Disorders of the Male Reproductive System
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

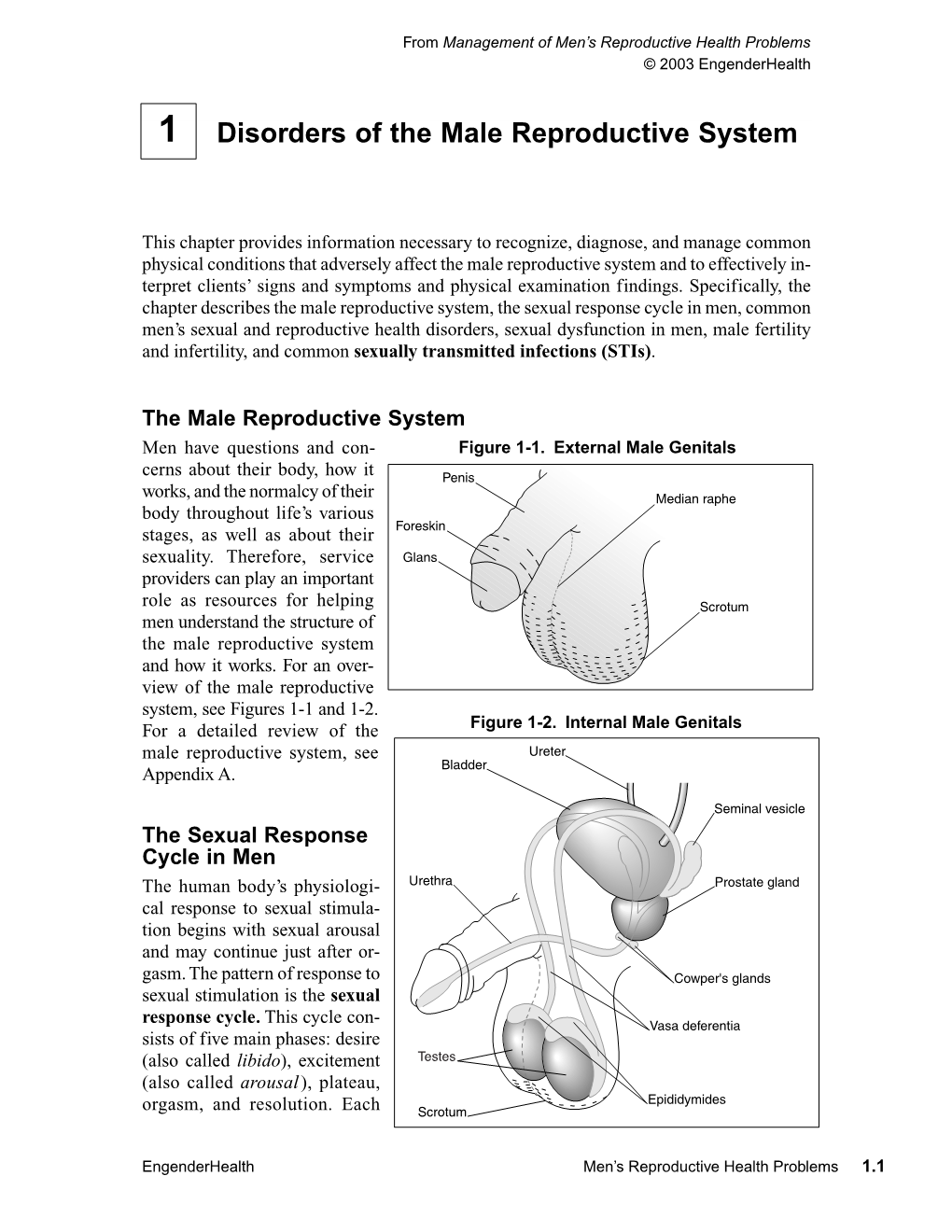
The Male Reproductive System
Management of Men’s Reproductive 3 Health Problems Men’s Reproductive Health Curriculum Management of Men’s Reproductive 3 Health Problems © 2003 EngenderHealth. All rights reserved. 440 Ninth Avenue New York, NY 10001 U.S.A. Telephone: 212-561-8000 Fax: 212-561-8067 e-mail: [email protected] www.engenderhealth.org This publication was made possible, in part, through support provided by the Office of Population, U.S. Agency for International Development (USAID), under the terms of cooperative agreement HRN-A-00-98-00042-00. The opinions expressed herein are those of the publisher and do not necessarily reflect the views of USAID. Cover design: Virginia Taddoni ISBN 1-885063-45-8 Printed in the United States of America. Printed on recycled paper. Library of Congress Cataloging-in-Publication Data Men’s reproductive health curriculum : management of men’s reproductive health problems. p. ; cm. Companion v. to: Introduction to men’s reproductive health services, and: Counseling and communicating with men. Includes bibliographical references. ISBN 1-885063-45-8 1. Andrology. 2. Human reproduction. 3. Generative organs, Male--Diseases--Treatment. I. EngenderHealth (Firm) II. Counseling and communicating with men. III. Title: Introduction to men’s reproductive health services. [DNLM: 1. Genital Diseases, Male. 2. Physical Examination--methods. 3. Reproductive Health Services. WJ 700 M5483 2003] QP253.M465 2003 616.6’5--dc22 2003063056 Contents Acknowledgments v Introduction vii 1 Disorders of the Male Reproductive System 1.1 The Male -

