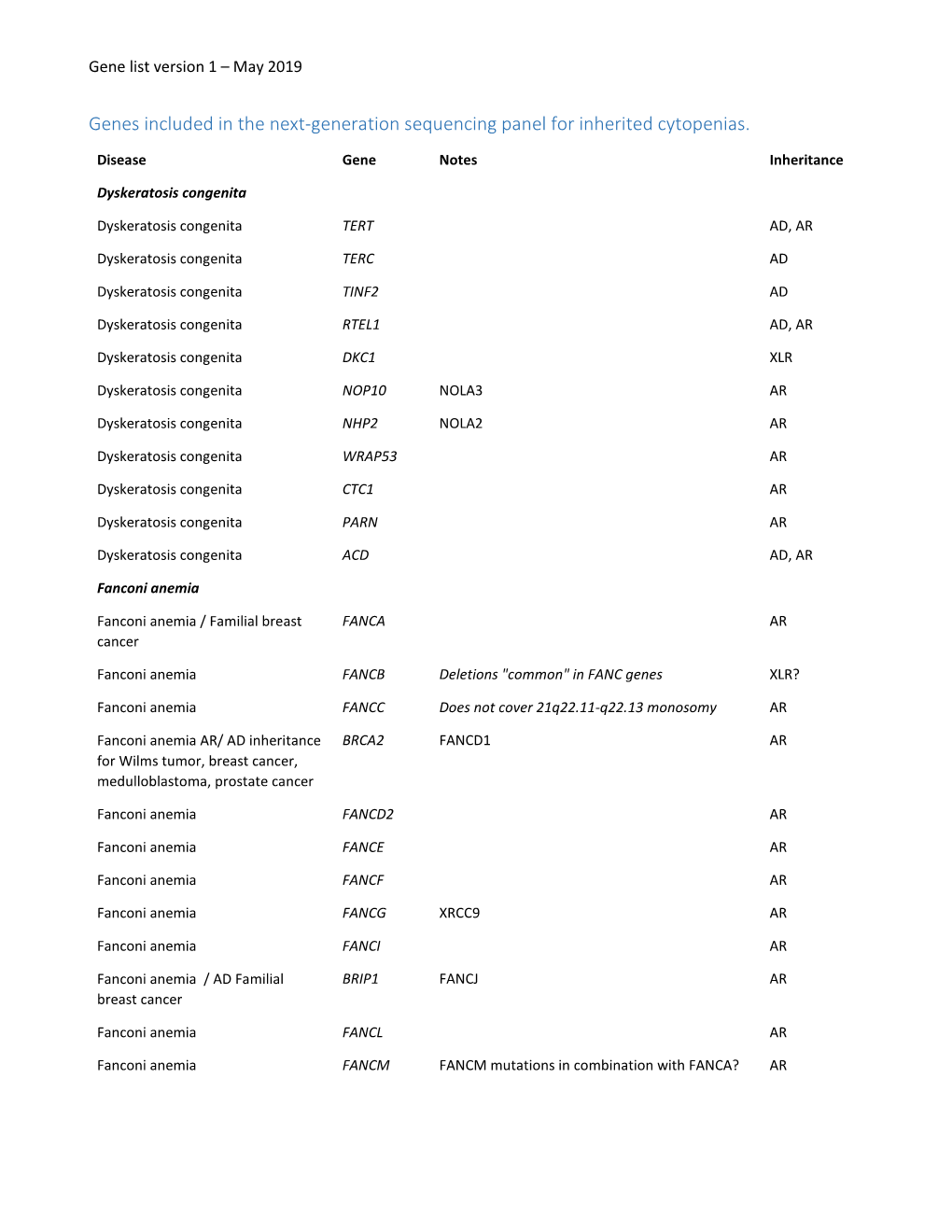
Genes Included in the Next-Generation Sequencing Panel for Inherited Cytopenias
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

WHIM Syndrome: from Pathogenesis Towards Personalized Medicine and Cure
Journal of Clinical Immunology (2019) 39:532–556 https://doi.org/10.1007/s10875-019-00665-w CME REVIEW WHIM Syndrome: from Pathogenesis Towards Personalized Medicine and Cure Lauren E. Heusinkveld1,2 & Shamik Majumdar1 & Ji-Liang Gao1 & David H. McDermott1 & Philip M. Murphy1 Received: 22 April 2019 /Accepted: 26 June 2019 /Published online: 16 July 2019 # This is a U.S. Government work and not under copyright protection in the US; foreign copyright protection may apply 2019 Abstract WHIM syndrome is a rare combined primary immunodeficiency disease named by acronym for the diagnostic tetrad of warts, hypogammaglobulinemia, infections, and myelokathexis. Myelokathexis is a unique form of non-cyclic severe congenital neutropenia caused by accumulation of mature and degenerating neutrophils in the bone marrow; monocytopenia and lympho- penia, especially B lymphopenia, also commonly occur. WHIM syndrome is usually caused by autosomal dominant mutations in the G protein-coupled chemokine receptor CXCR4 that impair desensitization, resulting in enhanced and prolonged G protein- and β-arrestin-dependent responses. Accordingly, CXCR4 antagonists have shown promise as mechanism-based treatments in phase 1 clinical trials. This review is based on analysis of all 105 published cases of WHIM syndrome and covers current concepts, recent advances, unresolved enigmas and controversies, and promising future research directions. Keywords Chemokine . CXCL12 . CXCR4 . CXCR2 . myelokathexis . human papillomavirus . plerixafor Historical Background [M:E] ratio with a “shift to the right”); and (3) numerous dysmorphic bone marrow neutrophils having cytoplasmic Myelokathexis was first described as a new type of severe hypervacuolation and hyperlobulated pyknotic nuclear lobes congenital neutropenia in 1964 by Krill and colleagues from connected by long thin strands (Fig. -

Some ABCA3 Mutations Elevate ER Stress and Initiate Apoptosis of Lung Epithelial Cells
Some ABCA3 mutations elevate ER stress and initiate apoptosis of lung epithelial cells Nina Weichert Aus der Kinderklinik und Kinderpoliklinik im Dr. von Haunerschen Kinderspital der Ludwig-Maximilians-Universität München Direktor: Prof. Dr. med. Dr. sci. nat. Christoph Klein Some ABCA3 mutations elevate ER stress and initiate apoptosis of lung epithelial cells Dissertation zum Erwerb des Doktorgrades der Humanmedizin an der Medizinischen Fakultät der Ludwig-Maximilians-Universität zu München Vorgelegt von Nina Weichert aus Heidelberg 2011 Mit Genehmigung der Medizinischen Fakultät der Universität München 1. Berichterstatter: Prof. Dr. Matthias Griese 2. Berichterstatter: Prof. Dr. Dennis Nowak Mitberichterstatter: Priv. Doz. Dr. Angela Abicht Prof. Dr. Michael Schleicher Mitbetreuung durch den promovierten Mitarbeiter: Dr. Suncana Kern Dekan: Herr Prof. Dr. med. Dr. h. c. Maximilian Reiser, FACR, FRCR Tag der mündlichen Prüfung: 24.11.2011 Table of Contents 1.Abstract ................................................................................................................... 