Acute Corneal Hydrops in Keratoconus Symposium
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

Diagnosing Dry Eye
MEDICAL ED NG UC UI AT A CONTINUING TIN IO CON N MEDICAL EDUCATION PUBLICATION CME ISSUE 14 Diagnosing Dry Eye ERIC D. DONNENFELD, MD Dry eye a ects tens of millions of patients and is among the most common reasons for eye care provider visits. Knowing what to look for, how, and in whom (hint: everyone) can help stem the tide of this quiet epidemic. Th e exact prevalence of dry eye is diffi cult to ascertain, for several reasons, including the absence of a single test (or universally accepted sequence of tests) for its diagnosis, and the fact that patient-reported symptoms are oft en poorly con- cordant with objective assessments.1 Estimates based on cohort studies suggest that about 5% to 35% of adults worldwide have dry eye, a rate that is expected to rise in the upcoming decades FIGURE 1 Lid margin with inspissated meibomian glands and pasty as common risk factors, including advanced age, increase.2,3 secretions indicative of MGD. Sometimes even higher estimates are cited, as dry eye symp- toms are oft en camoufl aged by other ocular surface condi- tions such as allergic conjunctivitis, surgery, and contact lens CATEGORIES AND MECHANISMS discomfort; in addition, many patients—up to 60% of those Dry eye is generally divided into two main categories based with objective evidence of dry eye—are pre-symptomatic.3 on the underlying cause: aqueous defi cient and evaporative.4 Th e landmark 2007 International Dry Eye Workshop Aqueous defi ciency describes inadequate tear production by (DEWS) report off ered the fi rst thorough expert review around the lacrimal glands. -

Role of Intracameral Dexamethasone in Preventing Immediate Postoperative Anterior Uveitis in Paediatric Cataract Extraction
ORIGINAL ARTICLE Role of Intracameral Dexamethasone in Preventing Immediate Postoperative Anterior Uveitis in Paediatric Cataract Extraction CHAUDARY NASIR AHMAD, ASAD ASLAM KHAN, ZAHID SIDDIQUE, SHAKIL AHMED ABSTRACT Objective: Paediatric cataract surgery can result in several complications like post operative inflammation. Topical steroids are relied upon as mainstay of treatment and prevention, adjuvant periocular and systemic steroids may be required to control the inflammation. The purpose of study was to evaluate the role of intracameral dexamethasone in preventing immediate postoperative anterior uveitis in paediatric cataract extraction. Methods: This was comparative study done at institute of Ophthalmology Mayo Hospital Lahore. Sixty patients were selected and divided into two equal groups. Group I were given routinely subconjuctival injection of gentamycin 20 mg and dexamethasone 2 mg while patients in group II were given subconjuctival injection of gentamycin 20 mg and intracameral dexamethasone 0.4 mg (0.1ml). Evaluation was done on 1st and 3rd postoperative day and on first follow up visit. Examination of children was done with help of slit lamp for cells, flare or any other sign of inflammation. In case of non cooperative children examination was done with microscope under sedation/general anesthesia for fibrinous reaction, exudative membrane, posterior synechiae and red reflex. Results: There were total of sixty patients age below 12 years divided into two equal groups, 43 were males and 17were females. Group I was given routinely subconjuctival injection of dexamethasone, while group II patients were given intracameral injection of dexamethasone. Group II patients showed better results than that of group I. Conclusion: Intracameral injection of dexamethasone was found superior to subconjuctival injection of dexamethasone in preventing immediate postoperative anterior uveitis. -

Intracameral Therapeutics for Cataract Surgery
s THE LITERATURE INTRACAMERAL THERAPEUTICS FOR CATARACT SURGERY Closing in on no-drop surgery. BY MARK A. KONTOS, MD; AND KENDALL E. DONALDSON, MD, MS DEXAMETHASONE INTRACAMERAL ninety-four patients scheduled for Anterior chamber cell clearing at DRUG-DELIVERY SUSPENSION FOR cataract surgery at 27 sites were day 8 was achieved in 25% of eyes INFLAMMATION ASSOCIATED WITH randomly assigned to three groups. in group 1, 63% in group 2, and CATARACT SURGERY: A RANDOMIZED, Group 1 received a 5-µL injection of 66% in group 3 (P > .001). Anterior PLACEBO-CONTROLLED PHASE III TRIAL placebo. Groups 2 and 3, respectively, chamber flare clearing at day 8 was received a 5-µL injection of 342 µg or achieved in 63.8% of eyes in group 1, Donnenfeld E, Holland E1 517 µg dexamethasone drug delivery 92.4% in group 2, and 89.1% in group suspension into the anterior chamber 3 (P > .001). Adverse events were ABSTRACT SUMMARY at the conclusion of cataract surgery. similar among the three groups with In this randomized, double-masked, Patients were observed for 90 days no serious adverse events reported up placebo-controlled study, inves- after surgery. to postoperative day 90. tigators sought to determine the The primary outcome measure safety and efficacy of dexamethasone was anterior chamber cell clearing DISCUSSION intraocular suspension 9% (Dexycu, at postoperative day 8. Secondary The appropriate postoperative EyePoint Pharmaceuticals) for measures were anterior chamber flare medical regimen for cataract surgery intracameral administration in and anterior chamber cell plus flare remains a hotly debated subject. The two dosages in patients undergoing clearing in the study eyes. -