Trauma-Associated Pulmonary Laceration in Dogs—A Cross Sectional Study of 364 Dogs
veterinary sciences Article Trauma-Associated Pulmonary Laceration in Dogs—A Cross Sectional Study of 364 Dogs Giovanna Bertolini 1,* , Chiara Briola 1, Luca Angeloni 1, Arianna Costa 1, Paola Rocchi 2 and Marco Caldin 3 1 Diagnostic and Interventional Radiology Division, San Marco Veterinary Clinic and Laboratory, via dell’Industria 3, 35030 Veggiano, Padova, Italy; [email protected] (C.B.); [email protected] (L.A.); [email protected] (A.C.) 2 Intensive Care Unit, San Marco Veterinary Clinic and Laboratory, via dell’Industria 3, 35030 Veggiano, Padova, Italy; [email protected] 3 Clinical Pathology Division, San Marco Veterinary Clinic and Laboratory, via dell’Industria 3, 35030 Veggiano, Padova, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-0498561098 Received: 5 March 2020; Accepted: 8 April 2020; Published: 12 April 2020 Abstract: In this study, we describe the computed tomography (CT) features of pulmonary laceration in a study population, which included 364 client-owned dogs that underwent CT examination for thoracic trauma, and compared the characteristics and outcomes of dogs with and without CT evidence of pulmonary laceration. Lung laceration occurred in 46/364 dogs with thoracic trauma (prevalence 12.6%). Dogs with lung laceration were significantly younger than dogs in the control group (median 42 months (interquartile range (IQR) 52.3) and 62 months (IQR 86.1), respectively; p = 0.02). Dogs with lung laceration were significantly heavier than dogs without laceration (median 20.8 kg (IQR 23.3) and median 8.7 kg (IQR 12.4 kg), respectively p < 0.0001). When comparing groups of dogs with thoracic trauma with and without lung laceration, the frequency of high-energy motor vehicle accident trauma was more elevated in dogs with lung laceration than in the control group. -

Ultrasonography and Elastography Imaging
Jemds.com Case Report Post Traumatic Hematocele - Ultrasonography and Elastography Imaging Shivesh Pandey1, Suresh Vasant Phatak2, Gopidi Sai Nidhi Reddy3, Apoorvi Bharat Shah4 1, 2, 3, 4 Department of Radio diagnosis, Jawaharlal Nehru Medical College, Sawangi (Meghe), Wardha, Maharashtra India. INTRODUCTION Hematocele with blunt scrotal trauma is an uncommon cause of the testicular pain. Corresponding Author: Elastography is the new recent advance in the field of ultrasound. USG and Dr. Suresh Vasant Phatak, elastography findings of the acute hematocele is described in this aricle. Department of Radiodiagnosis, Jawaharlal Testicular trauma is the third most common cause of acute scrotal pain,1 and Nehru Medical College, Sawangi (Meghe), high-frequency ultrasonography (USG) with a linear array transducer is the first Wardha, Maharashtra – 442001, India. E-mail: [email protected] preferred modality for testicular trauma evaluation. Extra testicular haematoceles or blood collections inside the tunica vaginalis are the most common findings in the DOI: 10.14260/jemds/2021/340 scrotum after blunt injury.2 On clinical assessment, haematocele appears as a hard mass like swelling and causes pain in the scrotum. In the majority of cases, How to Cite This Article: spontaneous resolution occurs with the support of conservative therapy,3 even if Pandey S, Phatak SV, Reddy GSN, et al. Post treated conservatively, may result in infection, discomfort, or atrophy in undiagnosed traumatic hematocele - usg and broad hematoceles and testicular hematomas over time.4 elastography imaging. J Evolution Med A testis with its coverings, epididymis, and spermatic cord are all contained in Dent Sci 2021;10(21):1636-1638, DOI: 10.14260/jemds/2021/340 each hemiscrotum. -

