Surgeons and Apothecaries in Suffolk: 1750-1830
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
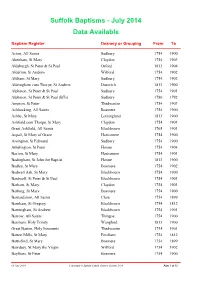
Baptism Data Available
Suffolk Baptisms - July 2014 Data Available Baptism Register Deanery or Grouping From To Acton, All Saints Sudbury 1754 1900 Akenham, St Mary Claydon 1754 1903 Aldeburgh, St Peter & St Paul Orford 1813 1904 Alderton, St Andrew Wilford 1754 1902 Aldham, St Mary Sudbury 1754 1902 Aldringham cum Thorpe, St Andrew Dunwich 1813 1900 Alpheton, St Peter & St Paul Sudbury 1754 1901 Alpheton, St Peter & St Paul (BTs) Sudbury 1780 1792 Ampton, St Peter Thedwastre 1754 1903 Ashbocking, All Saints Bosmere 1754 1900 Ashby, St Mary Lothingland 1813 1900 Ashfield cum Thorpe, St Mary Claydon 1754 1901 Great Ashfield, All Saints Blackbourn 1765 1901 Aspall, St Mary of Grace Hartismere 1754 1900 Assington, St Edmund Sudbury 1754 1900 Athelington, St Peter Hoxne 1754 1904 Bacton, St Mary Hartismere 1754 1901 Badingham, St John the Baptist Hoxne 1813 1900 Badley, St Mary Bosmere 1754 1902 Badwell Ash, St Mary Blackbourn 1754 1900 Bardwell, St Peter & St Paul Blackbourn 1754 1901 Barham, St Mary Claydon 1754 1901 Barking, St Mary Bosmere 1754 1900 Barnardiston, All Saints Clare 1754 1899 Barnham, St Gregory Blackbourn 1754 1812 Barningham, St Andrew Blackbourn 1754 1901 Barrow, All Saints Thingoe 1754 1900 Barsham, Holy Trinity Wangford 1813 1900 Great Barton, Holy Innocents Thedwastre 1754 1901 Barton Mills, St Mary Fordham 1754 1812 Battisford, St Mary Bosmere 1754 1899 Bawdsey, St Mary the Virgin Wilford 1754 1902 Baylham, St Peter Bosmere 1754 1900 09 July 2014 Copyright © Suffolk Family History Society 2014 Page 1 of 12 Baptism Register Deanery or Grouping -

The Journal of New Latin Poetry
VATES The Journal of New Latin Poetry Issue 4, Autumn/Winter 2011-12 CONTENTS Editorial 2 Carmina Latina After the Raid (Brad Walton) 3 2 First World War Poems (Paul Murgatroyd) 7 Webicus Bacchus (Joseph Tusiani) 9 2 Carmina (J. Turner Brakeley) 10 Eoan Airs (Massimo Scorsone) 12 Uxor Tiresiae (Paul Murgatroyd) 26 Pro Senectute Mea (Joseph Tusiani) 29 Laus Bacchi (Raul Lavalle) 30 3 Carmina ex Hobbito Illo (Mark Walker) 32 Features Toiling Up Parnassus (Barry Baldwin) 37 Verba Inaudita (Mark Walker) 40 Book Review: Musa Pedestris (Barry Baldwin) 46 De gustibus non est disputandum 48 Contributors 50 Edited by Mark Walker email: [email protected] Vates is a Pineapple Publications publication Vates Issue 4 Editorial Welcome to this fourth edition of Vates, the free journal of new Latin poetry. I‟m delighted that we are reaching an ever wider and increasingly international audience. Poetry in this issue comes from Italy, Argentina the USA, Canada and the UK. We have readers in Europe, North America, Jamaica, Australia … and the generous contributions from our poets around the globe shows no sign of slowing down, either – quite the opposite, in fact, which is a gratifying indication that we must be doing something right! One issue that prompted me to set up this journal in the first place was the problem of finding a readership for new Latin verse: „Who reads Latin Poems written in these days!‟ wrote Walter Savage Landor‟s exasperated brother in 1820, scarcely able to believe his brother would waste his talents on such a quixotic endeavour, and the situation can hardly be said to have improved since then. -

