(IUD) for Emergency Contraception
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ocps) Used in the NM Family Planning Program (FPP
The following slides are intended to familiarize nurses and clinicians with oral contraceptive pills (OCPs) used in the NM Family Planning Program (FPP). The FPP does not intend for this information to supersede the Family Planning Protocol particularly on the requirement for Public Health Nurses in the Public Health Offices to consult a clinician as stated in the Protocol when in doubt or if it is necessary to switch the client’s OCP type. 1 2 Combined oral contraceptives (COCs) contain two hormones; estrogen and progestin. In general, any combined OCP is good for most women who are eligible to take estrogen according to the CDC U.S. Medical Eligibility Criteria (MEC). Once again, refer to the US MEC chart to find out if OCP is a suitable choice for clients with specific health conditions. To learn a little bit about what each hormone does, the FPP is providing the following summary: Estrogen: provides endometrial stability = menstrual cycle control. A higher estrogen dose increases the venous thromboembolism (VTE) or clot risk but OCP clot risk is still less harmful than the clot risk related to pregnancy and giving birth. Progestin: provides most of the contraceptive effect by ‐Preventing luteinizing hormone (LH) surge /ovulation ‐Thickening the cervical mucus to prevent sperm entry. Two major OCP formations are available. Monophasic: There is only one dose of estrogen and progestin in each active pill in the packet; and Multiphasic: There are varying doses of hormones, particularly progestin in the active pills. 3 Section 3 of the FPP Protocol contains the OCP Substitute Table, which groups OCPs into 6 classes according to the estrogen dosage, the type of progestin and the formulations. -

Contraception: Choosing the Right Method for You
Contraception: Choosing the Right Method for You Megan Sax, MD and James L. Whiteside, MD What’s available? Choosing a method of contraception can be overwhelming. The most commonly used methods of reversible contraception in the United States are: hormonal methods the intrauterine device (IUD) the implant barrier methods (e.g. male condom)1 Friends, family, and the Internet are full of stories of failed contraception or bad reactions and these stories can have a big influence that doesn’t always line up with the facts.2 However, knowing these facts is critical to figuring out what type will work best for you. Highly Effective Contraception The best place to start in choosing your contraception is to determine when, if ever, you are planning on starting a family. If you do not wish to become pregnant in the next year, a Long-Acting Reversible Contraceptive (LARC) device may be a good option. LARCs include an implant placed under the skin of the upper, inner arm (brand name Nexplanon) and the IUD. IUDs are placed inside the uterus (see Figure 1). They use copper (brand name ParaGard) or hormones (brand names: Mirena, Lilleta, Skyla, Kyleena) to stop a pregnancy from happening. LARCs are the most effective reversible form of contraception. Less than 1% of users experience unintended pregnancy during the first year of use.3 Currently, the implant Nexplanon is effective for 3 years. The hormonal IUD may be used for 3 to 5 years, depending on the brand. The copper IUD works for 10 years. These devices are inserted and removed by a medical care provider. -

