Management of Acute Corneal Hydrops in a Patient with Keratoconus: a Teaching Case Report | 1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Intraoperative Optical Coherence Tomography Imaging in Corneal Surgery: a Literature Review and Proposal of Novel Applications
Hindawi Journal of Ophthalmology Volume 2020, Article ID 1497089, 10 pages https://doi.org/10.1155/2020/1497089 Research Article Intraoperative Optical Coherence Tomography Imaging in Corneal Surgery: A Literature Review and Proposal of Novel Applications Hiroshi Eguchi ,1 Fumika Hotta,1 Shunji Kusaka,1 and Yoshikazu Shimomura2 1Department of Ophthalmology, Kindai University, Faculty of Medicine, 377-2 Ohnohigashi, Osakasayama, Osaka 589-8511, Japan 2Department of Ophthalmology, Fuchu Eye Center, 1-10-17 Hiko-cho, Izumi, Osaka 594-0076, Japan Correspondence should be addressed to Hiroshi Eguchi; [email protected] Received 26 June 2020; Revised 12 August 2020; Accepted 21 August 2020; Published 11 September 2020 Academic Editor: Sang Beom Han Copyright © 2020 Hiroshi Eguchi et al. &is is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Intraoperative optical coherence tomography (iOCT) is widely used in ophthalmic surgeries for cross-sectional imaging of ocular tissues. &e greatest advantage of iOCTis its adjunct diagnostic efficacy, which facilitates to decision-making during surgery. Since the development of microscopic-integrated iOCT (MIOCT), it has been widely used mainly for vitreoretinal and anterior segment surgeries. In corneal transplantation, MIOCT allows surgeons to visualise structure underneath the turbid and distorted cornea, which are impossible to visualise with a usual microscope. Real-time visualisation of hard-to-see area reduces the operation time and leads to favorable surgical outcomes. &e use of MIOCT is advantageous for a variety of corneal surgical procedures. Here, we have reviewed articles focusing on the utility of iOCT and MIOCTin penetrating keratoplasty, deep anterior lamellar keratoplasty, Descemet stripping automated endothelial keratoplasty, and Descemet membrane endothelial keratoplasty. -
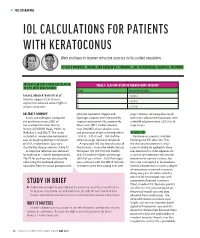
Iol Calculations for Patients with Keratoconus
s THE LITERATURE IOL CALCULATIONS FOR PATIENTS WITH KERATOCONUS Work continues to improve refractive accuracy in this patient population. BY ALICE ROTHWELL, MBCHB, AND ANDREW M.J. TURNBULL, BM, PGCERTMEDED, PGDIPCRS, FRCOPHTH INTRAOCULAR LENS POWER CALCULATION TABLE 1. CLASSIFICATION OF KERATOCONUS SEVERITY IN EYES WITH KERATOCONUS Stage Keratometry Reading Savini G, Abbate R, Hoffer KJ, et al1 1 ≤ 48.00 D Industry support: K.J.H. licenses 2 > 48.00 D registered trademark name Hoffer to various companies 3 > 53.00 D ABSTRACT SUMMARY spherical equivalent. Myopic and stage 1 disease. Accuracy decreased Savini and colleagues compared hyperopic surprises were indicated by with more advanced keratoconus, with the prediction errors (PEs) of negative and positive PEs, respectively. a MedAE of greater than 2.50 D in all five standard formulas: Barrett Mean error (ME), median absolute stage 3 eyes. Universal II (BUII), Haigis, Hoffer Q, error (MedAE), mean absolute error, Holladay 1, and SRK/T. The study and percentage of eyes achieving within DISCUSSION included 41 consecutive keratoconic ±0.50 D, ±0.75 D, and ±1.00 D of the Keratoconus presents multiple eyes undergoing phacoemulsification refractive target were also calculated. challenges to IOL selection. First, and IOL implantation. Eyes were A hyperopic ME was found across all the standard keratometric index classified by disease severity (Table 1). five formulas. Across the whole dataset, cannot reliably be applied to these A subjective refraction was obtained the lowest ME (0.91 D) and MedAE eyes because this index depends on for each eye at 1 month postoperatively. (0.62 D) and the highest percentage a normal ratio between the anterior The PE for each eye was calculated by (36%) of eyes within ±0.50 D of target and posterior corneal surfaces, but subtracting the predicted spherical were achieved with the SRK/T formula. -

