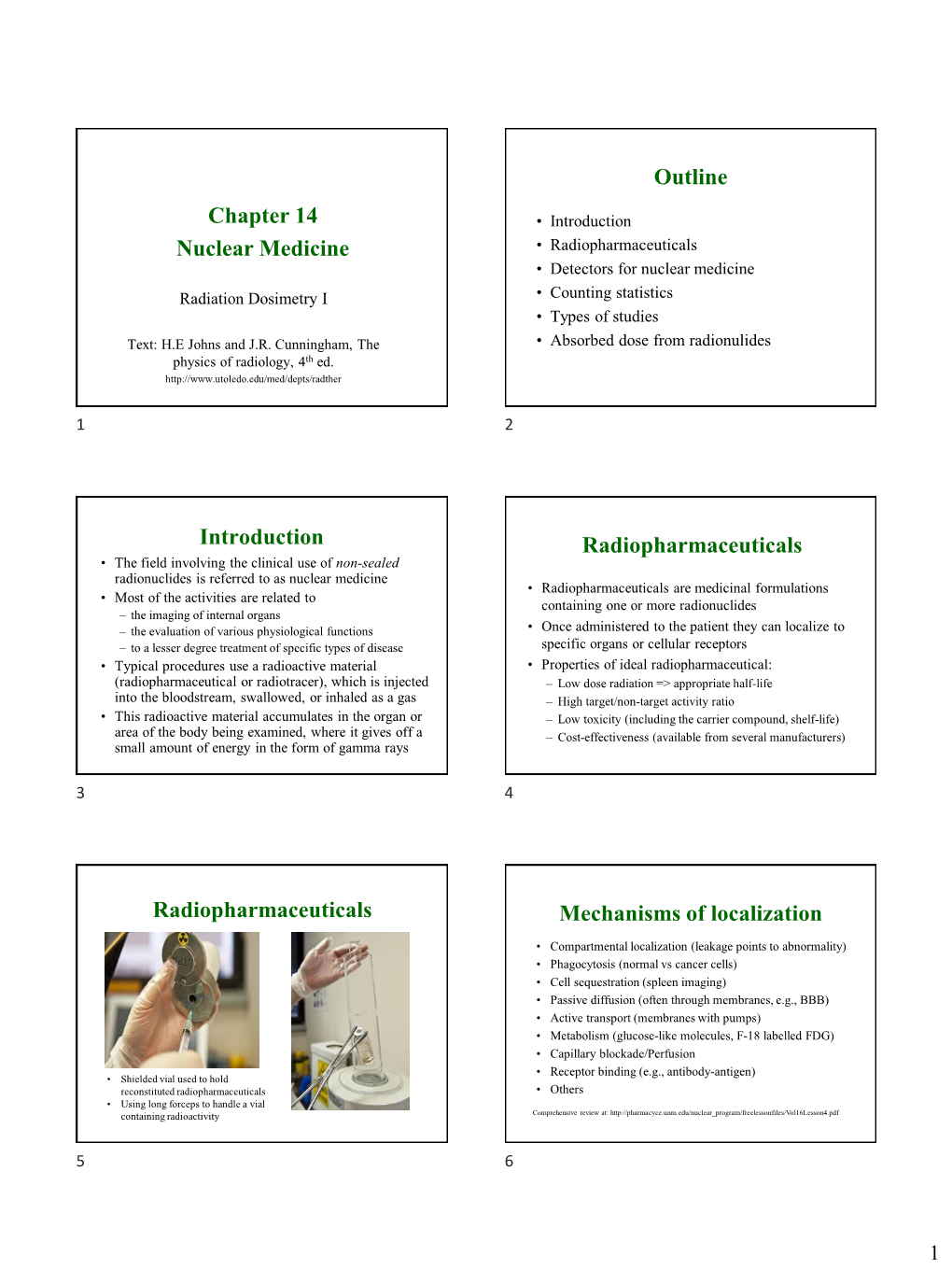
Chapter 14 Nuclear Medicine Outline Introduction Radiopharmaceuticals Radiopharmaceuticals Mechanisms of Localization
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

OPERATIONAL GUIDANCE on HOSPITAL RADIOPHARMACY: a SAFE and EFFECTIVE APPROACH the Following States Are Members of the International Atomic Energy Agency
OPERATIONAL GUIDANCE ON HOSPITAL RADIOPHARMACY: A SAFE AND EFFECTIVE APPROACH The following States are Members of the International Atomic Energy Agency: AFGHANISTAN GUATEMALA PAKISTAN ALBANIA HAITI PALAU ALGERIA HOLY SEE PANAMA ANGOLA HONDURAS PARAGUAY ARGENTINA HUNGARY PERU ARMENIA ICELAND PHILIPPINES AUSTRALIA INDIA POLAND AUSTRIA INDONESIA PORTUGAL AZERBAIJAN IRAN, ISLAMIC REPUBLIC OF QATAR BANGLADESH IRAQ REPUBLIC OF MOLDOVA BELARUS IRELAND ROMANIA BELGIUM ISRAEL RUSSIAN FEDERATION BELIZE ITALY SAUDI ARABIA BENIN JAMAICA SENEGAL BOLIVIA JAPAN SERBIA BOSNIA AND HERZEGOVINA JORDAN SEYCHELLES BOTSWANA KAZAKHSTAN BRAZIL KENYA SIERRA LEONE BULGARIA KOREA, REPUBLIC OF SINGAPORE BURKINA FASO KUWAIT SLOVAKIA CAMEROON KYRGYZSTAN SLOVENIA CANADA LATVIA SOUTH AFRICA CENTRAL AFRICAN LEBANON SPAIN REPUBLIC LIBERIA SRI LANKA CHAD LIBYAN ARAB JAMAHIRIYA SUDAN CHILE LIECHTENSTEIN SWEDEN CHINA LITHUANIA SWITZERLAND COLOMBIA LUXEMBOURG SYRIAN ARAB REPUBLIC COSTA RICA MADAGASCAR TAJIKISTAN CÔTE D’IVOIRE MALAWI THAILAND CROATIA MALAYSIA THE FORMER YUGOSLAV CUBA MALI REPUBLIC OF MACEDONIA CYPRUS MALTA TUNISIA CZECH REPUBLIC MARSHALL ISLANDS TURKEY DEMOCRATIC REPUBLIC MAURITANIA UGANDA OF THE CONGO MAURITIUS UKRAINE DENMARK MEXICO UNITED ARAB EMIRATES DOMINICAN REPUBLIC MONACO UNITED KINGDOM OF ECUADOR MONGOLIA GREAT BRITAIN AND EGYPT MONTENEGRO NORTHERN IRELAND EL SALVADOR MOROCCO ERITREA MOZAMBIQUE UNITED REPUBLIC ESTONIA MYANMAR OF TANZANIA ETHIOPIA NAMIBIA UNITED STATES OF AMERICA FINLAND NEPAL URUGUAY FRANCE NETHERLANDS UZBEKISTAN GABON NEW ZEALAND VENEZUELA GEORGIA NICARAGUA VIETNAM GERMANY NIGER YEMEN GHANA NIGERIA ZAMBIA GREECE NORWAY ZIMBABWE The Agency’s Statute was approved on 23 October 1956 by the Conference on the Statute of the IAEA held at United Nations Headquarters, New York; it entered into force on 29 July 1957. The Headquarters of the Agency are situated in Vienna. -
Azedra) Reference Number: ERX.SPA.420 Effective Date: 03.01.21 Last Review Date: 02.21 Line of Business: Commercial, Medicaid Revision Log
Clinical Policy: Iobenguane I-131 (Azedra) Reference Number: ERX.SPA.420 Effective Date: 03.01.21 Last Review Date: 02.21 Line of Business: Commercial, Medicaid Revision Log See Important Reminder at the end of this policy for important regulatory and legal information. Description Iobenguane I-131 (Azedra®) injection is a radioactive agent. FDA Approved Indication(s) Azedra is indicated for the treatment of adult and pediatric patients 12 years and older with iobenguane scan positive, unresectable, locally advanced or metastatic pheochromocytoma or paraganglioma who require systemic anticancer therapy. Policy/Criteria Provider must submit documentation (such as office chart notes, lab results or other clinical information) supporting that member has met all approval criteria. Health plan approved formularies should be reviewed for all