1 2.Zusammenfassung................................................................................................. 2 3.Intoduction .............................................................................................................. 3 3.1 Pediatric interstitial lung disease ............................................................................... 3 3.1.1 Epidemiology of pILD.............................................................................................. -

Prevalence and Incidence of Rare Diseases: Bibliographic Data
Number 1 | January 2019 Prevalence and incidence of rare diseases: Bibliographic data Prevalence, incidence or number of published cases listed by diseases (in alphabetical order) www.orpha.net www.orphadata.org If a range of national data is available, the average is Methodology calculated to estimate the worldwide or European prevalence or incidence. When a range of data sources is available, the most Orphanet carries out a systematic survey of literature in recent data source that meets a certain number of quality order to estimate the prevalence and incidence of rare criteria is favoured (registries, meta-analyses, diseases. This study aims to collect new data regarding population-based studies, large cohorts studies). point prevalence, birth prevalence and incidence, and to update already published data according to new For congenital diseases, the prevalence is estimated, so scientific studies or other available data. that: Prevalence = birth prevalence x (patient life This data is presented in the following reports published expectancy/general population life expectancy). biannually: When only incidence data is documented, the prevalence is estimated when possible, so that : • Prevalence, incidence or number of published cases listed by diseases (in alphabetical order); Prevalence = incidence x disease mean duration. • Diseases listed by decreasing prevalence, incidence When neither prevalence nor incidence data is available, or number of published cases; which is the case for very rare diseases, the number of cases or families documented in the medical literature is Data collection provided. A number of different sources are used : Limitations of the study • Registries (RARECARE, EUROCAT, etc) ; The prevalence and incidence data presented in this report are only estimations and cannot be considered to • National/international health institutes and agencies be absolutely correct. -

Practice Parameter for the Diagnosis and Management of Primary Immunodeficiency
Practice parameter Practice parameter for the diagnosis and management of primary immunodeficiency Francisco A. Bonilla, MD, PhD, David A. Khan, MD, Zuhair K. Ballas, MD, Javier Chinen, MD, PhD, Michael M. Frank, MD, Joyce T. Hsu, MD, Michael Keller, MD, Lisa J. Kobrynski, MD, Hirsh D. Komarow, MD, Bruce Mazer, MD, Robert P. Nelson, Jr, MD, Jordan S. Orange, MD, PhD, John M. Routes, MD, William T. Shearer, MD, PhD, Ricardo U. Sorensen, MD, James W. Verbsky, MD, PhD, David