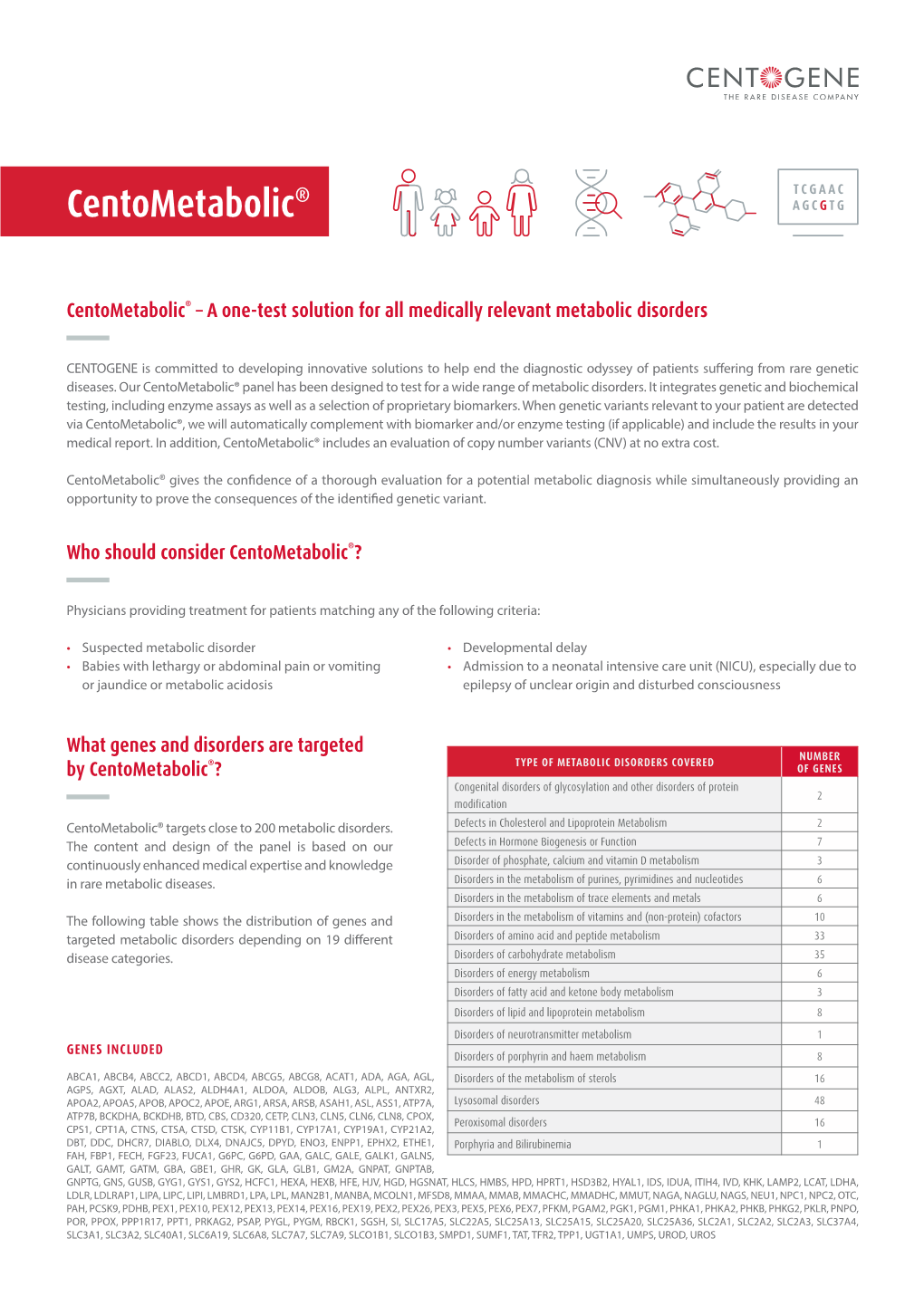
Centometabolic®
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Seq2pathway Vignette
seq2pathway Vignette Bin Wang, Xinan Holly Yang, Arjun Kinstlick May 19, 2021 Contents 1 Abstract 1 2 Package Installation 2 3 runseq2pathway 2 4 Two main functions 3 4.1 seq2gene . .3 4.1.1 seq2gene flowchart . .3 4.1.2 runseq2gene inputs/parameters . .5 4.1.3 runseq2gene outputs . .8 4.2 gene2pathway . 10 4.2.1 gene2pathway flowchart . 11 4.2.2 gene2pathway test inputs/parameters . 11 4.2.3 gene2pathway test outputs . 12 5 Examples 13 5.1 ChIP-seq data analysis . 13 5.1.1 Map ChIP-seq enriched peaks to genes using runseq2gene .................... 13 5.1.2 Discover enriched GO terms using gene2pathway_test with gene scores . 15 5.1.3 Discover enriched GO terms using Fisher's Exact test without gene scores . 17 5.1.4 Add description for genes . 20 5.2 RNA-seq data analysis . 20 6 R environment session 23 1 Abstract Seq2pathway is a novel computational tool to analyze functional gene-sets (including signaling pathways) using variable next-generation sequencing data[1]. Integral to this tool are the \seq2gene" and \gene2pathway" components in series that infer a quantitative pathway-level profile for each sample. The seq2gene function assigns phenotype-associated significance of genomic regions to gene-level scores, where the significance could be p-values of SNPs or point mutations, protein-binding affinity, or transcriptional expression level. The seq2gene function has the feasibility to assign non-exon regions to a range of neighboring genes besides the nearest one, thus facilitating the study of functional non-coding elements[2]. Then the gene2pathway summarizes gene-level measurements to pathway-level scores, comparing the quantity of significance for gene members within a pathway with those outside a pathway. -

ABCG1 (ABC8), the Human Homolog of the Drosophila White Gene, Is a Regulator of Macrophage Cholesterol and Phospholipid Transport
ABCG1 (ABC8), the human homolog of the Drosophila white gene, is a regulator of macrophage cholesterol and phospholipid transport Jochen Klucken*, Christa Bu¨ chler*, Evelyn Orso´ *, Wolfgang E. Kaminski*, Mustafa Porsch-Ozcu¨ ¨ ru¨ mez*, Gerhard Liebisch*, Michael Kapinsky*, Wendy Diederich*, Wolfgang Drobnik*, Michael Dean†, Rando Allikmets‡, and Gerd Schmitz*§ *Institute for Clinical Chemistry and Laboratory Medicine, University of Regensburg, 93042 Regensburg, Germany; †National Cancer Institute, Laboratory of Genomic Diversity, Frederick, MD 21702-1201; and ‡Departments of Ophthalmology and Pathology, Columbia University, Eye Research Addition, New York, NY 10032 Edited by Jan L. Breslow, The Rockefeller University, New York, NY, and approved November 3, 1999 (received for review June 14, 1999) Excessive uptake of atherogenic lipoproteins such as modified low- lesterol transport. Although several effector molecules have been density lipoprotein complexes by vascular macrophages leads to proposed to participate in macrophage cholesterol efflux (6, 9), foam cell formation, a critical step in atherogenesis. Cholesterol efflux including endogenous apolipoprotein E (10) and the cholesteryl mediated by high-density lipoproteins (HDL) constitutes a protective ester transfer protein (11), the detailed molecular mechanisms mechanism against macrophage lipid overloading. The molecular underlying cholesterol export in these cells have not yet been mechanisms underlying this reverse cholesterol transport process are characterized. currently not fully understood. To identify effector proteins that are Recently, mutations of the ATP-binding cassette (ABC) trans- involved in macrophage lipid uptake and release, we searched for porter ABCA1 gene have been causatively linked to familial HDL genes that are regulated during lipid influx and efflux in human deficiency and Tangier disease (12–14). -