coverage determinations. Requirements to use preferred alternative agents apply only when such requirements align with the health plan approved formulary. It is the policy of health plans affiliated with Envolve Pharmacy Solutions™ that Azedra is medically necessary when the following criteria are met: I. Initial Approval Criteria A. Pheochromocytoma and Paraganglioma (must meet all): 1. Diagnosis of pheochromocytoma or paraganlioma; 2. Prescribed by or in consultation with an oncologist; 3. Age ≥ 12 years; 4. Tumor is unresectable, locally advanced, or metastatic; 5. Member currently receives medication to control tumor secretion of catecholamines (e.g., epinephrine, norepinephrine, dopamine) and related symptoms (e.g., hypertension, arrhythmia, hyperglycemia); 6. Metaiodobenzylguanidine (MIBG) scan is positive; 7. Concurrent radiopharmaceuticals have not been prescribed (e.g., Lutathera® [lutetium lu-177 dotatate]); 8. Request meets one of the following (a or b):* a. Dose does not exceed (i or ii): i. -
COMMENT (11) Status: Pending Post PUBLIC SUBMISSION PUBLICATION Tracking No
Page 1 of 2 SUNSI Review Complete Template = ADM-013 E-RIDS=ADM-03 ADD: Jazel Parks, As of: 10/1/19 1:22 PM Harriet Karagiannis Received: September 25, 2019 COMMENT (11) Status: Pending_Post PUBLIC SUBMISSION PUBLICATION Tracking No. 1k3-9ce3-dnzr DATE: 7/26/2019 Comments Due: September 26, 2019 CITATION 84 FR Submission Type: Web 36127 Docket: NRC-2019-0154 Release of Patients Administered Radioactive Material Comment On: NRC-2019-0154-0003 Release of Patients Administered Radioactive Material; Extension of comment period Document: NRC-2019-0154-DRAFT-0012 Comment on FR Doc # 2019-17060 Submitter Information Name: Daniel Miron Address: W176S8019 Joel Drive Muskego, WI, 53150 Email: [email protected] General Comment I am pleased to comment on the draft regulatory guide (DG), DG-8057, Release of Patients Administered Radioactive Material that was published in the Federal Register on July 26, 2019. (Docket ID NRC-2019- 0154). I am a health physicist who is certified by the American Board of Health Physics and have over 25 years of health physics experience in medical health physics. This includes being the Radiation Safety Officer (RSO) on multiple limited scope and broad scope medical licenses. I recommend that the data for I-123 NaI in table 3 Activities of Radiopharmaceuticals That Require Instructions and Records When Administered to Patients Who Are Breastfeeding an Infant or Child be reviewed and updated to reflect the current clinical use of I-123 NaI. Specifically the recommended duration of interruption of breastfeeding should be changed to Complete cessation due to the reasons listed below. -

The Evolving Landscape of Therapeutic and Diagnostic Radiopharmaceuticals