Diagnosing Dry Eye
MEDICAL ED NG UC UI AT A CONTINUING TIN IO CON N MEDICAL EDUCATION PUBLICATION CME ISSUE 14 Diagnosing Dry Eye ERIC D. DONNENFELD, MD Dry eye a ects tens of millions of patients and is among the most common reasons for eye care provider visits. Knowing what to look for, how, and in whom (hint: everyone) can help stem the tide of this quiet epidemic. Th e exact prevalence of dry eye is diffi cult to ascertain, for several reasons, including the absence of a single test (or universally accepted sequence of tests) for its diagnosis, and the fact that patient-reported symptoms are oft en poorly con- cordant with objective assessments.1 Estimates based on cohort studies suggest that about 5% to 35% of adults worldwide have dry eye, a rate that is expected to rise in the upcoming decades FIGURE 1 Lid margin with inspissated meibomian glands and pasty as common risk factors, including advanced age, increase.2,3 secretions indicative of MGD. Sometimes even higher estimates are cited, as dry eye symp- toms are oft en camoufl aged by other ocular surface condi- tions such as allergic conjunctivitis, surgery, and contact lens CATEGORIES AND MECHANISMS discomfort; in addition, many patients—up to 60% of those Dry eye is generally divided into two main categories based with objective evidence of dry eye—are pre-symptomatic.3 on the underlying cause: aqueous defi cient and evaporative.4 Th e landmark 2007 International Dry Eye Workshop Aqueous defi ciency describes inadequate tear production by (DEWS) report off ered the fi rst thorough expert review around the lacrimal glands. -

Role of Intracameral Dexamethasone in Preventing Immediate Postoperative Anterior Uveitis in Paediatric Cataract Extraction
ORIGINAL ARTICLE Role of Intracameral Dexamethasone in Preventing Immediate Postoperative Anterior Uveitis in Paediatric Cataract Extraction CHAUDARY NASIR AHMAD, ASAD ASLAM KHAN, ZAHID SIDDIQUE, SHAKIL AHMED ABSTRACT Objective: Paediatric cataract surgery can result in several complications like post operative inflammation. Topical steroids are relied upon as mainstay of treatment and prevention, adjuvant periocular and systemic steroids may be required to control the inflammation. The purpose of study was to evaluate the role of intracameral dexamethasone in preventing immediate postoperative anterior uveitis in paediatric cataract extraction. Methods: This was comparative study done at institute of Ophthalmology Mayo Hospital Lahore. Sixty patients were selected and divided into two equal groups. Group I were given routinely subconjuctival injection of gentamycin 20 mg and dexamethasone 2 mg while patients in group II were given subconjuctival injection of gentamycin 20 mg and intracameral dexamethasone 0.4 mg (0.1ml). Evaluation was done on 1st and 3rd postoperative day and on first follow up visit. Examination of children was done with help of slit lamp for cells, flare or any other sign of inflammation. In case of non cooperative children examination was done with microscope under sedation/general anesthesia for fibrinous reaction, exudative membrane, posterior synechiae and red reflex. Results: There were total of sixty patients age below 12 years divided into two equal groups, 43 were males and 17were females. Group I was given routinely subconjuctival injection of dexamethasone, while group II patients were given intracameral injection of dexamethasone. Group II patients showed better results than that of group I. Conclusion: Intracameral injection of dexamethasone was found superior to subconjuctival injection of dexamethasone in preventing immediate postoperative anterior uveitis. -