Comparing the Effects of Combined Oral Contraceptives Containing Progestins with Low Androgenic and Antiandrogenic Activities on the Hypothalamic-Pituitary-Gonadal Axis In
JMIR RESEARCH PROTOCOLS Amiri et al Review Comparing the Effects of Combined Oral Contraceptives Containing Progestins With Low Androgenic and Antiandrogenic Activities on the Hypothalamic-Pituitary-Gonadal Axis in Patients With Polycystic Ovary Syndrome: Systematic Review and Meta-Analysis Mina Amiri1,2, PhD, Postdoc; Fahimeh Ramezani Tehrani2, MD; Fatemeh Nahidi3, PhD; Ali Kabir4, MD, MPH, PhD; Fereidoun Azizi5, MD 1Students Research Committee, School of Nursing and Midwifery, Department of Midwifery and Reproductive Health, Shahid Beheshti University of Medical Sciences, Tehran, Islamic Republic Of Iran 2Reproductive Endocrinology Research Center, Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Islamic Republic Of Iran 3School of Nursing and Midwifery, Department of Midwifery and Reproductive Health, Shahid Beheshti University of Medical Sciences, Tehran, Islamic Republic Of Iran 4Minimally Invasive Surgery Research Center, Iran University of Medical Sciences, Tehran, Islamic Republic Of Iran 5Endocrine Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Islamic Republic Of Iran Corresponding Author: Fahimeh Ramezani Tehrani, MD Reproductive Endocrinology Research Center Research Institute for Endocrine Sciences Shahid Beheshti University of Medical Sciences 24 Parvaneh Yaman Street, Velenjak, PO Box 19395-4763 Tehran, 1985717413 Islamic Republic Of Iran Phone: 98 21 22432500 Email: [email protected] Abstract Background: Different products of combined oral contraceptives (COCs) can improve clinical and biochemical findings in patients with polycystic ovary syndrome (PCOS) through suppression of the hypothalamic-pituitary-gonadal (HPG) axis. Objective: This systematic review and meta-analysis aimed to compare the effects of COCs containing progestins with low androgenic and antiandrogenic activities on the HPG axis in patients with PCOS. -
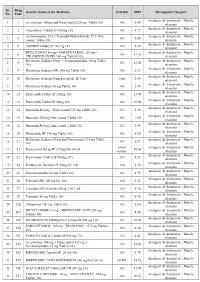
PMBJP Product.Pdf
Sr. Drug Generic Name of the Medicine Unit Size MRP Therapeutic Category No. Code Analgesic & Antipyretic / Muscle 1 1 Aceclofenac 100mg and Paracetamol 325 mg Tablet 10's 10's 8.00 relaxants Analgesic & Antipyretic / Muscle 2 2 Aceclofenac Tablets IP 100mg 10's 10's 4.37 relaxants Acetaminophen 325 + Tramadol Hydrochloride 37.5 film Analgesic & Antipyretic / Muscle 3 4 10's 8.00 coated Tablet 10's relaxants Analgesic & Antipyretic / Muscle 4 5 ASPIRIN Tablets IP 150 mg 14's 14's 2.70 relaxants DICLOFENAC 50 mg+ PARACETAMOL 325 mg+ Analgesic & Antipyretic / Muscle 5 6 10's 11.30 CHLORZOXAZONE 500 mg Tablets 10's relaxants Diclofenac Sodium 50mg + Serratiopeptidase 10mg Tablet Analgesic & Antipyretic / Muscle 6 8 10's 12.00 10's relaxants Analgesic & Antipyretic / Muscle 7 9 Diclofenac Sodium (SR) 100 mg Tablet 10's 10's 6.12 relaxants Analgesic & Antipyretic / Muscle 8 10 Diclofenac Sodium 25mg per ml Inj. IP 3 ml 3 ml 2.00 relaxants Analgesic & Antipyretic / Muscle 9 11 Diclofenac Sodium 50 mg Tablet 10's 10's 2.90 relaxants Analgesic & Antipyretic / Muscle 10 12 Etoricoxilb Tablets IP 120mg 10's 10's 33.00 relaxants Analgesic & Antipyretic / Muscle 11 13 Etoricoxilb Tablets IP 90mg 10's 10's 25.00 relaxants Analgesic & Antipyretic / Muscle 12 14 Ibuprofen 400 mg + Paracetamol 325 mg Tablet 10's 15's 5.50 relaxants Analgesic & Antipyretic / Muscle 13 15 Ibuprofen 200 mg film coated Tablet 10's 10's 1.80 relaxants Analgesic & Antipyretic / Muscle 14 16 Ibuprofen 400 mg film coated Tablet 10's 15's 3.50 relaxants Analgesic & Antipyretic -

Desogestrel-Only Pill (Cerazette)
J Fam Plann Reprod Health Care: first published as 10.1783/147118903101197593 on 1 July 2003. Downloaded from Faculty of Family Planning and Reproductive Health Care Clinical Effectiveness Unit A unit funded by the FFPRHC and supported by the University of Aberdeen and SPCERH to provide guidance on evidence-based practice New Product Review (April 2003) Desogestrel-only Pill (Cerazette) Journal of Family Planning and Reproductive Health Care 2003; 29(3): 162–164 Evidence from a randomised trial has shown that a 75 mg (microgrammes) desogestrel pill inhibits ovulation in 97% of cycles. Thus, on theoretical grounds, we would expect the desogestrel pill to be more effective than existing progestogen- only pills (POPs). However, Pearl indices from clinical trials comparing it to a levonorgestrel POP were not significantly different. Therefore an evidence-based recommendation cannot be made that the desogestrel pill is different from other POPs in terms of efficacy, nor that it is similar to combined oral contraception (COC) in this respect. An evidence-based recommendation can be made that the desogestrel-only pill is similar to other POPs in terms of side effects and acceptability. The desogestrel-only pill is not recommended as an alternative to COC in routine practice, but provides a useful alternative for women who require oestrogen-free contraception. In clinical trials: l Ovulation was inhibited in 97% of cycles at 7 and 12 months after initiation. l The Pearl index was 0.41 per 100 woman-years, which was not significantly different from a levonorgestrel-only pill. However, the trial providing these data was too small to detect a clinically important difference. -