ARTICLE THE EVOLVING LANDSCAPE OF THERAPEUTIC AND DIAGNOSTIC RADIOPHARMACEUTICALS Therapeutic and diagnostic approaches involving the use of radiation and radioactive compounds have a long- standing history in the fields of science and medicine. Radiotherapy was first used in cancer treatments in 1896.1 Since then, the field of radiation has advanced to further understand how radioactive compounds interact with biological tissues and how they can be used in both diagnostic and therapeutic applications. Radiopharmaceuticals are compounds used for medicinal purposes that contain radioactive isotopes (also known as radionuclides) and can be diagnostic or therapeutic in nature, or both.2 They represent a unique category of pharmaceuticals due to their radioactive properties. As such, there are specific guidelines and regulations that impact and direct the study and use of these compounds. Radiopharmaceutical drug development has rapidly expanded over the last decade. Radiopharmaceuticals are widely used in the field of imaging for diagnosis, staging, and follow up; in the realm of therapeutics, their use has increased, most notably, in the area of oncology. In a recent webinar, experts from Medpace’s radiation oncology, imaging, regulatory, and operational teams discussed the growing space of radiopharmaceutical development with respect to their biological use and application, regulatory frameworks that govern their evaluation in support of approvals, operational manufacturing considerations, and associated imaging approaches. BIOLOGICAL MECHANISMS OF ACTION OF RADIONUCLIDES According to Dr. Jess Guarnaschelli, Medical Director, Radiation Oncology, the radioactivity of radionuclides can be employed for both diagnostic and therapeutic medical uses. While external beam ionizing radiation involves radiation emitted in the form of electromagnetic waves or particles, radiopharmaceuticals use radionuclides to deliver localized radiation to specific targets. -

Thyroid Uptake and Imaging with Iodine-123 at 4-5 Hours
ThyroidUptake and Imaging with Iodine-123 at 4-5 Hours: Replacement of the 24-Hour Iodine-131 Standard John L. Floyd, Paul R. Rosen, Ronald D. Borchent, Donald E. Jackson, and Frednick L. Weiland Nuclear Medicine Section, Department ofRadiology, David Grant USAF Medical Center, Travis AFB, California; Nuclear Medicine Department, Boston Children's Hospital. Boston, Massachusetts; Nuclear Medicine Section, Department ofRadiology, and Wilford Hall USAF Medical Center, Lackland AFB, San Antonio, Texas. A studywas canied outto determinethe suitabilityof utilizinga 4 to 5 hr intervalfrom edministration of lodine-123 to imaging and uptake measurement as a replacement for the 24-hr standardoriginallyestablishedwith Iodine-131. In 55 patientswho underwent scintigraphy at 4 and 24 hr. there was no discrepancy between paired images. In 55 patientswho hal uptakemeasuredat 4 and 24 lwandin 191 patientswho haduptake measuredat 5 and 24 lw,the earlymeastrementsprovedequalor betterdiscrimantsof euthyroldfrom hyperthyroidpatients.Inour Institutions,thesefindingsandthe lOgiStical advantagesof completingthe exam in 4—5hr ledusto abandonthe 24-hr studyin the majorityof patients. J Nucl Med 26:884—887,1985 he benchmark of iodine accumulation by the thy and/on uptake measurements has remained tied to the noid gland has been the “24-hournadioiodine uptake― 24-hr 1311standard. The inconvenience and expense since the post-World War II introduction of clinical often associated with a 2-day test has led many depart thyroid investigation with reactor-produced iodine-131 ments to use pertechnetate for imaging and utilize 1231 (‘@‘I).With the development of the rectilinear scanner or ‘@‘Ionly when an uptake is specifically required. by Cassen in 1951, the “24-houruptake and scan― Though 1-hr 123!images are inferior to 24-hr scinti became the world-standard test for anatomical map grams (4), successful thyroid imaging at 4—6hr after ping and functional assessment of the thyroid. -