Reaching out to People Living with HIV/AIDS in India
Spring 2006 United Nations Update Population Award Laureate Reaching Out to People Living with HIV/AIDS in India “The doctor was very loving and only 35,000 were receiving ART. patient. It’s rare to get doctors like Weak supply systems, prohibitive him. I have a lot of respect for him. costs, and lack of information He was not only my doctor, he was about HIV treatments all con- also my counselor—he helped me tribute to this treatment gap. Even disclose my status to my wife. Thanks people who receive ART face to him, I could counsel others who ongoing challenges due to side saw my side effects and were scared effects, a dearth of treatment to start ART (antiretroviral therapy).” information in local languages, —HIV-positive client and/or lack of support on how to manage treatment regimens. menting an integrated training With the second highest number The good news is that a nation- initiative that includes establish- of people living with HIV/AIDS in al effort is underway to address ing two Continuing Education the world after South Africa, India these issues. EngenderHealth’s and Training Centers (CETCs); is facing one of its biggest public India Office is part of a diverse these will serve as model training health challenges. India accounts consortium of local Indian non- centers for the consortium for nearly 10% of the 40 million governmental organizations throughout the six states. The people living with HIV/AIDS glob- (NGOs) working to improve the centers will also provide ongoing ally and more than 60% of the quality of care and support ser- training and support to providers 7.4 million such people in the vices for people taking ART. -

Infection Prevention
Infection Prevention A reference booklet for health care providers 2nd edition Infection Prevention A reference booklet for health care providers 2nd edition © 2011 EngenderHealth. All rights reserved. 440 Ninth Avenue New York, NY, 10001 U.S.A. Telephone: 212-561-8000 Fax: 212-561-8067 e-mail: [email protected] www.engenderhealth.org EngenderHealth works to improve the health and well-being of people in the poorest communities of the world. We do this by sharing our expertise in sexual and reproductive health and transforming the quality of health care. We promote gender equity, advocate for sound practices and policies, and inspire people to assert their rights to better, healthier lives. Working in partnership with local organizations, we adapt our work in response to local needs. The first edition of this publication was made possible by a grant from the Bill & Melinda Gates Foundation. EngenderHealth has taken all reasonable precautions to verify the information contained in this handbook. However, the material is provided on an “as is” basis, without warranty or condition, either expressed or implied. Responsibility for interpreting and using the information contained herein belongs to the reader alone; the publisher (EngenderHealth) is in no way liable for any loss or damage, of any kind, arising from its use. Printed in the United States of America. Printed on recycled paper. ISBN 978-1-885063-99-1 Suggested citation: EngenderHealth. 2011. Infection prevention: A reference booklet for health care providers, 2nd edition. New -

Kellie ID Emergencies.Pptx
4/24/11 ID Alert! recognizing rapidly fatal infections Susan M. Kellie, MD, MPH Professor of Medicine Division of Infectious Diseases, UNMSOM Hospital Epidemiologist UNMHSC and NMVAHCS Fever and…. Rash and altered mental status Rash Muscle pain Lymphadenopathy Hypotension Shortness of breath Recent travel Abdominal pain and diarrhea Case 1. The cross-country trucker A 30 year-old trucker driving from Oklahoma to California is hospitalized in Deming with fever and headache He is treated with broad-spectrum antibiotics, but deteriorates with obtundation, low platelet count, and a centrifugal petechial rash and is transferred to UNMH 1 4/24/11 What is your diagnosis? What is the differential diagnosis of fever and headache with petechial rash? (in the US) Tickborne rickettsioses ◦ RMSF Bacteria ◦ Neisseria meningitidis Key diagnosis in this case: “doxycycline deficiency” Key vector-borne rickettsioses treated with doxycycline: RMSF-case-fatality 5-10% ◦ Fever, nausea, vomiting, myalgia, anorexia and headache ◦ Maculopapular rash progresses to petechial after 2-4 days of fever ◦ Occasionally without rash Human granulocytotropic anaplasmosis (HGA): case-fatality<1% Human monocytotropic ehrlichiosis (HME): case fatality 2-3% 2 4/24/11 Lab clues in rickettsioses The total white blood cell (WBC) count is typicallynormal in patients with RMSF, but increased numbers of immature bands are generally observed. Thrombocytopenia, mild elevations in hepatic transaminases, and hyponatremia might be observed with RMSF whereas leukopenia -