Olivia Steinberg ICO Primary Care/Ocular Disease Resident American Academy of Optometry Residents Day Submission
Olivia Steinberg ICO Primary Care/Ocular Disease Resident American Academy of Optometry Residents Day Submission The use of oral doxycycline and vitamin C in the management of acute corneal hydrops: a case comparison Abstract- We compare two patients presenting to clinic with an uncommon complication of keratoconus, acute corneal hydrops. Management of the patients differs. One heals quickly, while the other has a delayed course to resolution. I. Case A a. Demographics: 40 yo AAM b. Case History i. CC: red eye, tearing, decreased VA x 1 day OS ii. POHx: (+) keratoconus OU iii. PMHx: depression, anxiety, asthma iv. Meds: Albuterol, Ziprasidone v. Scleral CL wearer for approximately 6 months OU vi. Denies any pain OS, denies previous occurrence OU, no complaints OD c. Pertinent Findings i. VA cc (CL’s)- 20/25 OD, 20/200 PH 20/60+2 OS ii. Slit Lamp 1. Inferior corneal thinning and Fleisher ring OD, central scarring OD, 2+ diffuse microcystic edema OS, Descemet’s break OS (photos and anterior segment OCT) 2. 2+ diffuse injection OS 3. D&Q A/C OU iii. Intraocular Pressures: deferred OD due to CL, 9mmHg OS (tonopen) iv. Fundus Exam- unremarkable OU II. Case B a. Demographics: 39 yo AAM b. Case History i. CC: painful, red eye, tearing, decreased VA x 1 day OS ii. POHx: unremarkable iii. PMHx: hypertension iv. Meds: unknown HTN medication v. Wears Soflens toric CL’s OU; reports previous doctor had difficulty achieving proper fit OU; denies diagnosis of keratoconus OU vi. Denies any injury OS, denies previous occurrence OU, no complaints OD c. -

Analysis of Human Corneal Igg by Isoelectric Focusing
Investigative Ophthalmology & Visual Science, Vol. 29, No. 10, October 1988 Copyright © Association for Research in Vision and Ophthalmology Analysis of Human Corneal IgG by Isoelectric Focusing J. Clifford Woldrep,* Robin L. Noe,f and R. Doyle Stulringf Parameters which regulate the localization and retention of IgG within the corneal stroma are complex and poorly understood. Although multiple factors are involved, electrostatic interactions between IgG and anionic corneal tissue components, ie, proteoglycans (PG) and glycosaminoglycans (GAG) may regulate the distribution of antibodies within the corneal stroma. Isoelectric focusing (IEF) and blotting analysis of IgG revealed a restricted pi profile for both central and peripheral regions of the normal cornea. Similar analysis of pathological corneas from keratoplasty specimens in Fuchs' dys- trophy and keratoconus reveal a variable IEF profile. In the majority of keratoplasty specimens from patients with corneal edema or graft rejection, there was generally little or no IgG detectable. These results suggest that in edematous corneas where there is altered PG/GAG in the stroma and modified fluid dynamics, there is a concomitant loss of IgG. These findings may have implications for immuno- logic surveillance and protection of the avascular cornea. Invest Ophthalmol Vis Sci 29:1538-1543, 1988 The humoral immune system plays an important the soluble plasma proteins through ionic interac- role in mediating immunologic surveillance and pro- tions. The PGs and GAGs have long been known to -