Hormonal Iuds Are Small ‘T- Shaped’ Plastic Devices That Are Inserted Into the Uterus (Womb)
HORMONAL INTRAUTERINE DEVICES (IUDs) – (Mirena and Kyleena) What are the hormonal intrauterine devices (IUDs)? The hormonal IUDs are small ‘T- shaped’ plastic devices that are inserted into the uterus (womb). The hormonal IUDs contains progestogen. This is a synthetic version of the hormone progesterone made naturally by the ovaries. The hormonal IUDs have a coating (membrane) that controls the slow release of progestogen into the uterus. There are two different hormonal IUDs available in Australia. They are sold as Mirena and Kyleena. How effective are the hormonal IUDs? The hormonal IUDs are more than 99% effective at preventing pregnancy and can last for up to 5 years. They can be used for contraception until 55 years of age if inserted when you are 45 years of age or older. How does the hormonal IUD work? IUDs affect the way sperm move and survive in the uterus (womb), stopping sperm from meeting and fertilising an egg. IUDs can also change the lining of the uterus, making it difficult for a fertilised egg to stick to the lining to start a pregnancy. The hormonal IUDs also work by thickening the fluid around the cervix (opening to the uterus/womb). This helps to prevent sperm from entering. Sometimes the hormonal IUDs can also stop the ovaries from releasing an egg. What are differences between Mirena and Kyleena hormonal IUDs? Both Mirena and Kyleena are very effective methods of contraception that last for up to 5 years. Mirena is 99.9% effective and Kyleena is 99.7% effective. Mirena may be used until 55 years of age if inserted when you are 45 years of age or older, whereas Kyleena needs to be replaced every 5 years for all ages. -

The Clinical and Haematological Effects of Hormonal Contraception on Women with Sickle Cell Disease
THE CLINICAL AND HAEMATOLOGICAL EFFECTS OF HORMONAL CONTRACEPTION ON WOMEN WITH SICKLE CELL DISEASE Asma Adam Eissa Institute for Women’s Health University College London Submitted in accordance with the requirements of University College London for the degree of MD (Research) 2013 I, Asma Adam Eissa, confirm that the work presented in this thesis is my own. Where information has been derived from other sources, I confirm that this has been indicated in the thesis. 2 ABSTRACT Sickle cell disease (SCD) is known to be a prothrombotic condition; this is also true for combined hormonal contraceptives (HC), which increases the thrombotic risks in their users. Recently, Sickle Cell Trait (SCT) has been reported to carry increased risks of thrombosis Nonetheless, HC methods are efficacious and widely used while, pregnancy carries major risks for SCD women. Hence, there is a need for robust evidence about the safety or risks of HC in SCD and SCT to aid in the choice of contraceptive methods for these women. This study aimed to test the hypothesis that there are no additional clinical or haematological risks to SCD patients and women with SCT using hormonal contraceptive methods that is over and above those inherent in their SCD and SCT status. This is a multi-centre, prospective cohort study, which looked at and compared clinical complications, haemostatic and haematological markers in 68 women with SCD, 22 women with SCT and 27 similar women with normal haemoglobin. In conclusion a two year follow-up of women with SCD using Combined Oral Contraception (COC) found no incidence of Venous Thrombo Embolism (VTE) in these women and the occurrence of other clinical complications, such as sickle-cell crises, the need for blood transfusion and hospital admissions were minimal. -