Mechanisms of Radiopharmaceutical Localization
.::VOLUME 16, LESSON 4::. Mechanisms of Radiopharmaceutical Localization Continuing Education for Nuclear Pharmacists And Nuclear Medicine Professionals By James A. Ponto, MS, RPh, BCNP Chief Nuclear Pharmacists, University of Iowa Hospitals and Clinics and Professor (Clinical), University of Iowa Hospitals and Clinics The University of New Mexico Health Sciences Center, College of Pharmacy is accredited by the Accreditation Council for Pharmacy Education as a provider of continuing pharmacy education. Program No. 0039-000-12-164- H04-P 2.5 Contact Hours or .25 CEUs. Initial release date: 7/19/2012 -- Intentionally left blank -- Mechanisms of Radiopharmaceutical Localization By James A. Ponto, MS, RPh, BCNP Editor, CENP Jeffrey Norenberg, MS, PharmD, BCNP, FASHP, FAPhA UNM College of Pharmacy Editorial Board Stephen Dragotakes, RPh, BCNP, FAPhA Michael Mosley, RPh, BCNP Neil Petry, RPh, MS, BCNP, FAPhA James Ponto, MS, RPh, BCNP, FAPhA Tim Quinton, PharmD, BCNP, FAPhA S. Duann Vanderslice, RPh, BCNP, FAPhA John Yuen, PharmD, BCNP Advisory Board Dave Engstrom, PharmD, BCNP Vivian Loveless, PharmD, BCNP, FAPhA Brigette Nelson, MS, PharmD, BCNP Brantley Strickland, BCNP Susan Lardner, BCNP Christine Brown, BCNP Director, CENP Administrator, CE & Web Publisher Kristina Wittstrom, MS, RPh, BCNP, FAPhA Christina Muñoz, M.A. UNM College of Pharmacy UNM College of Pharmacy While the advice and information in this publication are believed to be true and accurate at the time of press, the author(s), editors, or the publisher cannot accept any legal responsibility for any errors or omissions that may be made. The publisher makes no warranty, expressed or implied, with respect to the material contained herein. -

Nuclear Imaging Advances and Trends
Liver scintigraphy of patient in Pakistan's Larkana Institute of Nuclear Medicine and Radiotherapy. (Credit: Pakistan AEC) Nuclear imaging Advances and trends Developments in several fields are influencing future directions by Gerard van Herk ' 'One picture is worth more than a thousand words''. The type of gamma camera that still is most com- The validity of this expression, which is a leitmotiv monly used is the one designed by Hal Anger in 1959. in the publicity sector, is not limited to the strategy In the "Anger" gamma camera, the radioactive distri- underlying advertisements. It certainly also applies to bution is projected as a whole through a parallel-hole the commanding role images play in diagnostic medi- collimator onto a thin scintillation crystal. The diameter cine. To draw lines of development in imaging instru- of its field of view can range from 18 to 50 centimetres. ments, one must start where the arsenal of nuclear Each scintillation event on the crystal is "seen" by an medicine equipment stands today. In this article, nuclear array of photomultiplier tubes (PMTs, typically 19 to imaging instruments