Intracameral Therapeutics for Cataract Surgery
s THE LITERATURE INTRACAMERAL THERAPEUTICS FOR CATARACT SURGERY Closing in on no-drop surgery. BY MARK A. KONTOS, MD; AND KENDALL E. DONALDSON, MD, MS DEXAMETHASONE INTRACAMERAL ninety-four patients scheduled for Anterior chamber cell clearing at DRUG-DELIVERY SUSPENSION FOR cataract surgery at 27 sites were day 8 was achieved in 25% of eyes INFLAMMATION ASSOCIATED WITH randomly assigned to three groups. in group 1, 63% in group 2, and CATARACT SURGERY: A RANDOMIZED, Group 1 received a 5-µL injection of 66% in group 3 (P > .001). Anterior PLACEBO-CONTROLLED PHASE III TRIAL placebo. Groups 2 and 3, respectively, chamber flare clearing at day 8 was received a 5-µL injection of 342 µg or achieved in 63.8% of eyes in group 1, Donnenfeld E, Holland E1 517 µg dexamethasone drug delivery 92.4% in group 2, and 89.1% in group suspension into the anterior chamber 3 (P > .001). Adverse events were ABSTRACT SUMMARY at the conclusion of cataract surgery. similar among the three groups with In this randomized, double-masked, Patients were observed for 90 days no serious adverse events reported up placebo-controlled study, inves- after surgery. to postoperative day 90. tigators sought to determine the The primary outcome measure safety and efficacy of dexamethasone was anterior chamber cell clearing DISCUSSION intraocular suspension 9% (Dexycu, at postoperative day 8. Secondary The appropriate postoperative EyePoint Pharmaceuticals) for measures were anterior chamber flare medical regimen for cataract surgery intracameral administration in and anterior chamber cell plus flare remains a hotly debated subject. The two dosages in patients undergoing clearing in the study eyes. -
Management Modalities for Keratoconus an Overview of Noninterventional and Interventional Treatments
REFRACTIVE SURGERY FEATURE STORY EXCLUSIVE ONLINE CONTENT AVAILABLE Management Modalities for Keratoconus An overview of noninterventional and interventional treatments. BY MAZEN M. SINJAB, MD, PHD anagement of keratoconus has advanced TAKE-HOME MESSAGE during the past few years, and surgeons can • When evaluating patients with keratoconus, ask now choose among numerous traditional and them to stop using RGP contact lenses at least 2 modern treatments. Traditional modalities weeks before evaluation to achieve correct Msuch as spectacle correction, contact lenses, penetrating measurement of the corneal shape. keratoplasty (PKP), and conductive keratoplasty (CK) • Interventional management modalities include CK, are still effective; however, demand for the last two has PKP, DALK, ICRSs, CXL, phakic IOLs, or some decreased with the advent of modern alternatives, specifi- combination of these treatments. cally intrastromal corneal ring segments (ICRSs) and cor- • Making the right management decision depends neal collagen crosslinking (CXL). Caution should be used on the patient’s corneal transparency and stress when considering these newer treatment modalities, and lines, age, progression, contact lens tolerance, surgeons should be aware of their indications, contraindi- refractive error, UCVA and BCVA, K-max, corneal cations, conditions, and complications before proceeding thickness, and sex. with treatment. Keratoconus treatments can be divided into two cate- Some patients achieve good vision correction and comfort gories, interventional and noninterventional. In this article, with this strategy. particular attention is given to ICRSs and CXL, as they are Advances in lens designs and materials have increased the the most popular emerging interventional management proportion of keratoconus patients who can be fitted with modalities for keratoconus. -

Painless Presentation of Acute Hydrops in Keratoconus with Serial In-Vivo Imaging
Painless Presentation of Acute Hydrops in Keratoconus with Serial In-vivo Imaging Sara Berke-Silva, O.D. and Kimberly Reed, O.D. Nova Southeastern University Abstract Acute corneal hydrops is typically associated with acute pain, photophobia, and tearing at onset, but our patient denied these symptoms. The poster will present this case and review current diagnostic and therapeutic strategies, including controversies. I. Case History a. 21 year old Hispanic female b. The patient woke up 3 hours prior to examination with an acute onset of a ‘white spot’ and reduced vision OD. Denies pain, photophobia, tearing. c. After further questioning, the patient reported foreign body sensation OU that was unchanged from the normal amount she experiences without her contact lenses. d. Diagnosed with Keratoconus at age 15. Wore corneal RGPs until two years ago when semi-scleral lenses were employed with excellent visual outcomes. II. Pertinent Findings a. The patient was not photophobic and denied pain throughout the exam. Increased lacrimation was evident, unbeknownst to the patient. b. Slit lamp examination revealed significant corneal edema centrally with an absence of an anterior chamber reaction. Epithelial bullae were present. c. OCT confirmed posterior corneal compromise and significant corneal edema throughout all layers, with several bullae and microcysts in the epithelium. III. Differential Diagnosis a. Hydrops b. Corneal abrasion caused by contact lens wear c. Corneal edema caused by contact lens overwear d. Corneal infection causing ulceration e. Acute, severe corneal edema due to other cause of endothelial failure IV. Diagnosis and Discussion a. Acute corneal hydrops in the context of keratoconus has typically been associated with pain, photophobia, and tearing at onset (1,2,3), but our patient denied having these symptoms. -