I. Bernstein, MD, Joann Blessing-Moore, MD, David Lang, MD, Richard A. Nicklas, MD, John Oppenheimer, MD, Jay M. Portnoy, MD, Christopher R. Randolph, MD, Diane Schuller, MD, Sheldon L. Spector, MD, Stephen Tilles, MD, Dana Wallace, MD Chief Editor: Francisco A. Bonilla, MD, PhD Co-Editor: David A. Khan, MD Members of the Joint Task Force on Practice Parameters: David I. Bernstein, MD, Joann Blessing-Moore, MD, David Khan, MD, David Lang, MD, Richard A. Nicklas, MD, John Oppenheimer, MD, Jay M. Portnoy, MD, Christopher R. Randolph, MD, Diane Schuller, MD, Sheldon L. Spector, MD, Stephen Tilles, MD, Dana Wallace, MD Primary Immunodeficiency Workgroup: Chairman: Francisco A. Bonilla, MD, PhD Members: Zuhair K. Ballas, MD, Javier Chinen, MD, PhD, Michael M. Frank, MD, Joyce T. Hsu, MD, Michael Keller, MD, Lisa J. Kobrynski, MD, Hirsh D. Komarow, MD, Bruce Mazer, MD, Robert P. Nelson, Jr, MD, Jordan S. Orange, MD, PhD, John M. Routes, MD, William T. Shearer, MD, PhD, Ricardo U. Sorensen, MD, James W. Verbsky, MD, PhD GlaxoSmithKline, Merck, and Aerocrine; has received payment for lectures from Genentech/ These parameters were developed by the Joint Task Force on Practice Parameters, representing Novartis, GlaxoSmithKline, and Merck; and has received research support from Genentech/ the American Academy of Allergy, Asthma & Immunology; the American College of Novartis and Merck. -

Commonly Used Lipidcentric ICD-10 (ICD-9) Codes
Commonly Used Lipidcentric ICD-10 (ICD-9) Codes *This is not an all inclusive list of ICD-10 codes R.LaForge 11/2015 E78.0 (272.0) Pure hypercholesterolemia E78.3 (272.3) Hyperchylomicronemia (Group A) (Group D) Familial hypercholesterolemia Grütz syndrome Fredrickson Type IIa Chylomicronemia (fasting) (with hyperlipoproteinemia hyperprebetalipoproteinemia) Hyperbetalipoproteinemia Fredrickson type I or V Hyperlipidemia, Group A hyperlipoproteinemia Low-density-lipoid-type [LDL] Lipemia hyperlipoproteinemia Mixed hyperglyceridemia E78.4 (272.4) Other hyperlipidemia E78.1 (272.1) Pure hyperglyceridemia Type 1 Diabetes Mellitus (DM) with (Group B) hyperlipidemia Elevated fasting triglycerides Type 1 DM w diabetic hyperlipidemia Endogenous hyperglyceridemia Familial hyperalphalipoproteinemia Fredrickson Type IV Hyperalphalipoproteinemia, familial hyperlipoproteinemia Hyperlipidemia due to type 1 DM Hyperlipidemia, Group B Hyperprebetalipoproteinemia Hypertriglyceridemia, essential E78.5 (272.5) Hyperlipidemia, unspecified Very-low-density-lipoid-type [VLDL] Complex dyslipidemia hyperlipoproteinemia Elevated fasting lipid profile Elevated lipid profile fasting Hyperlipidemia E78.2 (272.2) Mixed hyperlipidemia (Group C) Hyperlipidemia (high blood fats) Broad- or floating-betalipoproteinemia Hyperlipidemia due to steroid Combined hyperlipidemia NOS Hyperlipidemia due to type 2 diabetes Elevated cholesterol with elevated mellitus triglycerides NEC Fredrickson Type IIb or III hyperlipoproteinemia with E78.6 (272.6) -

:.. ;}.·:···.·;·1 Congenital Neutropenia
