basins) such as Okigwe watershed, Mbaise / Mbano watershed, Orlu watershed, Oguta watershed and finally, Owerri watershed. The knowledge of the river basins in Imo State will help analyze the problems involved in water resources allocation and to provide guidance for the planning and management of water resources in the state for sustainable development. Keywords: Rivers; Basins/Watersheds; Water allocation; • What minimum reservoir capacity will be sufficient to assure Sustainability adequate water for irrigation or municipal water supply, during droughts? Introduction • How much quantity of water will become available at a reservoir An understanding of the hydrology of a region or state is paramount site, and when will it become available? In other words, what in the development of such region (state). -

Statistical Prediction of Gully Erosion Development on the Coastal Plain Sands of the South Eastern Nigeria
Nigerian Journal of Technology, Vol. 24, No. 2, September 2005 Nwakwasi and Tee 59 STATISTICAL PREDICTION OF GULLY EROSION DEVELOPMENT ON THE COASTAL PLAIN SANDS OF THE SOUTH EASTERN NIGERIA NWAKWASI, N.L., and TEE, D.P. Department of Civil Engineering, Federal University of Technology, Owerri, Nigeria ABSTRACT A statistical model for predicting gully initiation was developed using variables from 20 randomly selected sites. The random samples gave 10 gully sites and 10 non-gully sites. In all, 12 variables were identified but using students t-tests approach, only four variables contributed to gully development. These four variables include Maximum slope, Maximum slope length, Microrelief amplitude and percentage coarse sand. The four variables were combined through factor analysis and statistical manipulations to form Linear Discriminant Function (LDF). Three functions were obtained by combining the variables in three different ways. An application of the three functions to the field situation identified function 1,1 as a very comfortable prediction. When Yl was used to classify the various sites using the variables obtained from the field, a 25% wrong classification was obtained. This value was quite low when compared with the other two functions whose wrong classification ranged from 35% and above. It was observed from the study that when Yl is less than 30, it indicated little or no gully erosion threat. INTRODUCTION spatial distribution of rainfall as induced gully Today, in our country Nigeria, erosion menace formation in most of our towns and express the has become all object of discussion and a major need to adopt good planning and policy ecological problem facing the nation. -

Aquifer Transmissivity from Surface Geo- Electrical Data: a Case Study of Owerri and Environs, South-Eastern Nigeria
See discussions, stats, and author profiles for this publication at: http://www.researchgate.net/publication/240613398 Aquifer Transmissivity from surface geo- electrical data: A case study of Owerri and Environs, South-eastern Nigeria ARTICLE in JOURNAL OF THE GEOLOGICAL SOCIETY OF INDIA · JUNE 2012 Impact Factor: 0.6 · DOI: 10.1007/s12594-012-0126-8 CITATIONS READS 3 52 2 AUTHORS: Amobi Ekwe ALEX IHEANYICHUKWU Opara Federal University Ndufu Alike Ikwo Federal University of Technology Owerri 17 PUBLICATIONS 50 CITATIONS 44 PUBLICATIONS 14 CITATIONS SEE PROFILE SEE PROFILE Available from: Amobi Ekwe Retrieved on: 23 December 2015 JOURNAL GEOLOGICAL SOCIETY OF INDIA Vol.80, July 2012, pp.123-128 Aquifer Transmissivity from Surface Geo-electrical Data: A Case Study of Owerri and Environs, Southeastern Nigeria 1 2 A. C. EKWE and A. I. OPARA 1Department of Geology, University of Nigeria, Nsukka 2Department of Geosciences, Federal University of Technology, Owerri, Imo State Email: [email protected]; [email protected], [email protected] Abstract: The combination of layer resistivity and thickness in the so called Da-zarrouk parameters S (longitudinal conductance) and R (transverse resistance) have proved useful in the evaluation of the transmissivities of the aquifers around Owerri and environs. The area is underlain by the unconsolidated to semi-consolidated coastal Benin Formation. The surface direct current electrical resistivity method was used in the study. Seven Vertical Electrical Soundings (VES) data by the Schlumberger array was acquired in the area. A maximum current electrode spacing (AB) of 1000 m was used for data acquisition. Four of the soundings were carried out near existing boreholes. -