Felsham Conservation Area Appraisal
FELSHAM CONSERVATION AREA APPRAISAL © Crown copyright All Rights Reserved M S D C Licence no 100017810 2010 INTRODUCTION The conservation area in Felsham was originally designated by Mid Suffolk District Council in 1996. The Council has a duty to review its conservation area designations from time to time, and this appraisal examines Felsham under a number of different headings as set out in English Heritage’s ‘Guidance on Conservation Area Appraisals’ (2006). As such it is a straightforward appraisal of Felsham’s built environment in conservation terms. This document is neither prescriptive nor overly descriptive, but more a demonstration of ‘quality of place’, sufficient for the briefing of the Planning Officer when assessing proposed works in the area. The photographs and maps are thus intended to contribute as much Pump Wheel as the text itself. As the English Heritage guidelines point out, the appraisal is to be read as a general overview, rather than as a comprehensive listing, and the omission of any particular building, feature or space does not imply that it is of no interest in conservation terms. Text, photographs and map overlays by Patrick Taylor, Conservation Architect, Mid Suffolk District Council 2011. Vintage Transport © Crown copyright All Rights Reserved M S D C Licence no 100017810 2010 TOPOGRAPHICAL FRAMEWORK Felsham is situated in central Suffolk about eight miles south-east of Bury St Edmunds. It lies on the boulder clay of ‘High Suffolk’, a recent glacial deposit over chalk at greater depth. The village lies on gently sloping ground between 75 and 85 metres above OD, very much on a watershed, standing near the beginnings of many local waterways. -

Historical Documents, Autographs & Ephemera
Historical Documents, Autographs & Ephemera Thursday 18 August 2011 10:30 Mullock's Specialist Auctioneers The Old Shippon Wall Under Heywood Church Stretton SY6 7DS Mullock's Specialist Auctioneers (Historical Documents, Autographs & Ephemera) Catalogue - Downloaded from UKAuctioneers.com Lot: 1 Correspondents include Archbishops, Bishops and members of West Midlands -Manor of Sedgley the minute books of the the aristocracy. Nelson was an active churchman and wrote Manor commencing February 27th 1817, and May 12th 1821, many hymns and was foremost in compiling the 'Sarum vellum covers, soiled but completely legible, interior contents Hymnal'. A number of these letters are from the Bishop of on paper written in a neat legible hand and in good order.4to. Salisbury who collaborated with Nelson on this work Estimate: £200.00 - £400.00 Estimate: £150.00 - £200.00 Lot: 2 Lot: 7 Autograph -Lord Randolph Churchill original membership Ireland -Acts of Parliament group of approx seven printed Acts application form for the Amphitryon Club, London, signed in of Parliament relating to the Census of Ireland together with pencil by Lord Randolph Churchill as sponsor for Prince extensive printouts on the 1821, 1831 & 1841 censuses Dolgoroukoff, the Imperial Attache for the Russian Ambassador compared (who has also signed), with two further signatures. Dated March Estimate: £70.00 - £100.00 31st 1894. Together with a similar application form for Prince Boris Priatopolk-Czetwertynski, dated August 24th 1891, signed by Lord de Grey and Count Andes Kreutz.Rare. The Lot: 8 Amphitryon Club was, in its day, the most sought after Ireland -Sean O'Duffy scarce printed handbill being a reprint of Gentleman's Club in London, boasting by far the highest prices a letter by Sean O'Duffy which was written to the Irish for food and drink. -

In the Western Mediterranean, 1703–1708
international journal of military history and historiography 39 (2019) 7-33 IJMH brill.com/ijmh Britain, Austria, and the “Burden of War” in the Western Mediterranean, 1703–1708 Caleb Karges* Concordia University Irvine, California [email protected] Abstract The Austrian and British alliance in the Western Mediterranean from 1703 to 1708 is used as a case study in the problem of getting allies to cooperate at the strategic and operational levels of war. Differing grand strategies can lead to disagreements about strategic priorities and the value of possible operations. However, poor personal rela- tions can do more to wreck an alliance than differing opinions over strategy. While good personal relations can keep an alliance operating smoothly, it is often military necessity (and the threat of grand strategic failure) that forces important compro- mises. In the case of the Western Mediterranean, it was the urgent situation created by the Allied defeat at Almanza that forced the British and Austrians to create a work- able solution. Keywords War of the Spanish Succession – Coalition Warfare – Austria – Great Britain – Mediter- ranean – Spain – Strategy * Caleb Karges obtained his MLitt and PhD in Modern History from the University of St An- drews, United Kingdom in 2010 and 2015, respectively. His PhD thesis on the Anglo-Austrian alliance during the War of the Spanish Succession received the International Commission of Military History’s “André Corvisier Prize” in 2017. He is currently an Assistant Professor of History at Concordia University Irvine in Irvine, California, usa. © koninklijke brill nv, leiden, 2019 | doi:10.1163/24683302-03901002Downloaded from Brill.com09/29/2021 03:43:06AM via free access <UN> 8 Karges 1 Introduction1 There were few wars in European history before 1789 as large as the War of the Spanish Succession. -