Intracameral Antibiotics for the Prevention of Endophthalmitis Post-Cataract Surgery: Review of Clinical and Cost-Effectiveness and Guidelines
Canadian Agency for Agence canadienne Drugs and Technologies des médicaments et des in Health technologies de la santé Rapid Response Report: Peer-Reviewed Summary with Critical Appraisal CADTH Intracameral Antibiotics for the Prevention of Endophthalmitis Post-Cataract Surgery: Review of Clinical and Cost-Effectiveness and Guidelines October 2010 Supporting Informed Decisions Until April 2006, the Canadian Agency for Drugs and Technologies in Health (CADTH) was known as the Canadian Coordinating Office for Health Technology Assessment (CCOHTA). Publications can be requested from: CADTH 600-865 Carling Avenue Ottawa ON Canada K1S 5S8 Tel.: 613-226-2553 Fax: 613-226-5392 Email: [email protected] or downloaded from CADTH’s website: http://www.cadth.ca Cite as: Ndegwa S, Cimon K, Severn M. Intracameral Antibiotics for the Prevention of Endophthalmitis Post-Cataract Surgery: Review of Clinical and Cost-Effectiveness and Guideline [Internet]. Ottawa: Canadian Agency for Drugs and Technologies in Health; 2010 (Rapid Response Report: Peer-Reviewed Summary with Critical Appraisal). [cited 2010-10-07]. Available from: http://www.cadth.ca/index.php/en/hta/reports-publications/search/publication/2683 Production of this report is made possible by financial contributions from Health Canada and the governments of Alberta, British Columbia, Manitoba, New Brunswick, Newfoundland and Labrador, Northwest Territories, Nova Scotia, Nunavut, Prince Edward Island, Saskatchewan, and Yukon. The Canadian Agency for Drugs and Technologies in Health takes sole responsibility for the final form and content of this report. The views expressed herein do not necessarily represent the views of Health Canada, or any provincial or territorial government. Reproduction of this document for non-commercial purposes is permitted provided appropriate credit is given to CADTH. -

How to Address Dry Eye in the Challenging Cornea Understand Dry Eye’S Various Factors and Causes to Get Ahead of the Treatment Curve
MARCH 2021 | 16 Ocular Surface Disease How to address dry eye in the challenging cornea Understand dry eye’s various factors and causes to get ahead of the treatment curve By Seema Nanda, OD Levels of severity y eyes are getting watery after log- For everyone who has been stuck at home binge ging off my tenth Zoom meeting watching Netflix, you know exactly what it feels this week, which makes me think like to have dry eyes. For the sake of simplic- of the others Zooming away and ity, dry eye symptoms can be reduced to the Mexperiencing dry eye symptoms. As an optom- levels of mild, moderate, or severe. etrist who sees corneal calamities on a contin- For mild cases, preservative-free artificial ual basis, it can become a challenge to treat. tears, such as Refresh Relieva (Allergan) and At first, clinicians may Retaine MGD (OCuSOFT), are excellent options. diagnose dry eye dis- Refresh Relieva contains an inactive ingredi- ease (DED) by observing ent, hyaluronic acid, that I have personally and simple superficial punc- anecdotally found to soothe the corneal sur- tate keratitis at the slit face. For moderate conditions, twice-daily use of lamp. However, compli- Retaine MGD drops combined with a clinically cations may ensue, such validated nutritional supplement can provide as recurrent epithelial ero- relief to the deficient lipid profile. For severe sions or persistent epithe- symptoms, additional therapies should be imple- SEEMA NANDA, lial defects, causing more mented to maintain the corneal integrity. OD, is in practice in Houston, Texas. problems. These chal- lenges could lead to neu- Use a supplement rotrophic ulcers and become even more difficult A supplement such as HydroEye (ScienceBased to handle. -