The Relationship Between Placement of Female Teachers and Academic Performnace of Secondary School Students in Owerri Urban of Imo State
Journal of Literature, Languages and Linguistics - An Open Access International Journal Vol.2 2013 The Relationship between Placement of Female Teachers and Academic Performnace of Secondary School Students in Owerri Urban of Imo State Lazarus I. okoroji* Julius O. Anyanwu. School of Management, Federal University o Technology, PMB 1526, Owerri. Imo State, Nigeria. * E-mail of the corresponding author: [email protected] Abstract This research focused on the relationship between placement of Women Teachers and Academic Performance of Secondary School Students in Owerri Urban of Imo State. Descriptive research design was adopted in carrying out the study. A random sampling technique was used to select ten (10) secondary schools used in the study out of twenty secondary schools in Owerri Urban of Imo state. Questionnaire was developed to collect primary data. The data collected was analyzed using the simple percentage method. It ascertained whether there are more female teachers in the Owerri Urban Secondary Schools than their male counterparts thereby assessing the role of women teachers to the education of the students, vis-à-vis their academic performance. In pursuance of the objectives, some hypotheses were stated as seen in chapter 1. A total of twelve schools (12) were sampled with twenty five (25) principals and vice principals, some classroom teachers and officials of the Secondary Education Management Board Owerri Zone as respondents. Data was collected through the use of questionnaires, oral interviews and personal observations respectively. From the findings as reflected in chapter five (5), it was concluded that although many variables are contributory to the excellent and poor performance of students, the posting of many women teachers in a School lowers teachers/school productivity and consequently affects adversely the student’s academic performance. -

Godwin Valentine O= University of Nigeria, Nsukka
EZE, CAROLINE NGOZI PG/Ph.D/10/57530 MOTIVATIONAL INITIATIVES FOR CITIZENS’ PARTICIPATION IN COMMUNITY DEVELOPMENT ACTIVITIES IN ANAMBRA AND IMO STATES OF NIGERIA FACULTY OF EDUCATION DEPARTMENT OF ADULT EDUCATION AND EXTRA MURAL STUDIES Digitally Signed by: Content manager’s Name DN : CN = Webmaster’s name Godwin Valentine O= University of Nigeria, Nsukka OU = Innovation Centre ii MOTIVATIONAL INITIATIVES FOR CITIZENS’ PARTICIPATION IN COMMUNITY DEVELOPMENT ACTIVITIES IN ANAMBRA AND IMO STATES OF NIGERIA By EZE, CAROLINE NGOZI PG/Ph.D/10/57530 DEPARTMENT OF ADULT EDUCATION AND EXTRA MURAL STUDIES FACULTY OF EDUCATION UNIVERSITY OF NIGERIA NSUKKA JULY, 2016 i TITLE PAGE MOTIVATIONAL INITIATIVES FOR CITIZENS’ PARTICIPATION IN COMMUNITY DEVELOPMENT ACTIVITIES IN ANAMBRA AND IMO STATES OF NIGERIA By EZE, CAROLINE NGOZI PG/Ph.D/10/57530 A THESIS SUBMITTED TO THE FACULTY OF EDUCATION, UNIVERSITY OF NIGERIA, NSUKKA IN PARTIAL FULFILLMENT FOR THE AWARD OF THE DEGREE OF DOCTOR OF PHILOSOPHY (Ph.D) IN ADULT EDUCATION/COMMUNITY DEVELOPMENT SUPERVISOR: PROF. (MRS.) C.I. OREH JULY, 2016 ii APPROVAL PAGE This thesis has been approved for the Department of Adult Education and Extral Mural Studies, University of Nigeria, Nsukka. By ……………………………… …………………………… Prof. (Mrs) C.I. Oreh Thesis Supervisor Internal Examiner ……………………….. ……………………………. External Examiner Prof. S.C. Nwizu Head of Department …………………………………… Prof. Uju Umo Dean, Faculty of Education iii CERTIFICATION Eze, Caroline Ngozi a Postgraduate Student in the Department of Adult Education and Extral Mural Studies, with registration Number PG/Ph.D/10/57530, has satisfactorily completed the requirements for research work for the degree of Doctor of Philosophy in Adult Education/Community Development. -