Acute Keratoconus-Like Corneal Hydrops Secondary to Ocular
perim Ex en l & ta a l ic O p in l h Journal of Clinical & Experimental t C h f a o l m l a o Ke et al., J Clin Exp Ophthalmol 2017, 8:6 n l o r g u y o Ophthalmology J DOI: 10.4172/2155-9570.1000694 ISSN: 2155-9570 Case Report Open Access Acute Keratoconus-Like Corneal Hydrops Secondary to Ocular Massage Following Trabeculectomy Hongmin Ke, Chengguo Zuo and Mingkai Lin* State Key Laboratory of Ophthalmology, Zhongshan Ophthalmic Center, Sun Yat-sen University, 54 Xianlie Nan Road, Guangzhou, China *Corresponding author: Mingkai Lin, State Key Laboratory of Ophthalmology, Zhongshan Ophthalmic Center, 54 Xianlie Nan Road, Guangzhou, China, 510060, E- mail: [email protected] Received date: November 13, 2017; Accepted date: November 21, 2017; Published date: November 23, 2017 Copyright: © 2017 Ke H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Purpose: To report a case of acute keratoconus-like corneal hydrops in a patient with long-term ocular massage following trabeculectomy. Methods: Case report and review of medical literature. Results: A rare complication of acute keratoconus-like corneal hydrops occurred in a patient following the use of ocular massage to maintain satisfactory aqueous humor filtration after trabeculectomy. The patient had a history of high myopia but denied previous ocular trauma, allergic disease and a family history of keratoconus. Slit-lamp examination demonstrated keratoconus-like corneal hydrops with formation of epithelial microcystic, and intrastromal cleft. -

Scleral Lenses and Eye Health
Scleral Lenses and Eye Health Anatomy and Function of the Human Eye How Scleral Lenses Interact with the Ocular Surface Just as the skin protects the human body, the ocular surface protects the human Scleral lenses are large-diameter lenses designed to vault the cornea and rest on the conjunctival tissue sitting on eye. The ocular surface is made up of the cornea, the conjunctiva, the tear film, top of the sclera. The space between the back surface of the lens and the cornea acts as a fluid reservoir. Scleral and the glands that produce tears, oils, and mucus in the tear film. lenses can range in size from 13mm to 19mm, although larger diameter lenses may be designed for patients with more severe eye conditions. Due to their size, scleral lenses consist SCLERA: The sclera is the white outer wall of the eye. It is SCLERAL LENS made of collagen fibers that are arranged for strength rather of at least two zones: than transmission of light. OPTIC ZONE The optic zone vaults over the cornea CORNEA: The cornea is the front center portion of the outer Cross section of FLUID RESERVOIR wall of the eye. It is made of collagen fibers that are arranged in the eye shows The haptic zone rests on the conjunctiva such a way so that the cornea is clear. The cornea bends light the cornea, overlying the sclera as it enters the eye so that the light is focused on the retina. conjunctiva, and sclera as CORNEA The cornea has a protective surface layer called the epithelium. -

Intracameral Antibiotics for the Prevention of Endophthalmitis Post-Cataract Surgery: Review of Clinical and Cost-Effectiveness and Guidelines
Canadian Agency for Agence canadienne Drugs and Technologies des médicaments et des in Health technologies de la santé Rapid Response Report: Peer-Reviewed Summary with Critical Appraisal CADTH Intracameral Antibiotics for the Prevention of Endophthalmitis Post-Cataract Surgery: Review of Clinical and Cost-Effectiveness and Guidelines October 2010 Supporting Informed Decisions Until April 2006, the Canadian Agency for Drugs and Technologies in Health (CADTH) was known as the Canadian Coordinating Office for Health Technology Assessment (CCOHTA). Publications can be requested from: CADTH 600-865 Carling Avenue Ottawa ON Canada K1S 5S8 Tel.: 613-226-2553 Fax: 613-226-5392 Email: [email protected] or downloaded from CADTH’s website: http://www.cadth.ca Cite as: Ndegwa S, Cimon K, Severn M. Intracameral Antibiotics for the Prevention of Endophthalmitis Post-Cataract Surgery: Review of Clinical and Cost-Effectiveness and Guideline [Internet]. Ottawa: Canadian Agency for Drugs and Technologies in Health; 2010 (Rapid Response Report: Peer-Reviewed Summary with Critical Appraisal). [cited 2010-10-07]. Available from: http://www.cadth.ca/index.php/en/hta/reports-publications/search/publication/2683 Production of this report is made possible by financial contributions from Health Canada and the governments of Alberta, British Columbia, Manitoba, New Brunswick, Newfoundland and Labrador, Northwest Territories, Nova Scotia, Nunavut, Prince Edward Island, Saskatchewan, and Yukon. The Canadian Agency for Drugs and Technologies in Health takes sole responsibility for the final form and content of this report. The views expressed herein do not necessarily represent the views of Health Canada, or any provincial or territorial government. Reproduction of this document for non-commercial purposes is permitted provided appropriate credit is given to CADTH.