Translocation of the ABC Transporter ABCD4 from the Endoplasmic
www.nature.com/scientificreports OPEN Translocation of the ABC transporter ABCD4 from the endoplasmic reticulum to Received: 31 December 2015 Accepted: 30 June 2016 lysosomes requires the escort Published: 26 July 2016 protein LMBD1 Kosuke Kawaguchi*, Takumi Okamoto*, Masashi Morita & Tsuneo Imanaka We previously demonstrated that ABCD4 does not localize to peroxisomes but rather, the endoplasmic reticulum (ER), because it lacks the NH2-terminal hydrophilic region required for peroxisomal targeting. It was recently reported that mutations in ABCD4 result in a failure to release vitamin B12 from lysosomes. A similar phenotype is caused by mutations in LMBRD1, which encodes the lysosomal membrane protein LMBD1. These findings suggested to us that ABCD4 translocated from the ER to lysosomes in association with LMBD1. In this report, it is demonstrated that ABCD4 interacts with LMBD1 and then localizes to lysosomes, and this translocation depends on the lysosomal targeting ability of LMBD1. Furthermore, endogenous ABCD4 was localized to both lysosomes and the ER, and its lysosomal localization was disturbed by knockout of LMBRD1. To the best of our knowledge, this is the first report demonstrating that the subcellular localization of the ABC transporter is determined by its association with an adaptor protein. The superfamily of ATP-binding cassette (ABC) transporters comprises membrane-bound proteins that catalyze the ATP-dependent transmembrane transport of a wide variety of substrates1. The human ABC transporter fam- ily currently comprises 49 members classified into seven subfamilies, A to G, based on structural organization and amino acid homology2,3. To date, four ABC proteins have been identified in mammals and classified into “subfamily D”4–7. -
Peroxisomal Disorders and Their Mouse Models Point to Essential Roles of Peroxisomes for Retinal Integrity
International Journal of Molecular Sciences Review Peroxisomal Disorders and Their Mouse Models Point to Essential Roles of Peroxisomes for Retinal Integrity Yannick Das, Daniëlle Swinkels and Myriam Baes * Lab of Cell Metabolism, Department of Pharmaceutical and Pharmacological Sciences, KU Leuven, 3000 Leuven, Belgium; [email protected] (Y.D.); [email protected] (D.S.) * Correspondence: [email protected] Abstract: Peroxisomes are multifunctional organelles, well known for their role in cellular lipid homeostasis. Their importance is highlighted by the life-threatening diseases caused by peroxisomal dysfunction. Importantly, most patients suffering from peroxisomal biogenesis disorders, even those with a milder disease course, present with a number of ocular symptoms, including retinopathy. Patients with a selective defect in either peroxisomal α- or β-oxidation or ether lipid synthesis also suffer from vision problems. In this review, we thoroughly discuss the ophthalmological pathology in peroxisomal disorder patients and, where possible, the corresponding animal models, with a special emphasis on the retina. In addition, we attempt to link the observed retinal phenotype to the underlying biochemical alterations. It appears that the retinal pathology is highly variable and the lack of histopathological descriptions in patients hampers the translation of the findings in the mouse models. Furthermore, it becomes clear that there are still large gaps in the current knowledge on the contribution of the different metabolic disturbances to the retinopathy, but branched chain fatty acid accumulation and impaired retinal PUFA homeostasis are likely important factors. Citation: Das, Y.; Swinkels, D.; Baes, Keywords: peroxisome; Zellweger; metabolism; fatty acid; retina M. Peroxisomal Disorders and Their Mouse Models Point to Essential Roles of Peroxisomes for Retinal Integrity. -