ELECTORAL DIVISION PROFILE 2017 This Division Comprises Bungay and Wainford Wards in Their Entirety Plus Part of the Saints Ward
UNGAY ELECTORAL DIVISION PROFILE 2017 This Division comprises Bungay and Wainford wards in their entirety plus part of The Saints ward www.suffolkobservatory.info 2 © Crown copyright and database rights 2017 Ordnance Survey 100023395 CONTENTS . Demographic Profile: Age & Ethnicity . Economy and Labour Market . Schools & NEET . Index of Multiple Deprivation . Health . Crime & Community Safety . Additional Information . Data Sources 3 ELECTORAL DIVISION PROFILES: AN INTRODUCTION These profiles have been produced to support elected members, constituents and other interested parties in understanding the demographic, economic, social and educational profile of their neighbourhoods. We have used the latest data available at the time of publication. Much more data is available from national and local sources than is captured here, but it is hoped that the profile will be a useful starting point for discussion, where local knowledge and experience can be used to flesh out and illuminate the information presented here. The profile can be used to help look at some fundamental questions e.g. Does the age profile of the population match or differ from the national profile? . Is there evidence of the ageing profile of the county in all the wards in the Division or just some? . How diverse is the community in terms of ethnicity? . What is the impact of deprivation on families and residents? . Does there seem to be a link between deprivation and school performance? . What is the breakdown of employment sectors in the area? . Is it a relatively healthy area compared to the rest of the district or county? . What sort of crime is prevalent in the community? A vast amount of additional data is available on the Suffolk Observatory www.suffolkobservatory.info The Suffolk Observatory is a free online resource that contains all Suffolk’s vital statistics; it is the one‐stop‐shop for information and intelligence about Suffolk. -

Medical Students in England and France, 1815-1858
FLORENT PALLUAULT D.E.A., archiviste paléographe MEDICAL STUDENTS IN ENGLAND AND FRANCE 1815-1858 A COMPARATIVE STUDY University of Oxford Faculty of Modern History - History of Science Thesis submitted for the degree of Doctor in Philosophy Trinity 2003 ACKNOWLEDGMENTS In the first instance, my most sincere gratitude goes to Dr Ruth Harris and Dr Margaret Pelling who have supervised this thesis. Despite my slow progress, they have supported my efforts and believed in my capacities to carry out this comparative study. I hope that, despite its defects, it will prove worthy of their trust. I would like to thank Louella Vaughan for providing an interesting eighteenth-century perspective on English medical education, sharing her ideas on my subject and removing some of my misconceptions. Similarly, I thank Christelle Rabier for her support and for our discussions regarding her forthcoming thesis on surgery in England and France. My thanks naturally go to the staff of the various establishments in which my research has taken me, and particularly to the librarians at the Wellcome Library for the History and Understanding of Medicine in London, the librarians in the History of Science Room at the Bibliothèque nationale de France in Paris, and to Bernadette Molitor and Henry Ferreira-Lopes at the Bibliothèque Inter-Universitaire de Médecine in Paris. I am grateful to Patricia Gillet from the Association d’entraide des Anciens élèves de l’École des Chartes for the financial support that the Association has given me and to Wes Cordeau at Texas Supreme Mortgage, Inc. for the scholarship that his company awarded me. -