C HAP T E R 13 >;:.. ;}.·:···.·;·1 CONGENITAL NEUTROPENIA Jill M. Watanabe, MD, MPH, and David C. Dale, MD defined by a neutrophil count less than 1500 cellS/ilL; KEY POINTS beyond 10 years of age, neutropenia is defined by a neu trophil count less' than 1800 cells//1L in persons of white Congenital Neutropenia and Asian descent. 1 In persons of African descent, neu tropenia is defined by a count of 800--1000 cells//1L. 1 (& Congenital neutropenia encompasses a heterogeneous group of The severity and duration of neutropenia are also clin iuheri ted diseases. ically important. Mild neutropenia is usually defined by • The genetic mutations causing congenital neutropenia may neutrophil counts of 1000-1500 cells//1L, moderate neu have an isolated effect on the bone marrow but can also affect tropenia is 500-1000 cells//1L, and severe neutropenia one or more other organ systems. is less than 500 cells//1L. Acute neutropenia usually is present for only 5-10 days; neutropenia is chronic if its (& The genetic defects underlying the diseases that cause con duration is at least several weeks. Almost all congenital genital neutropenia have been rapidly identified over the past neutropenias are chronic neutropenia. decade. The characteristics and causes of congenital neu (& Granulocyte colony-stimulating factor has dramatically tropenia are shown in Tables 13-1 and 13-2, and an algo improved the prognosis for children with congenital rithm for their diagnosis is presented in Figure 13-1. neutropenia. SEVERE CONGENITAL NEUTROPENIA Patient'; with severe congenital neutropenia (SCN) typi cally present with recurrent bacterial infections and neutrophil count'> persistently less than 200 cells//1L. -

Patient Handbook 3-2-10
∑ UNDERSTANDING SEVERE CHRONIC NEUTROPENIA A Handbook for Patients and Their Families Written for the Severe Chronic Neutropenia International Registry By: Audrey Anna Bolyard, R.N., B.S. Laurence Boxer, M.D. Tammy Cottle Carole Edwards, R.G.N/R.S.C.N., BSc. Sally Kinsey, M.D. Peter Newburger, M.D. Beate Schwinzer, Ph.D. Cornelia Zeidler, M.D. Understanding Severe Chronic Neutropenia 1 A handbook for patients and their families Revised February 2010 ∑ Contents Page Introduction 3 How Blood is Formed 3 What is Neutropenia? 4 Overview: Diagnosis & Treatment of Severe Chronic Neutropenia 5 Risk of Myelodysplastic Syndrome and Leukemia 6 Risk of Osteopenia/Osteoporosis 7 Types of Severe Chronic Neutropenia 7 Severe Congenital Neutropenia 8 Cyclic Neutropenia 8 Shwachman-Diamond Syndrome 9 Metabolic disorders with neutropenia 10 Glycogen-Storage Disease Type 1b 10 Barth Syndrome 10 Idiopathic Neutropenia 10 Autoimmune Neutropenia 10 Other Conditions Associated with Neutropenia 11 Genetics of Severe Congenital Neutropenia 11 Diagnostic Tests Used in Severe Chronic Neutropenia 12 Blood Count Monitoring 12 Other Blood Tests 12 Bone Marrow Aspirate / Trephine Biopsy 12 Cytogenetic Evaluation 12 Investigations in Other Conditions 12 Treatment for Severe Chronic Neutropenia 13 Granulocyte-Colony Stimulating Factor (G-CSF) 14 Hematopoietic Stem Cell (Bone Marrow) Transplant 15 Other Treatments 15 Long Term Management of SCN 16 Bone Marrow Monitoring 17 Pregnancy 17 Psychosocial Issues 17 The Severe Chronic Neutropenia International Registry 18 Support Groups 20 Frequently Asked Questions and Answers 20 Information Form for Schools 24 Glossary 25 Understanding Severe Chronic Neutropenia 2 A handbook for patients and their families Revised February 2010 ∑ Introduction Severe chronic neutropenia (SCN) is the name given to a group of conditions in which neutropenia is the primary problem. -