Coexpression of ATP-Binding Cassette Proteins ABCG5 and ABCG8 Permits Their Transport to the Apical Surface
Coexpression of ATP-binding cassette proteins ABCG5 and ABCG8 permits their transport to the apical surface Gregory A. Graf, … , Jonathan C. Cohen, Helen H. Hobbs J Clin Invest. 2002;110(5):659-669. https://doi.org/10.1172/JCI16000. Article Cardiology Mutations in either ATP-binding cassette (ABC) G5 or ABCG8 cause sitosterolemia, an autosomal recessive disorder of sterol trafficking. To determine the site of action of ABCG5 and ABCG8, we expressed recombinant, epitope-tagged mouse ABCG5 and ABCG8 in cultured cells. Both ABCG5 and ABCG8 underwent N-linked glycosylation. When either protein was expressed individually in cells, the N-linked sugars remained sensitive to Endoglycosidase H (Endo H). When ABCG5 and ABCG8 were coexpressed, the attached sugars were Endo H–resistant and neuraminidase-sensitive, indicating that the proteins were transported to the trans-Golgi complex. The mature, glycosylated forms of ABCG5 and ABCG8 coimmunoprecipitated, consistent with heterodimerization of these two proteins. The Endo H–sensitive forms of ABCG5 and ABCG8 were confined to the endoplasmic reticulum (ER), whereas the mature forms were present in non-ER fractions in cultured hepatocytes. Immunoelectron microscopy revealed ABCG5 and ABCG8 on the plasma membrane of these cells. In polarized WIF-B cells, recombinant ABCG5 localized to the apical (canalicular) membrane when coexpressed with ABCG8, but not when expressed alone. To our knowledge this is the first direct demonstration that trafficking of an ABC half-transporter to the cell surface requires the presence of its dimerization partner. Find the latest version: https://jci.me/16000/pdf Coexpression of ATP-binding cassette See the related Commentary beginning on page 605. -

Transcriptional and Post-Transcriptional Regulation of ATP-Binding Cassette Transporter Expression
Transcriptional and Post-transcriptional Regulation of ATP-binding Cassette Transporter Expression by Aparna Chhibber DISSERTATION Submitted in partial satisfaction of the requirements for the degree of DOCTOR OF PHILOSOPHY in Pharmaceutical Sciences and Pbarmacogenomies in the Copyright 2014 by Aparna Chhibber ii Acknowledgements First and foremost, I would like to thank my advisor, Dr. Deanna Kroetz. More than just a research advisor, Deanna has clearly made it a priority to guide her students to become better scientists, and I am grateful for the countless hours she has spent editing papers, developing presentations, discussing research, and so much more. I would not have made it this far without her support and guidance. My thesis committee has provided valuable advice through the years. Dr. Nadav Ahituv in particular has been a source of support from my first year in the graduate program as my academic advisor, qualifying exam committee chair, and finally thesis committee member. Dr. Kathy Giacomini graciously stepped in as a member of my thesis committee in my 3rd year, and Dr. Steven Brenner provided valuable input as thesis committee member in my 2nd year. My labmates over the past five years have been incredible colleagues and friends. Dr. Svetlana Markova first welcomed me into the lab and taught me numerous laboratory techniques, and has always been willing to act as a sounding board. Michael Martin has been my partner-in-crime in the lab from the beginning, and has made my days in lab fly by. Dr. Yingmei Lui has made the lab run smoothly, and has always been willing to jump in to help me at a moment’s notice. -