WSC Planning Decisions 43/19
PLANNING AND REGULATORY SERVICES DECISIONS WEEK ENDING 25/10/2019 PLEASE NOTE THE DECISIONS LIST RUN FROM MONDAY TO FRIDAY EACH WEEK DC/15/2298/FUL Planning Application - (i) Extension and Village Hall DECISION: alterations to Hopton Village Hall (ii) Thelnetham Road Approve Application Doctor's surgery and associated car Hopton DECISION TYPE: parking and the modification of the existing Suffolk Committee vehicular access onto Thelnetham Road IP22 2QY ISSUED DATED: (iii) residential development of 37 24 Oct 2019 dwellings (including 11 affordable housing WARD: Barningham units) and associated public open space PARISH: Hopton Cum including a new village green, Knettishall landscaping,ancillary works and creation of new vehicular access onto Bury Road APPLICANT: Pigeon Investment Management AGENT: Evolution Town Planning LLP - Mr David Barker DC/18/0628/HYB Hybrid Planning Application - 1. Full Former White House Stud, DECISION: Planning Application - (i) Horse racing White Lodge Stables Refuse Application industry facility (including workers Warren Road DECISION TYPE: dwelling) and (ii) new access (following Herringswell Delegated demolition of existing buildings to the CB8 7QP ISSUED DATED: south of the site) 2. Outline Planning 22 Oct 2019 Application (Means of Access to be WARD: Iceni considered) (i) up to 100no. dwellings and PARISH: Herringswell (ii) new access (following demolition of existing buildings to the north of the site and the existing dwelling known as White Lodge Bungalow). APPLICANT: Hill Residential Ltd AGENT: Mrs Meghan Bonner - KWA Architects (Cambridge) Ltd Planning and Regulatory Services, West Suffolk Council, West Suffolk House, Western Way, Bury St Edmunds, Suffolk, IP33 3YU DC/19/0235/FUL Planning Application - 2no. -

E-Book Code: REAU1036
E-book Code: REAU1036 Written by Margaret Etherton. Illustrated by Terry Allen. Published by Ready-Ed Publications (2007) © Ready-Ed Publications - 2007. P.O. Box 276 Greenwood Perth W.A. 6024 Email: [email protected] Website: www.readyed.com.au COPYRIGHT NOTICE Permission is granted for the purchaser to photocopy sufficient copies for non-commercial educational purposes. However, this permission is not transferable and applies only to the purchasing individual or institution. ISBN 1 86397 710 4 12345678901234567890123456789012123456789012345678901234567890121234567890123456789012345678901212345678901234567890123456789012123456789012345 12345678901234567890123456789012123456789012345678901234567890121234567890123456789012345678901212345678901234567890123456789012123456789012345 12345678901234567890123456789012123456789012345678901234567890121234567890123456789012345678901212345678901234567890123456789012123456789012345 12345678901234567890123456789012123456789012345678901234567890121234567890123456789012345678901212345678901234567890123456789012123456789012345 12345678901234567890123456789012123456789012345678901234567890121234567890123456789012345678901212345678901234567890123456789012123456789012345 12345678901234567890123456789012123456789012345678901234567890121234567890123456789012345678901212345678901234567890123456789012 12345678901234 5 12345678901234567890123456789012123456789012345678901234567890121234567890123456789012345678901212345678901234567890123456789012123456789012345 12345678901234567890123456789012123456789012345678901234567890121234567890123456789012345678901212345678901234567890123456789012123456789012345 -

ARCHAEOLOGY in SUFFOLK ARCHAEOLOGICAL FINDS, 1980� Compiled by Edward Martin, Judith Plouviez and Hilary Ross
ARCHAEOLOGY IN SUFFOLK ARCHAEOLOGICAL FINDS, 1980 compiled by Edward Martin, Judith Plouviez and Hilary Ross Once again this is a selection of the new sites and finds discovered during the year. All the siteson this list have been incorporated into the County's Sites and Monuments Index; the reference to this is the final number given in each entry, preceded by the abbreviation S.A.U. Information for this list has been contributed by Miss E. Owles, Moyses Hall Museum; Mr C. Pendleton, Mildenhall Museum; Mr A. Pye, Lowestoft Archaeological Society; and Mr D. Sherlock. The drawings of the axes from Covehithe were kindly supplied by Mr P. Durbridge. Abbreviations: I. M. Ipswich Museum L.A.S. Lowestoft Archaeological and Local History Society M.H. MoysesHall Museum, Bury St Edmunds M.M. Mildenhall Museum S.A.U. Suffolk Archaeological Unit, Shire Hall, Bury St Edmunds T.M. Thetford Museum Pa Palaeolithic AS Anglo-Saxon Me Mesolithic MS Middle Saxon Ne Neolithic LS Late Saxon BA Bronze Age Md Medieval IA Iron Age PM Post-Medieval RB Romano-British UN Period unknown Aldringham (TM/4760). Ne. Flaked flint axe, found in a garden several years ago. (F. B. Macrae; S.A.U. ARG 008). Aldringham (TM/4759). Md. The disturbed remain.s of a skeleton, lying in an east-west grave, were found in a gas mains service trench at the end of the archway between the Thorpeness Almshouses. At least one other skeleton was intact beneath it and there may have been more. These are probably associated with the medieval St Mary's Chapel, Thorpe, which formerly existed in that area. -