Whole-Exome Sequencing Identifies Causative Mutations in Families
BASIC RESEARCH www.jasn.org Whole-Exome Sequencing Identifies Causative Mutations in Families with Congenital Anomalies of the Kidney and Urinary Tract Amelie T. van der Ven,1 Dervla M. Connaughton,1 Hadas Ityel,1 Nina Mann,1 Makiko Nakayama,1 Jing Chen,1 Asaf Vivante,1 Daw-yang Hwang,1 Julian Schulz,1 Daniela A. Braun,1 Johanna Magdalena Schmidt,1 David Schapiro,1 Ronen Schneider,1 Jillian K. Warejko,1 Ankana Daga,1 Amar J. Majmundar,1 Weizhen Tan,1 Tilman Jobst-Schwan,1 Tobias Hermle,1 Eugen Widmeier,1 Shazia Ashraf,1 Ali Amar,1 Charlotte A. Hoogstraaten,1 Hannah Hugo,1 Thomas M. Kitzler,1 Franziska Kause,1 Caroline M. Kolvenbach,1 Rufeng Dai,1 Leslie Spaneas,1 Kassaundra Amann,1 Deborah R. Stein,1 Michelle A. Baum,1 Michael J.G. Somers,1 Nancy M. Rodig,1 Michael A. Ferguson,1 Avram Z. Traum,1 Ghaleb H. Daouk,1 Radovan Bogdanovic,2 Natasa Stajic,2 Neveen A. Soliman,3,4 Jameela A. Kari,5,6 Sherif El Desoky,5,6 Hanan M. Fathy,7 Danko Milosevic,8 Muna Al-Saffar,1,9 Hazem S. Awad,10 Loai A. Eid,10 Aravind Selvin,11 Prabha Senguttuvan,12 Simone Sanna-Cherchi,13 Heidi L. Rehm,14 Daniel G. MacArthur,14,15 Monkol Lek,14,15 Kristen M. Laricchia,15 Michael W. Wilson,15 Shrikant M. Mane,16 Richard P. Lifton,16,17 Richard S. Lee,18 Stuart B. Bauer,18 Weining Lu,19 Heiko M. Reutter ,20,21 Velibor Tasic,22 Shirlee Shril,1 and Friedhelm Hildebrandt1 Due to the number of contributing authors, the affiliations are listed at the end of this article. -

Rush University Medical Center, May 2008
Chicago Dermatological Society May 2008 Monthly Educational Conference Program Information Continuing Medical Education Certification and Case Presentations Wednesday, May 21, 2008 Conference Host: Department of Dermatology Rush University Medical Center Chicago, Illinois Chicago Dermatological Society 10 W. Phillip Rd., Suite 120 Vernon Hills, IL 60061-1730 (847) 680-1666 Fax: (847) 680-1682 Email: [email protected] CDS Monthly Conference Program May 2008 -- Rush University Medical Center May 21, 2008 8:30 a.m. REGISTRATION & CONTINENTAL BREAKFAST Searle Conference Center, Professional Bldg., 5th Floor; Elevator II 9:00 a.m. - 10:00 a.m. RESIDENT LECTURE Brainard; Searle Conference Center 9:30 a.m. - 11:00 a.m. CLINICAL ROUNDS Patient Viewing Dermatology Clinic - Room 264 Professional Building (Elevator III) Slide Viewing Herrick; Searle Conference Center 11:00 a.m. - 12:00 p.m. GENERAL SESSION Brainard; Searle Conference Center 11:00 a.m. CDS Business Meeting 11:15 a.m. FREDERICK MALKINSON LECTURE -- “Vaccines for the Prevention of Infectious Diseases with Mucocutaneous Manifestations” Stephen K. Tyring, MD, PhD 12:15 p.m. - 1:15 p.m. AWARDS LUNCHEON Garden Room - 5th Floor Professional Building 1:15 p.m. - 3:00 p.m. AFTERNOON GENERAL SESSION Brainard; Searle Conference Center RESEARCH GRANT