Identification of Common Gene Networks Responsive To
Cancer Gene Therapy (2014) 21, 542–548 © 2014 Nature America, Inc. All rights reserved 0929-1903/14 www.nature.com/cgt ORIGINAL ARTICLE Identification of common gene networks responsive to radiotherapy in human cancer cells D-L Hou1, L Chen2, B Liu1, L-N Song1 and T Fang1 Identification of the genes that are differentially expressed between radiosensitive and radioresistant cancers by global gene analysis may help to elucidate the mechanisms underlying tumor radioresistance and improve the efficacy of radiotherapy. An integrated analysis was conducted using publicly available GEO datasets to detect differentially expressed genes (DEGs) between cancer cells exhibiting radioresistance and cancer cells exhibiting radiosensitivity. Gene Ontology (GO) enrichment analyses, Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway analysis and protein–protein interaction (PPI) networks analysis were also performed. Five GEO datasets including 16 samples of radiosensitive cancers and radioresistant cancers were obtained. A total of 688 DEGs across these studies were identified, of which 374 were upregulated and 314 were downregulated in radioresistant cancer cell. The most significantly enriched GO terms were regulation of transcription, DNA-dependent (GO: 0006355, P = 7.00E-09) for biological processes, while those for molecular functions was protein binding (GO: 0005515, P = 1.01E-28), and those for cellular component was cytoplasm (GO: 0005737, P = 2.81E-26). The most significantly enriched pathway in our KEGG analysis was Pathways in cancer (P = 4.20E-07). PPI network analysis showed that IFIH1 (Degree = 33) was selected as the most significant hub protein. This integrated analysis may help to predict responses to radiotherapy and may also provide insights into the development of individualized therapies and novel therapeutic targets. -

Whole-Exome Sequencing Identifies Novel Mutations in ABC Transporter
Liu et al. BMC Pregnancy and Childbirth (2021) 21:110 https://doi.org/10.1186/s12884-021-03595-x RESEARCH ARTICLE Open Access Whole-exome sequencing identifies novel mutations in ABC transporter genes associated with intrahepatic cholestasis of pregnancy disease: a case-control study Xianxian Liu1,2†, Hua Lai1,3†, Siming Xin1,3, Zengming Li1, Xiaoming Zeng1,3, Liju Nie1,3, Zhengyi Liang1,3, Meiling Wu1,3, Jiusheng Zheng1,3* and Yang Zou1,2* Abstract Background: Intrahepatic cholestasis of pregnancy (ICP) can cause premature delivery and stillbirth. Previous studies have reported that mutations in ABC transporter genes strongly influence the transport of bile salts. However, to date, their effects are still largely elusive. Methods: A whole-exome sequencing (WES) approach was used to detect novel variants. Rare novel exonic variants (minor allele frequencies: MAF < 1%) were analyzed. Three web-available tools, namely, SIFT, Mutation Taster and FATHMM, were used to predict protein damage. Protein structure modeling and comparisons between reference and modified protein structures were performed by SWISS-MODEL and Chimera 1.14rc, respectively. Results: We detected a total of 2953 mutations in 44 ABC family transporter genes. When the MAF of loci was controlled in all databases at less than 0.01, 320 mutations were reserved for further analysis. Among these mutations, 42 were novel. We classified these loci into four groups (the damaging, probably damaging, possibly damaging, and neutral groups) according to the prediction results, of which 7 novel possible pathogenic mutations were identified that were located in known functional genes, including ABCB4 (Trp708Ter, Gly527Glu and Lys386Glu), ABCB11 (Gln1194Ter, Gln605Pro and Leu589Met) and ABCC2 (Ser1342Tyr), in the damaging group. -