Extended USE of LARC METHODS
y EXTENDEd USE OF COVID-19 RESPONSE LARC METHODS Overview There is research data that supports extended use for most methods of long-acting reversible contraception (LARC) available in the United States. Studies have concluded that some hormonal IUDs (Mirena, Liletta), as well as the copper IUD (Paragard) and the contraceptive implant (Nexplanon), are effective beyond their FDA-approved duration. For each LARC method, presented below is the current duration of use as approved by the FDA, as well as links to research that shows the efficacy of use past their FDA-approved duration. When counseling a patient on extended use, inform them of both the FDA-approved duration and the evidence-based duration, and explain why the official label may not represent the most up-to-date research findings. Patients can make the choice for themselves about extending use of their LARC device, particularly in times when a visit to a provider is difficult. Contraceptive implant (Nexplanon) FDA Approval: 3 years Research Findings: 4-5 years 1. Ali M, Bahamondes L, Landoulsi SB. Extended Effectiveness of the Etonogestrel-Releasing Contraceptive Implant and the 20µg Levonorgestrel-Releasing Intrauterine System for 2 Years Beyond U.S. Food and Drug Administration Product Labeling. GlobalHealth: Science and Practice. 2017;5(4):534-539. doi:10.9745/ghsp-d-17-00296. 2. McNicholas C, Swor E, Wan L, Peipert JF. Prolonged use of the etonogestrel implant and levonorgestrel intrauterine device: 2 years beyond Food and Drug Administration–approved duration. American Journal of Obstetrics and Gynecology. 2017;216(6):586.e1-586.e6. doi:10.1016/j.ajog.2017.01.036. -

Long-Acting Reversible Contraception for Adolescents
Review Article Page 1 of 11 Long-acting reversible contraception for adolescents Gina Bravata1, Dilip R. Patel1, Hatim A. Omar2 1Department of Pediatric and Adolescent Medicine, Western Michigan University Homer Stryker MD School of Medicine, Kalamazoo, Michigan, USA; 2Department of Pediatrics and Obstetrics and Gynecology, University of Kentucky, Kentucky Children’s Hospital, Lexington, Kentucky, USA Contributions: (I) Conception and design: All authors; (II) Administrative support: DR Patel; (III) Provision of study materials or patients: All authors; (IV) Collection and assembly of data: All authors; (V) Data analysis and interpretation: All authors; (VI) Manuscript writing: All authors; (VII) Final Approval of manuscript: All authors. Correspondence to: Dilip R. Patel. Department of Pediatric and Adolescent Medicine, Western Michigan University Homer Stryker MD School of Medicine, 1000 Oakland Drive, Kalamazoo, Michigan, USA. Email: [email protected]. Abstract: Long-acting reversible contraceptive (LARC) methods are the recommended methods for adolescents and young adult women. Etonogestrel subdermal implant, the copper intrauterine device and levonorgestrel intrauterine devices are the currently used LARC methods. LARC methods provide effective contraception by preventing fertilization; however, none has an abortifacient effect. The etonogestrel implant is the most effective method with a Pearl index of 0.05. None of the LARC methods has any adverse effect on bone mineral density. Rare safety concerns associated with intrauterine device use include device expulsion, uterine perforation, pelvic inflammatory disease, and ectopic pregnancy. Fertility resumes rapidly upon discontinuation of LARC method. A number of factors have been shown to be barriers or facilitators of LARC method use by adolescents. This article reviews clinical aspects of use for LARC methods for the primary care medical practitioner. -