Chapter 99 – Urological Disorders Episode Overview Urinary Tract Infections in Adults 1
Crack Cast Show Notes – Urological Disorders – August 2017 www.crackcast.org Chapter 99 – Urological Disorders Episode Overview Urinary Tract Infections in Adults 1. Differentiate between the three major causes of dysuria in women? (ddx of dysuria) 2. List 3 common UTI pathogens, and list 3 additional pathogens in complicated UTIs 3. Define uncomplicated UTI and antibiotic options 4. Define complicated UTI and antibiotic options 5. List two antibiotic options for uncomplicated and complicated pyelonephritis. 6. How is pyelonephritis managed in pregnancy? What are safe antibiotic options for bacteriuria in pregnancy? Prostatitis 1. Describe the diagnosis and management of prostatitis Renal Calculi 1. Name the areas of narrowing in the ureter 2. Name 6 risk factors for urolithiasis 3. List 8 alternative diagnoses (other than renal colic) for pain associated with urolithiasis 4. What are indications for hospitalization of patients with urolithiasis Bladder (Vesical) Calculi 1. Describe this condition and its management Acute Scrotal Pain 1. List causes of acute scrotal swelling by age groups (infant, child, adolescent, adult) 2. Describe the physiology, diagnosis and management of testicular torsion 3. Describe the treatment for sexually vs. non-sexually acquired epididymitis Acute Urinary Retention 1. Describe the physiology of urination 2. List 10 causes of acute urinary retention in adults 3. List 6 causes of urinary retention in women Hematuria 1. List causes of red-coloured urine without hematuria 2. List risk factors for urinary tract malignancy Wisecracks: 1. When is a urine culture indicated (box 89.1) 2. What is a CAUTI and how is it managed? 3. What are two medication classes of drugs for prostatic enlargement? 4. -

GERONTOLOGICAL NURSE PRACTITIONER Review and Resource M Anual
13 Male Reproductive System Disorders Vaunette Fay, PhD, RN, FNP-BC, GNP-BC GERIATRIC APPRoACH Normal Changes of Aging Male Reproductive System • Decreased testosterone level leads to increased estrogen-to-androgen ratio • Testicular atrophy • Decreased sperm motility; fertility reduced but extant • Increased incidence of gynecomastia Sexual function • Slowed arousal—increased time to achieve erection • Erection less firm, shorter lasting • Delayed ejaculation and decreased forcefulness at ejaculation • Longer interval to achieving subsequent erection Prostate • By fourth decade of life, stromal fibrous elements and glandular tissue hypertrophy, stimulated by dihydrotestosterone (DHT, the active androgen within the prostate); hyperplastic nodules enlarge in size, ultimately leading to urethral obstruction 398 GERONTOLOGICAL NURSE PRACTITIONER Review and Resource M anual Clinical Implications History • Many men are overly sensitive about complaints of the male genitourinary system; men are often not inclined to initiate discussion, seek help; important to take active role in screening with an approach that is open, trustworthy, and nonjudgmental • Sexual function remains important to many men, even at ages over 80 • Lack of an available partner, poor health, erectile dysfunction, medication adverse effects, and lack of desire are the main reasons men do not continue to have sex • Acute and chronic alcohol use can lead to impotence in men • Nocturia is reported in 66% of patients over 65 – Due to impaired ability to concentrate urine, reduced -

Assessment of Lower Urinary Tract Symptoms in Younger Men
MEN’S HEALTH ASSESSMENT OF LOWER URINARY TRACT SYMPTOMS IN YOUNGER MEN Lower urinary tract symptoms (LUTS) are common in the ageing male and represent a significant burden on both the patient and the healthcare system worldwide. 1,2 Accordingly, the majority of clinical trials and guidelines focus on the older patient, despite the fact that men below these ages will also present with many of the same symptoms. In this review, the authors explore the challenges of assessing and managing men below 50 years with LUTS. Dr Odunayo The aetiology of LUTS is multifactorial with causes How common are LUTS Kalejaiye attributed to dysfunction of the bladder and its in younger men? Urology SpR outlet – including the prostate, urethra and sphincter; The EPIC study, 3 a population-based survey which the neurological innervation of the lower urinary recruited men aged over 18 years, found that the Professor tract, and medical co-morbidities.1,2 It is important prevalence of LUTS increased with age, from 51.3% Raj Persad to consider all these aspects when assessing patients. in men aged 18-39 years to 62% in those aged 40-59 While in older men, benign prostatic enlargement years. This is compared with a prevalence of 80.7% Consultant is the commonest cause of male LUTS, in younger in men aged 60 years or older. Storage symptoms Urologist; men this is unusual, and other diagnoses should be were commonest in men 39 years or younger, with a Honorary considered more likely. prevalence of 37.5%, compared with a prevalence of Professor of 19.9% for voiding symptoms in this age group. -