that are likely to be of interest to the 75). The relative outputs of the PMTs are analysed by nuclear medicine community of developing countries are an electronic positioning network, which produces two emphasized. position signals per registered photon. When entered The rectilinear scanner was the earliest instrument into a display monitor, the original "scintillation" is with which one created an image of a radioactive distri- represented by a corresponding light dot on the screen. bution inside the body. -

Determination of Iodine Uptake by Cancer Thyroid Cells with Μ-AMS and Gamma Detector
Determination of iodine uptake by cancer thyroid cells with µ-AMS and gamma detector Ana Sofia Gusmão Gomes Thesis to obtain the Master of Science Degree in Biomedical Technologies Supervisor: Dr. Maria de Lurdes Gano Dr. Hélio Fernandes Luís Examination Committee Chairperson: Prof. Maria Margarida Fonseca Rodrigues Diogo Supervisor: Dr. Hélio Fernandes Luís Members of the committee: Prof. Maria Micaela Leal da Fonseca November of 2016 Abstract: Compared with the normal thyroid cells, thyroid cancer cells have a reduced iodine uptake. Nevertheless, radioactive iodine is the principal treatment for thyroid cancer. The aim of this dissertation is to evaluate the possibility of the use of µ-AMS as an alternative to gamma counting techniques in studies of iodine uptake in thyroid cells. For the determination of the precision and accuracy of the gamma counter used in bioassay laboratory of radiopharmaceutical group in CTN, 3 tubes with 125I solution and an activity of 0,9 µCi were prepared. These were used for the determination of the geometric effect, the reproducibility of the measurements, detection efficiency and the detection limit for 125I. In order to determine the detection limit for 129I with LATR/CTN µ-AMS system, an AgI pellet was made and measured. Another pellet, using carcinoma cells, was made to mimic the extraction of 129I by thyroid. The study allowed us to conclude that, the Berthold LB2111 can detect a minimum of 9,6x107 125I particles (4%uncertainity) compared with 2,8x105 127I particles (1% uncertainty) by µ-AMS. Since cancer cells have a lower iodine uptake than healthy cells, the better detection limit of µ-AMS is a valuable tool in the study of iodine uptake of thyroid cancer cells. -

Simulation Studies of Nuclear Medicine Instrumentation
Simulation Studies of Nuclear Medicine Instrumentation A. G. Schulz L. G. Knowles L. C. Kohlenstein A BOUT FIVE YEARS AGO A GROUP at the Applied high noise levels and poor spatial resolution which ~ Physics Laboratory began a study of the make interpretation difficult. Improving the inter design of instrumentation systems for use in nu pretability of these images through increased sys clear medicine under the guidance of Professor tem performance is thus highly desirable. Attempts H. N. Wagner, J r. , of The Johns Hopkins Medical to develop a quantitative science for evaluating Institutions. A critical goal of these nuclear medi system performance have been hampered by the cine systems is to produce an image of a soft tedious and time consuming efforts necessary to organ within the body, such as the liver or brain, conduct suitable experiments with clinical equip with the objective of detecting tumors or organ ment. It appeared that all significant elements dysfunction. 