The Land Has Changed: History, Society and Gender in Colonial Eastern Nigeria
University of Calgary PRISM: University of Calgary's Digital Repository University of Calgary Press University of Calgary Press Open Access Books 2010 The land has changed: history, society and gender in colonial Eastern Nigeria Korieh, Chima J. University of Calgary Press Chima J. Korieh. "The land has changed: history, society and gender in colonial Eastern Nigeria". Series: Africa, missing voices series 6, University of Calgary Press, Calgary, Alberta, 2010. http://hdl.handle.net/1880/48254 book http://creativecommons.org/licenses/by-nc-nd/3.0/ Attribution Non-Commercial No Derivatives 3.0 Unported Downloaded from PRISM: https://prism.ucalgary.ca University of Calgary Press www.uofcpress.com THE LAND HAS CHANGED History, Society and Gender in Colonial Eastern Nigeria Chima J. Korieh ISBN 978-1-55238-545-6 THIS BOOK IS AN OPEN ACCESS E-BOOK. It is an electronic version of a book that can be purchased in physical form through any bookseller or on-line retailer, or from our distributors. Please support this open access publication by requesting that your university purchase a print copy of this book, or by purchasing a copy yourself. If you have any questions, please contact us at [email protected] Cover Art: The artwork on the cover of this book is not open access and falls under traditional copyright provisions; it cannot be reproduced in any way without written permission of the artists and their agents. The cover can be displayed as a complete cover image for the purposes of publicizing this work, but the artwork cannot be extracted from the context of the cover of this specific work without breaching the artist’s copyright. -

Effects of Soil Erosion and Sediment Deposition on Surface Water Quality: a Case Study of Otamiri River
Asian Journal of Engineering and Technology (ISSN: 2321 – 2462) Volume 02 – Issue 05, October 2014 Effects of Soil Erosion and Sediment Deposition on Surface Water Quality: A Case Study of Otamiri River J. C. Osuagwu, A. N. Nwachukwu, H. U. Nwoke, K. C. Agbo Department of Civil Engineering, Federal University of Technology, Owerri, Nigeria _____________________________________________________________________________________________ ABSTRACT---- Soil erosion involves detachment soil particles and transportation by run-off with subsequent deposition of the sediments in river courses and land depressions. The otamiri river is one of the main rivers in Imo state, Nigeria and the source for Owerri water scheme. The river runs from Egbu in Owerri, Imo state to Ozuzu in Etche, Rivers State from where it flows to the Atlantic Ocean. It is a major receiver of sediments from numerous gullies in the watershed. The objective of study was to analyse the nature and extent of the effects of the sediments inflow on the major quality parameters of the river with a view to making recommendations on sustainable preservation of the river. Water samples were collected during runoff inflows at two different locations (A and B) simultaneously for physical and biochemical tests. Location A was near the source at Egbu while B is a location downstream near discharge point of a major gully. The results showed marked fluctuation in quality between samples from location A and B. Measured values of Ph, hardness, Iron, chloride, BOD, TSS and TDS indicated 30.8%, 88.9%, 50%, 60% , 176%, 94.5% and 84.4% differences respectively. The value of pollution index computed for sample B is 2.43 while that of Sample A is 1.22. -
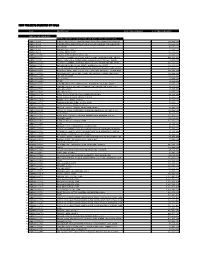
New Projects Inserted by Nass
NEW PROJECTS INSERTED BY NASS CODE MDA/PROJECT 2018 Proposed Budget 2018 Approved Budget FEDERAL MINISTRY OF AGRICULTURE AND RURAL SUPPLYFEDERAL AND MINISTRY INSTALLATION OF AGRICULTURE OF LIGHT AND UP COMMUNITYRURAL DEVELOPMENT (ALL-IN- ONE) HQTRS SOLAR 1 ERGP4145301 STREET LIGHTS WITH LITHIUM BATTERY 3000/5000 LUMENS WITH PIR FOR 0 100,000,000 2 ERGP4145302 PROVISIONCONSTRUCTION OF SOLAR AND INSTALLATION POWERED BOREHOLES OF SOLAR IN BORHEOLEOYO EAST HOSPITALFOR KOGI STATEROAD, 0 100,000,000 3 ERGP4145303 OYOCONSTRUCTION STATE OF 1.3KM ROAD, TOYIN SURVEYO B/SHOP, GBONGUDU, AKOBO 0 50,000,000 4 ERGP4145304 IBADAN,CONSTRUCTION OYO STATE OF BAGUDU WAZIRI ROAD (1.5KM) AND EFU MADAMI ROAD 0 50,000,000 5 ERGP4145305 CONSTRUCTION(1.7KM), NIGER STATEAND PROVISION OF BOREHOLES IN IDEATO NORTH/SOUTH 0 100,000,000 6 ERGP445000690 SUPPLYFEDERAL AND CONSTITUENCY, INSTALLATION IMO OF STATE SOLAR STREET LIGHTS IN NNEWI SOUTH LGA 0 30,000,000 7 ERGP445000691 TOPROVISION THE FOLLOWING OF SOLAR LOCATIONS: STREET LIGHTS ODIKPI IN GARKUWARI,(100M), AMAKOM SABON (100M), GARIN OKOFIAKANURI 0 400,000,000 8 ERGP21500101 SUPPLYNGURU, YOBEAND INSTALLATION STATE (UNDER OF RURAL SOLAR ACCESS STREET MOBILITY LIGHTS INPROJECT NNEWI (RAMP)SOUTH LGA 0 30,000,000 9 ERGP445000692 TOSUPPLY THE FOLLOWINGAND INSTALLATION LOCATIONS: OF SOLAR AKABO STREET (100M), LIGHTS UHUEBE IN AKOWAVILLAGE, (100M) UTUH 0 500,000,000 10 ERGP445000693 ANDEROSION ARONDIZUOGU CONTROL IN(100M), AMOSO IDEATO - NCHARA NORTH ROAD, LGA, ETITI IMO EDDA, STATE AKIPO SOUTH LGA 0 200,000,000 11 ERGP445000694 -