PRESENTATIONS -- “Evaluation and Manipulation of Cellular Molecular Determinants of ALA-induced PpIx Forumation” Bernhard Ortel, MD; University of Chicago “Topical Therapuetic Options for Keratosis Pilaris” Sarah Kasprowicz, MD; Rush University Discussion of cases observed during morning clinical rounds Joan Guitart, MD, moderator Stephen K. Tyring, MD, PhD CME Information This activity is jointly sponsored by the Chicago Medical Society and the Chicago Dermatological Society. -

Pathology of Tangier Disease
J Clin Pathol: first published as 10.1136/jcp.24.7.609 on 1 October 1971. Downloaded from J. clin. Path., 1971, 24, 609-616 Pathology of Tangier disease PATRICIA M. BALE, P. CLIFTON-BLIGH, B. N. P. BENJAMIN, AND H. M. WHYTE From the Institute of Pathology, Royal Alexandra Hospital for Children, Camperdown, Sydney, and the Department of Clinical Science, Australian National University, Canberra sYNoPsis Two cases of Tangier disease are described in children from families unrelated to each other. Necropsy in one case, the first to be reported in this condition, showed large collections of cholesterol-laden macrophages in tonsils, thymus, lymph nodes, and colon, and moderate numbers in pyelonephritic scars and ureter. As the storage cells may be scanty in marrow, jejunum, and liver, the rectum is suggested as the site of choice for biopsy. The diagnosis was confirmed by demonstrating the absence of a-lipoproteins from the plasma of the living child, and by finding low plasma levels in both parents of both cases. The disease can be distinguished from other lipidoses by differences in the predominant sites of storage, staining re- actions, and serum lipid studies. Tangier disease is a familial storage disorder in necropsied case. The 12 subjects (Table I) have come which esterified cholesterol accumulates in macro- from eight families, the first of which lived on copyright. phages, while plasma cholesterol is low, and plasma Tangier Island, Chesapeake Bay, Virginia. Males high density lipoprotein is virtually absent. and females have been equally represented, and Ten cases have been reported, and we have studied affected relatives have always oeen siblings, never two additional patients, one of whom is the first parent and child, suggesting an autosomal recessive Received for publication 27 November 1970. -

Blueprint Genetics Comprehensive Hematology and Hereditary Cancer
Comprehensive Hematology and Hereditary Cancer Panel Test code: HE1401 Is a 348 gene panel that includes assessment of non-coding variants. Is ideal for patients with a clinical suspicion of hematological disorder with genetic predisposition to malignancies. This panel is designed to detect heritable germline mutations and should not be used for the detection of somatic mutations in tumor tissue. Is not recommended for patients suspected to have anemia due to alpha-thalassemia (HBA1 or HBA2). These genes are highly homologous reducing mutation detection rate due to challenges in variant call and difficult to detect mutation profile (deletions and gene-fusions within the homologous genes tandem in the human genome). Is not recommended for patients with a