Expression Profiling of ATP-Binding Cassette Transporters in Childhood T-Cell Acute Lymphoblastic Leukemia
1986 Expression profiling of ATP-binding cassette transporters in childhood T-cell acute lymphoblastic leukemia Thomas Efferth,1 Jean-Pierre Gillet,2 of both transporters. As a consequence, a significant Axel Sauerbrey,3 Felix Zintl,4 Vincent Bertholet,5 sensitization of cells to cytostatic drugs was achieved. In Franc¸oise de Longueville,5 Jose Remacle,6 conclusion, ABCA2 and ABCA3 are expressed in many and Daniel Steinbach4 T-ALL and contribute to drug resistance. [Mol Cancer Ther 2006;5(8):1986–94] 1German Cancer Research Center, Heidelberg, Germany; 2Laboratory of Cell Biology, National Cancer Institute, NIH, Introduction Bethesda, Maryland; 3Helios Children’s Hospital, Erfurt, Germany; 4Children’s Hospital, University of Jena, Jena, Germany; Although cancer therapy for childhood T cell acute 5Department of Biology, University of Namur; and 6Eppendorf lymphoblastic leukemia (T-ALL) has remarkably improved Array Technologies, Namur, Belgium during the past two decades, and normal life expectancy is a reality for many patients, a considerable number Abstract of patients cannot permanently be cured. In the majority of children suffering from T-ALL, remissions can be achieved A major issue in the treatment of T-cell acute lympho- by chemotherapy. Nevertheless, f25% of the patients blastic leukemia (T-ALL) is resistance to chemotherapeutic develop relapses. One major reason is the development drugs. Multidrug resistance can be caused by ATP-binding of drug resistance. In patients with a T cell immunophe- cassette (ABC) transporters. The majority of these notype (T-ALL), drug resistance is even more commonly proteins have not yet been examined in T-ALL. Using a encountered. newly developed microarray for the simultaneous quanti- The expression of one drug resistance gene, the multi- fication of 38 ABC transporter genes, we observed a drug resistance gene, MDR1,anditsgeneproduct, ABCA2/ABCA3 consistent overexpression of in clinical P-glycoprotein, has been well documented in leukemia. -

Categorization and Classification of Different ABCA3 Variants Causing Interstitial Lung Disease
Categorization and classification of different ABCA3 variants causing interstitial lung disease Dissertation der Mathematisch-Naturwissenschaftlichen Fakultät der Eberhard Karls Universität Tübingen zur Erlangung des Doktorgrades Doktor der Naturwissenschaften (Dr. rer. nat.) vorgelegt von Thomas Wittmann aus Neumarkt in der Oberpfalz, Deutschland Tübingen 2016 Gedruckt mit Genehmigung der Mathematisch-Naturwissenschaftlichen Fakultät der Eberhard Karls Universität Tübingen. Tag der mündlichen Qualifikation: 15.07.2016 Dekan: Prof. Dr. Wolfgang Rosenstiel 1. Berichterstatter: Prof. Dr. Dominik Hartl 2. Berichterstatter: Prof. Dr. Andreas Peschel Table of contents Table of contents Table of contents ..........................................................................................................I List of tables.................................................................................................................II List of figures................................................................................................................II Abbreviations ..............................................................................................................III Summary..................................................................................................................... V Zusammenfassung .................................................................................................... VI Publications............................................................................................................. -