Management of Acute Corneal Hydrops Secondary to Keratoconus by Descemetopexy Using Intracameral
NUJHS Vol. I, No.4, December 2011, ISSN 2249-7110 Nitte University Journal of Health Science Case Report MANAGEMENT OF ACUTE CORNEAL HYDROPS SECONDARY TO KERATOCONUS BY DESCEMETOPEXY USING INTRACAMERAL PERFLUOROPROPANE (C3F8) – A CASE REPORT Vijay Pai 1, Jayaram Shetty 2, Hrishikesh Amin 3, S. Bhat 4, Divya Lakshmi 5 1 Professor, 2 Prof.& Head, 3 Professor, 4 Assoc. Professor, 5 Sr. Resident, Dept. of Ophthalmology, K.S. Hegde Medical Academy, Deralakatte, Mangalore - 575 018. Correspondence: Vijay Pai, Professor, Dept. of Ophthalmology, K.S. Hegde Medical Academy, Deralakatte, Mangalore – 575018. E-mail : [email protected], [email protected] Abstract : Keratoconus is a clinical term used to describe bilateral non-inflammatory corneal ectasia in its axial part due to which cornea assumes a conical shape1. The onset of keratoconus is generally at the age of puberty, and progresses over a period of 10-20 years2,3. The treatment of Keratoconus is rarely an emergency, with the exception of corneal hydrops resulting from rupture of the Descemet's membrane. This may be the common mode of presentation in patients with associated developmental delay, probably related to habitual ocular massage4,5. Keywords : Keratoconus, acute hydrops, descemetopexy, C3F8 Case Report : Descemetopexy under intravenous sedation, after A 21 year old girl presented to the cornea services of Justice obtaining an informed consent. Preoperatively, the pupil K.S. Hegde Charitable Hospital, Mangalore with complaints was constricted using 2% Pilocarpine eye drops, 1 drop of sudden decrease in vision in the right eye since one every 15 min, 1 hour prior to the surgery, not only to avoid week. -

A Survey of Measures Used for the Prevention of Postoperative
Eye (2008) 22, 620–627 & 2008 Nature Publishing Group All rights reserved 0950-222X/08 $30.00 www.nature.com/eye CLINICAL STUDY A survey of P Gordon-Bennett, A Karas, D Flanagan, C Stephenson and M Hingorani measures used for the prevention of postoperative endophthalmitis after cataract surgery in the United Kingdom Abstract used a neomycin eyedrop for postoperative prophylaxis. Purpose This study investigates the current Eye (2008) 22, 620–627; doi:10.1038/sj.eye.6702675; practice of United Kingdom (UK) published online 15 December 2006 ophthalmologists in perioperative antibiotic and antiseptic use in cataract surgery. Keywords: antibiotic; cataract surgery; Materials and methods A telephone postoperative endophthalmitis; prevention; interview survey was conducted with prophylaxis ophthalmic staff at all ophthalmic training units in the UK in October and November 2005. Results The practices of a total of 800 Introduction Department of consultants were ascertained. Preoperatively, Ophthalmology, 795 (99.4%) surgeons used povidone-iodine to There is widespread variation in the prophylactic measures used to prevent Hinchingbrooke Hospital, prepare the skin. In all, 558 (69.8%) instilled Huntingdon, endophthalmitis following cataract surgery1 but 5 or 10% povidone-iodine in the conjunctival Cambridgeshire, UK in the light of rising endophthalmitis incidence sac; 47 (5.9%) gave preoperative antibiotic rates2,3 and new scientific evidence, a eyedrops. Intraoperatively, intracameral Correspondence: P Gordon- reassessment of methods is required. Although Bennett, antibiotics were given either as a bolus rare, endophthalmitis carries a devastating Department of [80 (10.0%) intracameral cefuroxime, 29 (3.6%) Ophthalmology, prognosis, with only 33% of patients achieving intracameral vancomycin] or in the irrigating Hinchingbrooke Hospital, visual acuity better than 6/12.4 Establishing Huntingdon, fluid [33 (4.1%) vancomycin]. -