ZONAL INTERVENTION PROJECTS Federal Goverment of Nigeria APPROPRIATION ACT
2014 APPROPRIATION ACT ZONAL INTERVENTION PROJECTS Federal Goverment of Nigeria APPROPRIATION ACT Federal Government of Nigeria 2014 APPROPRIATION ACT S/NO PROJECT TITLE AMOUNT AGENCY =N= 1 CONSTRUCTION OF ZING-YAKOKO-MONKIN ROAD, TARABA STATE 300,000,000 WORKS 2 CONSTRUCTION OF AJELE ROAD, ESAN SOUTH EAST LGA, EDO CENTRAL SENATORIAL 80,000,000 WORKS DISTRICT, EDO STATE 3 YOUTH DEVELOPMENT CENTRE, OTADA, OTUKPO, BENUE STATE (ONGOING) 150,000,000 YOUTH 4 YOUTH DEVELOPMENT CENTRE, OBI, BENUE STATE (ONGOING) 110,000,000 YOUTH 5 YOUTH DEVELOPMENT CENTRE, AGATU, BENUE STATE (ONGOING) 110,000,000 YOUTH 6 YOUTH DEVELOPMENT CENTRE-MPU,ANINRI LGA ENUGU STATE 70,000,000 YOUTH 7 YOUTH DEVELOPMENT CENTRE-AWGU, ENUGU STATE 150,000,000 YOUTH 8 YOUTH DEVELOPMENT CENTRE-ACHI,OJI RIVER ENUGU STATE 70,000,000 YOUTH 9 YOUTH DEVELOPMENT CENTRE-NGWO UDI LGA ENUGU STATE 100,000,000 YOUTH 10 YOUTH DEVELOPMENT CENTRE- IWOLLO, EZEAGU LGA, ENUGU STATE 100,000,000 YOUTH 11 YOUTH EMPOWERMENT PROGRAMME IN LAGOS WEST SENATORIAL DISTRICT, LAGOS STATE 250,000,000 YOUTH 12 COMPLETION OF YOUTH DEVELOPMENT CENTRE AT BADAGRY LGA, LAGOS 200,000,000 YOUTH 13 YOUTH DEVELOPMENT CENTRE IN IKOM, CROSS RIVER CENTRAL SENATORIAL DISTRICT, CROSS 34,000,000 YOUTH RIVER STATE (ON-GOING) 14 ELECTRIFICATION OF ALIFETI-OBA-IGA OLOGBECHE IN APA LGA, BENUE 25,000,000 REA 15 ELECTRIFICATION OF OJAGBAMA ADOKA, OTUKPO LGA, BENUE (NEW) 25,000,000 REA 16 POWER IMPROVEMENT AND PROCUREMENT AND INSTALLATION OF TRANSFORMERS IN 280,000,000 POWER OTUKPO LGA (NEW) 17 ELECTRIFICATION OF ZING—YAKOKO—MONKIN (ON-GOING) 100,000,000 POWER ADD100M 18 SUPPLY OF 10 NOS. -