Role of Genetic Variation in ABC Transporters in Breast Cancer Prognosis and Therapy Response
International Journal of Molecular Sciences Article Role of Genetic Variation in ABC Transporters in Breast Cancer Prognosis and Therapy Response Viktor Hlaváˇc 1,2 , Radka Václavíková 1,2, Veronika Brynychová 1,2, Renata Koževnikovová 3, Katerina Kopeˇcková 4, David Vrána 5 , Jiˇrí Gatˇek 6 and Pavel Souˇcek 1,2,* 1 Toxicogenomics Unit, National Institute of Public Health, 100 42 Prague, Czech Republic; [email protected] (V.H.); [email protected] (R.V.); [email protected] (V.B.) 2 Biomedical Center, Faculty of Medicine in Pilsen, Charles University, 323 00 Pilsen, Czech Republic 3 Department of Oncosurgery, Medicon Services, 140 00 Prague, Czech Republic; [email protected] 4 Department of Oncology, Second Faculty of Medicine, Charles University and Motol University Hospital, 150 06 Prague, Czech Republic; [email protected] 5 Department of Oncology, Medical School and Teaching Hospital, Palacky University, 779 00 Olomouc, Czech Republic; [email protected] 6 Department of Surgery, EUC Hospital and University of Tomas Bata in Zlin, 760 01 Zlin, Czech Republic; [email protected] * Correspondence: [email protected]; Tel.: +420-267-082-711 Received: 19 November 2020; Accepted: 11 December 2020; Published: 15 December 2020 Abstract: Breast cancer is the most common cancer in women in the world. The role of germline genetic variability in ATP-binding cassette (ABC) transporters in cancer chemoresistance and prognosis still needs to be elucidated. We used next-generation sequencing to assess associations of germline variants in coding and regulatory sequences of all human ABC genes with response of the patients to the neoadjuvant cytotoxic chemotherapy and disease-free survival (n = 105). -

ABC Transporter Expression Profiling After Ischemic Reperfusion Injury in Mouse Kidney M Huls1, JJMW Van Den Heuvel1, HBPM Dijkman2, FGM Russel1 and R Masereeuw1
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector original article http://www.kidney-international.org & 2006 International Society of Nephrology ABC transporter expression profiling after ischemic reperfusion injury in mouse kidney M Huls1, JJMW van den Heuvel1, HBPM Dijkman2, FGM Russel1 and R Masereeuw1 1Department of Pharmacology and Toxicology, Nijmegen Centre for Molecular Life Sciences, Radboud University Nijmegen Medical Centre, Nijmegen, The Netherlands and 2Department of Pathology, Radboud University Nijmegen Medical Centre, Nijmegen, The Netherlands Renal ATP binding cassette (ABC) transporters have an Members of the ATP binding cassette (ABC) superfamily of important role in the elimination of metabolic waste transporters are expressed in almost all tissues and cells where products and compounds foreign to the body. The kidney many of them are involved in the cellular defense against has the ability to tightly control the expression of these efflux endogenous and exogenous xenobiotics, and their meta- transporters to maintain homeostasis, and as a major bolites.1,2 Their overexpression in tumor cells is associated mechanism of adaptation to environmental stress. In the with multidrug resistance, which is a major complication for present study, we investigated the expression of 45 ABC successful cancer chemotherapy. The transport proteins transporter genes in the mouse kidney under basal couple ATP hydrolysis to the transport of specific substrates. conditions, after induction of ischemia and after In excretory organs, like the kidney, ABC transporters have regeneration. Two days after clamping, mice showed a 76% an important role in the elimination of metabolic waste decrease in renal creatinine clearance, which improved products and compounds foreign to the body.