Penile Fracture Anurag Chahal,1 Sahil Gupta,2 Chandan Das1
Images in… BMJ Case Reports: first published as 10.1136/bcr-2016-215385 on 13 May 2016. Downloaded from Penile fracture Anurag Chahal,1 Sahil Gupta,2 Chandan Das1 1Department of DESCRIPTION Radiodiagnosis, All India A 32-year-old man presented to our emergency Institute of Medical Sciences, New Delhi, India department, with pain, swelling and a dorsal curva- 2Department of Surgical ture in his penis. He had severe pain and lost Disciplines, All India Institute tumescence with a snapping sound during vigorous of Medical Sciences, New sexual intercourse. On examination, he had a swel- Delhi, India ling with ecchymosis on the ventral aspect of his fi Correspondence to penis causing an acute dorsal angulation ( gure 1). Dr Sahil Gupta, There was no blood at the meatus/haematuria. [email protected] Taking the typical history and examination findings Figure 3 Ultrasound images showing ventral into account, the diagnosis of penile fracture was Accepted 1 May 2016 haematoma (H) displacing the corpus spongiosum (CS), made. Ultrasound showed a focal tear in the medial and central urethra (U) displaced towards the left with wall of the right corpora cavernosa with haema- the corpora cavernosa (CC) seen dorsally. toma tracking ventrally and displacing the corpora spongiosa to the other side (figures 2 and 3). The patient was taken for emergent haematoma diagnosis is usually clinical and requires prompt evacuation and corporal repair. surgical intervention.3 Sometimes, the presentation Penile fracture occurs when an erect penis under- may be occult and the patient may present with goes a blunt trauma during sexual intercourse or pain with or without swelling. -

Case Report a Case of a Patient Who Is Diagnosed with Mild Acquired Hemophilia a After Tooth Extraction Died of Acute Subdural Hematoma Due to Head Injury
Hindawi Case Reports in Dentistry Volume 2018, Article ID 7185263, 3 pages https://doi.org/10.1155/2018/7185263 Case Report A Case of a Patient Who Is Diagnosed with Mild Acquired Hemophilia A after Tooth Extraction Died of Acute Subdural Hematoma due to Head Injury Tomohisa Kitamura,1 Tsuyoshi Sato ,1 Eiji Ikami,1 Yosuke Fukushima,1 and Tetsuya Yoda2 1Department of Oral and Maxillofacial Surgery, Saitama Medical University, 38 Moro-hongou, Moroyama-machi, Iruma-gun, Saitama 350-0495, Japan 2Department of Maxillofacial Surgery, Tokyo Medical and Dental University, Tokyo, Japan Correspondence should be addressed to Tsuyoshi Sato; [email protected] Received 13 September 2018; Revised 12 November 2018; Accepted 25 November 2018; Published 9 December 2018 Academic Editor: Yuk-Kwan Chen Copyright © 2018 Tomohisa Kitamura et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Background. Acquired hemophilia A (AHA) is a rare disorder which results from the presence of autoantibodies against blood coagulation factor VIII. The initial diagnosis is based on the detection of an isolated prolongation of the activated partial thromboplastin time (aPTT) with negative personal and family history of bleeding disorder. Definitive diagnosis is the identification of reduced FVIII levels with evidence of FVIII neutralizing activity. Case report. We report a case of a 93-year-old female who was diagnosed as AHA after tooth extraction at her home clinic. Prolongation of aPTT and a reduction in factor VIII activity levels were observed with the presence of factor VIII inhibitor. -

WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 31/05 (2006.01) A61P 31/02 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/CA20 14/000 174 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 4 March 2014 (04.03.2014) KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, (25) Filing Language: English OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (26) Publication Language: English SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, (30) Priority Data: ZW. 13/790,91 1 8 March 2013 (08.03.2013) US (84) Designated States (unless otherwise indicated, for every (71) Applicant: LABORATOIRE M2 [CA/CA]; 4005-A, rue kind of regional protection available): ARIPO (BW, GH, de la Garlock, Sherbrooke, Quebec J1L 1W9 (CA). GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, (72) Inventors: LEMIRE, Gaetan; 6505, rue de la fougere, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, Sherbrooke, Quebec JIN 3W3 (CA).