Baptism Data Available
Suffolk Baptisms - January 2019 Data Available Baptism Register Deanery or Grouping From To Acton, All Saints Sudbury 1754 1900 Akenham, St Mary Claydon 1754 1903 Aldeburgh, St Peter & St Paul Orford 1754 1904 Alderton, St Andrew Wilford 1754 1902 Aldham, St Mary Sudbury 1754 1902 Aldringham cum Thorpe, St Andrew Dunwich 1754 1900 Aldringham, Particular Baptist Baptist 1809 1837 Alpheton, St Peter & St Paul Sudbury 1754 1901 Alpheton, St Peter & St Paul (BTs) Sudbury 1780 1792 Ampton, St Peter Thedwastre 1650 1903 Ashbocking, All Saints Bosmere 1754 1900 Ashby, St Mary Lothingland 1813 1900 Ashfield cum Thorpe, St Mary Claydon 1754 1901 Great Ashfield, All Saints Blackbourn 1765 1901 Aspall, St Mary of Grace Hartismere 1754 1900 Assington, St Edmund Sudbury 1754 1900 Athelington, St Peter Hoxne 1754 1904 Bacton, St Mary Hartismere 1754 1901 Badingham, St John the Baptist Hoxne 1754 1900 Badley, St Mary Bosmere 1754 1902 Badwell Ash, St Mary Blackbourn 1650 1900 Bardwell, Baptist Baptist 1820 1837 Bardwell, St Peter & St Paul Blackbourn 1650 1901 Barham, St Mary Claydon 1754 1901 Barking, St Mary Bosmere 1754 1900 Barnardiston, All Saints Clare 1650 1899 Barnby, St John the Baptist Lothingland 1813 1900 Barnham, St Gregory Blackbourn 1730 1902 Barningham, St Andrew Blackbourn 1650 1901 Barrow, All Saints Thingoe 1754 1900 Barsham, Holy Trinity Wangford 1813 1900 Great Barton, Holy Innocents Thedwastre 1650 1901 Barton Mills, St Mary Fordham 1663 1901 01 January 2019 Copyright © Suffolk Family History Society 2019 Page 1 of 16 Baptism Register -
Report Writing
MID SUFFOLK DISTRICT COUNCIL To: Council Report Number: C/63/14 From: Corporate Manager – Elections and Date of meeting: 17 December 2014 Electoral Management REVIEW OF POLLING DISTRICTS, POLLING PLACES AND POLLING STATIONS 1. Purpose of Report 1.1 In accordance with the Electoral Registration and Administration Act 2013, every council in England and Wales must undertake and complete a review of all of the polling districts and polling places in its area. 1.2 Guidance produced by the Electoral Commission sets out the process for a review, and this has been followed. 1.3 The appendix to this report provides a list of the recommended polling districts, polling places and polling stations, showing the changes which have been made since the last review. 2. Recommendations 2.1 That the Council adopts the Polling Districts, Polling Places and Polling Stations as listed in Appendix A to this report. 2.2 That the Council notes the Polling Stations proposed by the Returning Officer as listed in Appendix A to this report. 3. Financial Implications 3.1 There are none. 4. Risk Management 4.1 This report is not linked with any of the Council’s Corporate / Significant Business Risks. 5. Consultations 5.1 Consultation has taken place with Parish and Town Councils, District and County councillors, the Acting Returning Officer and other interested parties. 6. Equality and Diversity Impact 6.1 Access to polling stations is a factor that is taken into account when deciding on a suitable location. 44 7. Shared Service / Partnership Implications 7.1 There are none. 8.