Intracameral Versus Sub-Conjunctival Dexamethasone Injection for Postoperative Inflammation in Congenital Cataract Surgery
Original Article Intracameral Versus Sub-conjunctival Dexamethasone Injection for Postoperative Inflammation in Congenital Cataract Surgery Afia Matloob Rana, Ali Raza, Waseem Akhter Pak J Ophthalmol 2019, Vol. 35, No. 3 . .. .. See end of article for Purpose: To compare the effect of intracameral with sub-conjunctival injection of authors affiliations dexamethasone in preventing immediate postoperative inflammation after congenital cataract extraction. …..……………………….. Study Design: Randomized control trial. Correspondence to: Afia Matloob Rana Place and Duration of Study: Holy Family Hospital, Rawalpindi from June 2014 Assistant Professor to May 2015. Ophthalmology Department Material and Methods: All Pediatric patients less than 15 years of age and of HBS General Hospital, Islamabad both genders, undergoing cataract surgery in Holy Family Hospital, were Email: [email protected] included in the study using a random table. Using standardized sample size calculator and statistical assumption with 95% CI and 5% alpha error, the study sample was 95 cases in each group. Group A patients got intracameral injection of dexamethasone while Group B patients got subconjunctival injection of dexamethasone. The outcome measure was intraocular inflammation after cataract surgery. Examination was done within first three postoperative days for signs of anterior chamber inflammation. Standard slit lamp or hand held slit lamp was used for this purpose. Results: One hundred and ninety patients were included in the study. The patients were equally divided into 2 groups. Male cases were in majority in group B (58.9%) whereas in group A females (55.8%) were in majority. Mean age was 6.43 ± 4.69 years in Group-A compared to 5.85 ± 4.10 years in Group-B. -

Management of Acute Corneal Hydrops Secondary to Keratoconus by Descemetopexy Using Intracameral
Published online: 2020-05-04 NUJHS Vol. I, No.4, December 2011, ISSN 2249-7110 Nitte University Journal of Health Science Case Report MANAGEMENT OF ACUTE CORNEAL HYDROPS SECONDARY TO KERATOCONUS BY DESCEMETOPEXY USING INTRACAMERAL PERFLUOROPROPANE (C3F8) – A CASE REPORT Vijay Pai 1, Jayaram Shetty 2, Hrishikesh Amin 3, S. Bhat 4, Divya Lakshmi 5 1 Professor, 2 Prof.& Head, 3 Professor, 4 Assoc. Professor, 5 Sr. Resident, Dept. of Ophthalmology, K.S. Hegde Medical Academy, Deralakatte, Mangalore - 575 018. Correspondence: Vijay Pai, Professor, Dept. of Ophthalmology, K.S. Hegde Medical Academy, Deralakatte, Mangalore – 575018. E-mail : [email protected], [email protected] Abstract : Keratoconus is a clinical term used to describe bilateral non-inflammatory corneal ectasia in its axial part due to which cornea assumes a conical shape1. The onset of keratoconus is generally at the age of puberty, and progresses over a period of 10-20 years2,3. The treatment of Keratoconus is rarely an emergency, with the exception of corneal hydrops resulting from rupture of the Descemet's membrane. This may be the common mode of presentation in patients with associated developmental delay, probably related to habitual ocular massage4,5. Keywords : Keratoconus, acute hydrops, descemetopexy, C3F8 Case Report : Descemetopexy under intravenous sedation, after A 21 year old girl presented to the cornea services of Justice obtaining an informed consent. Preoperatively, the pupil K.S. Hegde Charitable Hospital, Mangalore with complaints was constricted using 2% Pilocarpine eye drops, 1 drop of sudden decrease in vision in the right eye since one every 15 min, 1 hour prior to the surgery, not only to avoid week. -
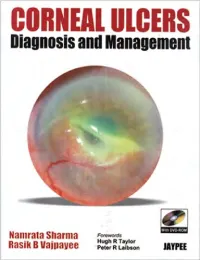
CORNEAL ULCERS Diagnosis and Management
CORNEAL ULCERS Diagnosis and Management System requirement: • Windows XP or above • Power DVD player (Software) • Windows Media Player 10.0 version or above • Quick time player version 6.5 or above Accompanying DVD ROM is playable only in Computer and not in DVD player. Kindly wait for few seconds for DVD to autorun. If it does not autorun then please do the following: • Click on my computer • Click the drive labelled JAYPEE and after opening the drive, kindly double click the file Jaypee CORNEAL ULCERS Diagnosis and Management Namrata Sharma MD DNB MNAMS Associate Professor of Ophthalmology Cornea, Cataract and Refractive Surgery Services Dr. Rajendra Prasad Centre for Ophthalmic Sciences All India Institute of Medical Sciences, New Delhi India Rasik B Vajpayee MS FRCSEd FRANZCO Head, Corneal and Cataract Surgery Centre for Eye Research Australia Royal Victorian Eye and Ear Hospital University of Melbourne Australia Forewords Hugh R Taylor Peter R Laibson ® JAYPEE BROTHERS MEDICAL PUBLISHERS (P) LTD New Delhi • Ahmedabad • Bengaluru • Chennai • Hyderabad • Kochi • Kolkata • Lucknow • Mumbai • Nagpur Published by Jitendar P Vij Jaypee Brothers Medical Publishers (P) Ltd B-3 EMCA House, 23/23B Ansari Road, Daryaganj New Delhi 110 002, India Phones: +91-11-23272143, +91-11-23272703, +91-11-23282021, +91-11-23245672 Rel: +91-11-32558559, Fax: +91-11-23276490, +91-11-23245683 e-mail: [email protected] Visit our website: www.jaypeebrothers.com Branches • 2/B, Akruti Society, Jodhpur Gam Road Satellite Ahmedabad 380 015, Phones: +91-79-26926233, -