1 The images are characterized by of the medical problem and the instrumentation could be simulated and "experiments" could be This research is supported by the U.S. Public Health Service conducted on variations of the system with ease, Grant No. GM 10548 from the National Institute of General using digital simulation techniques familiar to Medical Sciences. those with experience in the development of large 1 H . N. Wagner, Jr., Principles of Nuclear Medicine, W . B. Saunders Company, Philadelphia, 1968. systems. In the following sections a brief intro- 2 APL T echnical Digest A digital simulation of the radionuclide scanning process has been developed to aid in the quantitative evaluation of the clinical significance of instrumentation techniques and operational parameters associated with these systems. -

Well Scintillation Counting Systems for Nuclear Medicine Applications Indeveloping Countries
IAEA-201 WELL SCINTILLATION COUNTING SYSTEMS FOR NUCLEAR MEDICINE APPLICATIONS INDEVELOPING COUNTRIES REPORT OF A CONSULTANTS' MEETING ORGANIZED BY THE INTERNATIONAL ATOMIC ENERGY AGENCY VIENNA, 23-25 MAY 1977 t#\ ~ A TECHNICAL DOCUMENT ISSUED BY THE (4..)INTERNATIONAL ATOMIC ENERGY AGENCY, VIENNA, 1977 Printed by the IAEA in Austria September 1977 PLEASE BE AWARE THAT ALL OF THE MISSING PAGES IN THIS DOCUMENT WERE ORIGINALLY BLANK The IAEA does not maintain stocks of reports in this series. However, microfiche copies of these reports can be obtained from INIS Microfiche Clearinghouse International Atomic Energy Agency Kimtner Ring 11 P.O. Box 590 A-1011 Vienna, Austria on prepayment of US $0.65 or against one IAEAmicrofiche service coupon. FOREWORD Nuclear medicine instruments employed in developing countries are usually acquired from the commercial market in developed countries. They thus embody the technological refinements characteristic of that market, but are by the same token optimized for purposes and conditions of use that may differ substantially from those found in developing countries. Furthermore, the diversity of instruments in this market is great, and their design is undergoing a very rapid evolution. It is, therefore, inevitable both that the instruments are not optimized for use in developing countries and that a rational selection even from among those available is difficult for the consumer in the developing country to make. A consultants' meeting was organized by the Medical Applications Section of the Division of Life Sciences, IAE&, during the period 23-25 May 1977, to examine well scintillation counting systems in the light of the requirements of laboratories in developing` countries. -

Nuclear Data Relevant to the Production of Radioiodine I-123, I