FUTO Supplementary Admission List - Uploaded On
FUTO Supplementary Admission List - Uploaded on www.myschoolgist.com.ng FUTO 2016/2017 FIRST SUPPLEMENTARY ADMISSIONS LIST State of S/No Cand. Name LGA JAMB Score Course Name Origin 1 UCHE FAVOUR EKENE-BEULAH ABIA UMUA N 280 AGRICULTURAL ECONOMICS 2 OBIYOR RITA ULOMA IMO AHI-M 223 AGRICULTURAL ECONOMICS 3 MGBOKWERE UGOCHUKWU HENRY IMO ORU E 249 AGRICULTURAL ECONOMICS 4 OHAERI CHIDERA THEIMA IMO EZINIH 210 AGRICULTURAL ECONOMICS 5 IGBOANUSI LILIAN CHINWENDU IMO NWANG 236 AGRICULTURAL ECONOMICS 6 ABANUKAM CHIGEMEZU FELICITAS IMO ORU E 237 AGRICULTURAL ECONOMICS 7 ODIDIKA CHINONYEREM JUDITH IMO ORSU 217 AGRICULTURAL ECONOMICS 8 AZORH MMADUABUCHI DAVID IMO NGOR O 261 AGRICULTURAL ECONOMICS 9 OKORO BLESSING C IMO ORU E 244 AGRICULTURAL ECONOMICS 10 TIMOTHY-AGUGUA CHIDINMA FAITH IMO NKWER 237 AGRICULTURAL ECONOMICS 11 EZEAGU MARIA-ASSUMPTA C IMO IDE N 218 AGRICULTURAL ECONOMICS 12 IWUOHA CHIDINMA GLORY IMO ISI M 229 AGRICULTURAL ECONOMICS 13 ONYENWE RUTH CHINECHEREM IMO NGOR OK 223 AGRICULTURAL ECONOMICS 14 OZOEMENA UZOCHUKWU DONALD IMO ORU W 282 AGRICULTURAL ECONOMICS 15 OGBONNA EBUKA GOODNEWS IMO MBAIT 210 AGRICULTURAL ECONOMICS 16 OGBODO CHIDUBEM DUKE ENUGU NKAN-W 217 AGRICULTURAL ECONOMICS 17 EMETO VICTORY CHINWENDU IMO ISI M 226 AGRICULTURAL ECONOMICS 18 EZENWA KELVIN AZUBUIKE ANA IDEMILI SOUTH 203 AGRICULTURAL ECONOMICS 19 OKPALA ONYINYE EMMANUELLA ANA AGUATA 200 AGRICULTURAL ECONOMICS 20 MGBEMELE IFEANYI FRANKLYN IMO OKIGW 217 AGRICULTURAL ECONOMICS 21 Ekeh Onyinyechi Juliet Imo Ahiazu-Mbaise 196 AGRICULTURAL ECONOMICS 22 OGUJIUBA UKACHI -

Democracy and OSU Caste Conflict Transformation in Eastern Nigeria: a Cultural Perspective
International Journal of History and Cultural Studies (IJHCS) Volume2, Issue 1, 2016, PP 1-16 ISSN 2454-7646 (Print) & ISSN 2454-7654 (Online) www.arcjournals.org Democracy and OSU Caste Conflict Transformation in Eastern Nigeria: A Cultural Perspective Luke A Amadi, Edmund F Obomanu Department of Political Science & Administrative Studies University of Port Harcourt, Nigeria Abstract: This paper argues that the material conditions of caste relationship among the Igbo of Eastern Nigeria are more integrally linked to institutionalized cultural practices building on the critical implications of stigmatization, discrimination and conflict on the basis of social status. Osu caste system is an old long cultural practice of discrimination in which the Osu who are dedicated to the gods as living sacrifices are socially discriminated by the Nwadiala who are free born. Through the articulation of a resultant conflict theoretical framework, the paper provides a critique of contemporary Osu caste practice in the era of nascent democracy in Nigeria. The study draws from recent and incendiary case analysis and argues that democracy seem to conceal rather than transform Osu caste practice as its founding ideals of equality, freedom, public opinion is limited or at variance with cast cultural practices which persists among the freeborn called Nwadiala and the out castes called Osu. The paper suggests that as an organizing principle for good governance democracy should assume a novel cause to reopen caste discrimination for policy reconsideration Keywords: Democracy Culture, Osu Caste System, Conflict, Development, Igbo 1. INTRODUCTION In recent decades cultural studies have not made an enormous contribution to the study of periphery societies and institutions.