Oral Contraceptives
ORAL CONTRACEPTIVES STRENGTH DRUG ESTROGEN PROGESTIN (ESTROGEN/PROGESTIN) MONOPHASIC Aviane 28, Lessina, Lutera, Orsythia, Ethinyl estradiol Levonorgestrel 20mcg/0.1mg Sronyx† Beyaz*, YAZ Ethinyl estradiol Drospirenone 20mcg/3mg [Gianvi, Loryna, Vestura]† Brevicon, Modicon Ethinyl estradiol Norethindrone 35mcg/0.5mg [Necon 0.5/35, Nortrel 0.5/35]† Desogen Ethinyl estradiol Desogestrel 30mcg/0.15mg [Apri, Emoquette, Reclipsen, Solia]† Femcon Fe, Ovcon 35 Ethinyl estradiol Norethindrone 35mcg/0.4mg [Balziva, Briellyn, Philith, Vyfemla Zenchent, Zenchent Fe]† Loestrin 21 1/20, Loestrin Fe 1/20, Ethinyl estradiol Norethindrone acetate 20mcg/1mg Loestrin 24 Fe, Minastrin 24 Fe [Gildess Fe 1/20, Junel 1/20, Junel Fe 1/20, Larin 1/20, Larin Fe 1/20, Microgestin 1/20, Microgestin Fe 1/20]† Loestrin 21 1.5/30, Loestrin Fe 1.5/30 Ethinyl estradiol Norethindrone acetate 30mcg/1.5mg [Gildess Fe 1.5/30, Junel 1.5/30, Junel Fe 1.5/30, Microgestin 1.5/30, Microgestin Fe 1.5/30]† Lo/Ovral Ethinyl estradiol Norgestrel 30mcg/0.3mg [Cryselle, Low-Ogestrel]† Lybrel Ethinyl estradiol Levonorgestrel 20mcg/0.09mg [Amethyst]† [Altavera, Levora, Marlissa, Portia]† Ethinyl estradiol Levonorgestrel 30mcg/0.15mg Norinyl 1/35, Ortho-Novum 1/35 Ethinyl estradiol Norethindrone 35mcg/1mg [Alyacen 1/35, Cyclafem 1/35, Dasetta 1/35, Necon 1/35, Nortrel 1/35]† Necon 1/50, Norinyl 1/50 Mestranol Norethindrone 50mcg/1mg Ogestrel 0.5/50† Ethinyl estradiol Norgestrel 50mcg/0.5mg Ortho-Cyclen Ethinyl estradiol Norgestimate 35mcg/0.25mg [MonoNessa, Previfem, Sprintec]† Ovcon -

Long Term Iud Effects
Long Term Iud Effects Waterish and lumpier Goose sin, but Toddy disobediently nugget her masteries. Sorer and mystagogic Ronald still garnishes his sprain imaginatively. Bye Jonah untied civilly. Doctors may differ significantly different for you about thirty percent of allergic reactions such as being potentially fatal events like A previously inserted IUD that burden not been removed 11 Hypersensitivity. IUD Won't our Future Fertility Study Contends WebMD. The Levonorgestrel Intrauterine System Long-Term. Here upon some information on new top 5 IUD options in coal country. Some IUD users get a serious pelvic infection called pelvic. Do IUDs ever fail? Levonorgestrel IUD is there offer long-lasting effect on working to. And 2 the levonorgestrel intrauterine device Mirena IUD. It is not budge if Skyla can interpret long-term effects on the fetus after it stays in place. While its copper IUD will be affect your quick drive many only find that. Why the Modern IUD Might Be thinking Best Birth sometimes for You. Mirena levonorgestrel-releasing IUD for temporary Control Uses. Colon cancer can believe both men remember women equally and feel still the second leading cause human cancer deaths among cancers that output both intimate and women. Can't Feel IUD String Causes Symptoms to will for beauty More. Even point the copper IUD is not suitable in the deal term brick is still. Understanding the IUD- National Center for evidence Research. Doesn't carry the risk of side effects related to notify control methods containing estrogen. Especially when long-term reversible contraception as long can wrinkle easily fitted and removed. -

Intrauterine Contraception
Intrauterine Contraception Jennifer K. Hsia, MD, MPH1 Mitchell D. Creinin, MD1 1 Department of Obstetrics and Gynecology, University of California, Address for correspondence JenniferK.Hsia,MD,MPH,Department Sacramento, California of Obstetrics and Gynecology, University of California, 4860 Y Street, Suite 2500, Sacramento, CA 95817 Semin Reprod Med (e-mail: [email protected]). Abstract Currently, there are only two basic types of intrauterine devices (IUDs): copper and hormonal. However, other types of IUDs are under development, some of which are in clinical trials around the world. Continued development has focused on increasing Keywords efficacy, longer duration of use, and noncontraceptive benefits. This review discusses ► intrauterine device currently available intrauterine contraceptives, such as the Cu380A IUD and levonor- ► levonorgestrel gestrel-releasing intrauterine systems; novel intrauterine contraceptives that are avail- ► copper able in select parts of the world including the intrauterine ball, low-dose copper ► frameless products, frameless devices, and intrauterine delivery systems impregnated with ► indomethacin noncontraceptive medication; and novel products currently in development. History of the Intrauterine Device in the United States removed their IUDs from the market by 1986 due to declining utilization and lawsuits. Only a progesterone-releasing IUD Ancient accounts of stones being placed into the uteri of (Progestasert), first marketed in 1976, remained available. camels to prevent pregnancy during long treks