International Letters of Chemistry, Physics and Astronomy Online: 2016-01-04 ISSN: 2299-3843, Vol. 63, pp 90-97 doi:10.18052/www.scipress.com/ILCPA.63.90 CC BY 4.0. Published by SciPress Ltd, Switzerland, 2016 Nuclear Data Relevant to the Production of Radioiodine I-123, I-125 by Indirect Route and Medical Applications Iman Tarik Al-Alawy* Raghad Saadoon Mohammed Al-Mustansiriyah University, College of Science, Physics department, Baghdad – Iraq *Email: [email protected] Keywords: Medical radioisotopes, Iodine production, Cross Section, Indirect reactions, Recommended values. ABSTRACT. The use of radioactive Iodine plays an important role in the treatment of some diseases and diagnosis of others, since they have suitable half-life. The radioactivity emitted from the dissolution of radioactive I-123 and I-125, such as the emission of Auger electrons, positrons and gamma rays reduce the spread of these diseases. Therefore, in this work we discuss the Iodine production via indirect reactions. In order to calculate the cross sections of these reactions for the mentioned target elements, we recommended the cross sections for EXFOR library using the recom.m program, which is written in the present work using Matlab-8, the data are taken from different authors. In order to supply accurate databases for different practical purposes such as proton beam energy monitoring, I-123 and I-125 radioisotopes production, we have evaluated the cross section collected from IAEA for EXFOR library measured by different authors of (p,xn), (d,xn) nuclear process. The selected data and our recommended cross sections were developed for practical applications. -

12-Liquid and Solid Scintillation
Handbook of instrumental techniques from CCiTUB Liquid and solid scintillation: principles and applications BT.12 Carmen Benito 1, Andrés Jiménez 2, Cristina Sánchez 3, and Aurea Navarro- Sabaté 4 Unitat de Protecció Radiològica, CCiTUB, Universitat de Barcelona. 1 IRA Biologia. Diagonal 645. 08028 Barcelona, Spain. 2 IRA Farmàcia. Joan XXIII s/n. 08028 Barcelona, Spain 3 IRA Medicina. Casanovas 143. 08036 Barcelona, Spain. 4 IRA Bellvitge. Feixa Llarga s/n. 08097 L’Hospitalet de Llobregat, Spain email: [email protected], [email protected], cristinasanchez@ccit. ub.edu, [email protected] Abstract . Scintillation counting is one of the most important developments in the application of radioisotopes to procedures needed by scientists, physicians, engineers, and technicians from many diverse discipline for the detection and quantitative measurement of radioactivity. In fact, Scintillation is the most sensitive and versatile technique for the detection and quantification of radioactivity. Particularly, Solid and Liquid scintillation measurement are, nowadays, standard laboratory methods in the life-sciences for measuring radiation from gamma- and beta-emitting nuclides, respectively. This methodology is used routinely in the vast majority of diagnostic and/or research laboratories from those of biochemistry and biology to clinical departments. Liquid and solid scintillation 1. Introduction Radioactive isotopes of common elements are extremely useful in life science disciplines, among others, because radioactive atoms can be substituted for their non radioactive counterparts in chemical formulations. The resulting radioactive compound is easily detectable but still chemically identical to the original material. Two different systems of detection and counting of radiolabeled compounds based on the scintillation technique have been developed: Solid Scintillation Counting (SSC) and Liquid Scintillation Counting (LSC) depending on the scintillator material used.