suspicion of severe Hemophilia A if the common inversions are not excluded by previous testing. An intron 22 inversion of the F8 gene is identified in 43%-45% individuals with severe hemophilia A and intron 1 inversion in 2%-5% (GeneReviews NBK1404; PMID:8275087, 8490618, 29296726, 27292088, 22282501, 11756167). This test does not detect reliably these inversions. Is not recommended for patients suspected to have anemia due to alpha-thalassemia (HBA1 or HBA2). These genes are highly homologous reducing mutation detection rate due to challenges in variant call and difficult to detect mutation profile (deletions and gene-fusions within the homologous genes tandem in the human genome). About Comprehensive Hematology and Hereditary Cancer Inherited hematological diseases are a group of blood disorders with variable clinical presentation. Many of them predispose to malignancies and for example patients with inherited bone marrow failure syndromes (Fanconi anemia) have a high risk of developing cancer, either leukemia or solid tumors. -

Mutation of the ABCA1 Gene in Hypoalphalipoproteinemia with Corneal Lipidosis
4600/366J Hum Genet (2002) 47:366–369 N. Matsuda et al.: © Jpn EGF Soc receptor Hum Genet and osteoblastic and Springer-Verlag differentiation 2002 SHORT COMMUNICATION Jun Ishii · Makoto Nagano · Takeshi Kujiraoka Mitsuaki Ishihara · Tohru Egashira · Daisuke Takada Masahiro Tsuji · Hiroaki Hattori · Mitsuru Emi Clinical variant of Tangier disease in Japan: mutation of the ABCA1 gene in hypoalphalipoproteinemia with corneal lipidosis Received: March 1, 2002 / Accepted: March 15, 2002 Abstract Despite progress in molecular characterization, hypoalphalipoproteinemia syndromes have hampered their specific diagnoses of disorders belonging to a group of in- classification into distinct disease entities. From a clinical herited hypoalphalipoproteinemias, i.e., apolipoprotein AI standpoint, the term “inherited hypoalphalipoproteinemia” deficiency, lecithin-cholesterol acyltransferase deficiency, can apply to apolipoprotein AI (apoAI) deficiency, lecithin- Tangier disease (TD), and familial high-density lipoprotein cholesterol acyltransferase (LCAT) deficiency, Tangier (HDL) deficiency, remain difficult on a purely clinical basis. disease (TD), or so-called familial high-density lipoprotein Several TD patients were recently found to be homozygous (HDL) deficiency (Assmann et al. 1995). Despite some for mutations in the ABCA1 gene. We have documented progress in molecular characterization, specific diagnoses of here a clinical variant of TD in a Japanese patient who these disorders remain difficult because of their phenotypic manifested corneal lipidosis and premature coronary artery spectra overlap and because the penetrance of some symp- disease as well as an almost complete absence of HDL- toms is age related. cholesterol, by identifying a novel homozygous ABCA1 Mutation in ABCA1, a gene mapping to 9q31 and encod- mutation (R1680W). We propose that patients with ap- ing an ATP-binding cassette transporter, confers suscepti- parently isolated HDL deficiency who are found to carry bility to TD, a recessive disease (Bodzioch et al.