Effect of Intracameral Triamcinolone Acetonide on Postoperative
Eye (2010) 24, 619–623 & 2010 Macmillan Publishers Limited All rights reserved 0950-222X/10 $32.00 www.nature.com/eye Effect of A Karalezli, M Borazan, C Kucukerdonmez, CLINICAL STUDY A Akman and YA Akova intracameral triamcinolone acetonide on postoperative intraocular pressure after cataract surgery Abstract Conclusion Intracameral injection of 1 mg TA after uncomplicated phacoemulsification Purpose To evaluate the effect of 1 mg surgery had no significant effects on intracameral triamcinolone acetonide (TA) postoperative IOP. on postoperative intraocular pressure (IOP) Eye (2010) 24, 619–623; doi:10.1038/eye.2009.182; after routine cataract surgery. published online 10 July 2009 Patients and methods This prospective, randomized, placebo-controlled study Keywords: intraocular pressure; comprised 120 eyes of 120 patients with phacoemulsification; postoperative uncomplicated cataract surgery. The patients inflammation; triamcinolone acetonide; visual were randomized into two groups. Eyes in acuity group 1 (60 eyes) received an injection of 1 mg TA into the anterior chamber at the end of the surgery, but eyes in group 2 (60 eyes) Introduction Department of did not. The biomicroscopic evaluation, Ophthalmology, Baskent visual acuity (VA), and IOP measurements Recent advances in cataract surgery, such as University School of were done at baseline (preoperatively) and techniques, instrumentation, and foldable Medicine, Ankara, Selcuklu, 6, 20–24 h, 1 week, and permonthly until intraocular lenses (IOLs), have resulted in a Konya, Turkey 6 months postoperatively. decrease in the physical trauma associated with Correspondence: Results Mean IOP at 6 and 20–24 h the surgery. Nevertheless, most patients still A Karalezli, Department of postoperatively were significantly higher exhibit postoperative ocular inflammation Ophthalmology, Baskent than baseline measurements in both groups after cataract surgery.1 Universitesi Tip Fakultesi, (Po0.001). -

DURYSTA (Bimatoprost Implant) Administration in Pregnant Women to Inform a Drug Associated Risk
NDA 211911 Page: 4 HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all the information ------------WARNINGS AND PRECAUTIONS----------- needed to use DURYSTATM safely and effectively. See Endothelial cell loss: Due to possible corneal full prescribing information for DURYSTATM. endothelial cell loss, administration of DURYSTA should be limited to a single implant per eye without DURYSTATM (bimatoprost implant), for intracameral retreatment. (5.1) administration Corneal Adverse Reactions: DURYSTA has been Initial U.S. Approval: 2001 associated with corneal adverse reactions and risks are increased with multiple implants. Use caution in ---------------INDICATIONS AND USAGE---------------- patients with limited corneal endothelial cell reserve. DURYSTATM is a prostaglandin analog indicated for the (5.1) reduction of intraocular pressure (IOP) in patients with Iridocorneal Angle: DURYSTA should be used with open angle glaucoma (OAG) or ocular hypertension caution in patients with narrow angles or anatomical (OHT). (1) angle obstruction. (5.2) ------------DOSAGE AND ADMINISTRATION---------- ------------------ADVERSE REACTIONS------------------- For ophthalmic intracameral administration. (2.1) In controlled studies, the most common ocular adverse The intracameral administration should be carried out reaction reported by 27% of patients was conjunctival under standard aseptic conditions. (2.2) hyperemia. Other common adverse reactions reported in 5-10% of patients were foreign body sensation, eye pain, -----------DOSAGE