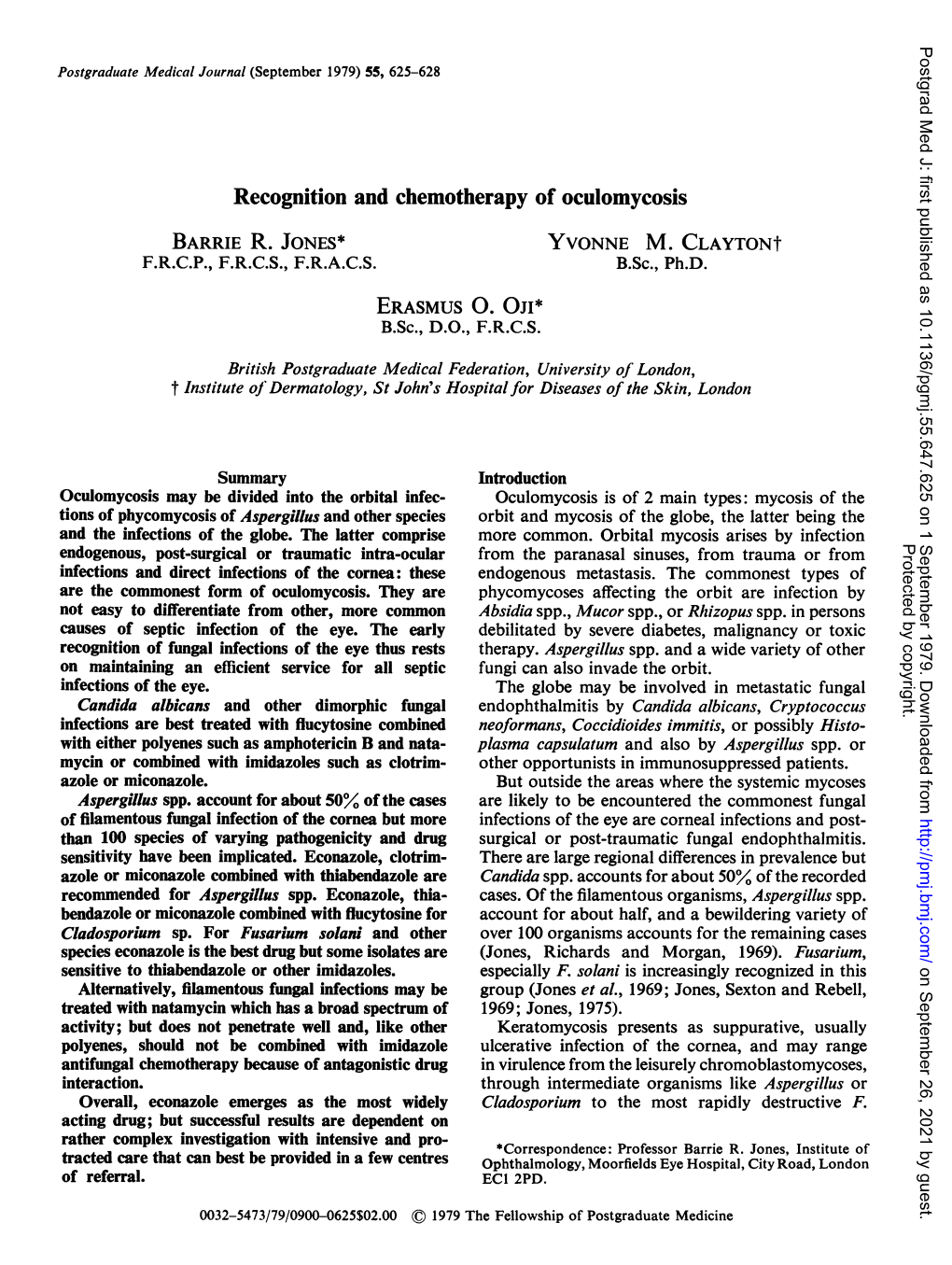
Recognition and Chemotherapy of Oculomycosis BARRIE R
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Topical and Systemic Antifungal Therapy for Chronic Rhinosinusitis (Protocol)
CORE Metadata, citation and similar papers at core.ac.uk Provided by University of East Anglia digital repository Cochrane Database of Systematic Reviews Topical and systemic antifungal therapy for chronic rhinosinusitis (Protocol) Head K, Sacks PL, Chong LY, Hopkins C, Philpott C Head K, Sacks PL, Chong LY, Hopkins C, Philpott C. Topical and systemic antifungal therapy for chronic rhinosinusitis. Cochrane Database of Systematic Reviews 2016, Issue 11. Art. No.: CD012453. DOI: 10.1002/14651858.CD012453. www.cochranelibrary.com Topical and systemic antifungal therapy for chronic rhinosinusitis (Protocol) Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd. TABLE OF CONTENTS HEADER....................................... 1 ABSTRACT ...................................... 1 BACKGROUND .................................... 1 OBJECTIVES ..................................... 3 METHODS ...................................... 3 ACKNOWLEDGEMENTS . 8 REFERENCES ..................................... 9 APPENDICES ..................................... 10 CONTRIBUTIONSOFAUTHORS . 25 DECLARATIONSOFINTEREST . 26 SOURCESOFSUPPORT . 26 NOTES........................................ 26 Topical and systemic antifungal therapy for chronic rhinosinusitis (Protocol) i Copyright © 2016 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd. [Intervention Protocol] Topical and systemic antifungal therapy for chronic rhinosinusitis Karen Head1, Peta-Lee Sacks2, Lee Yee Chong1, Claire Hopkins3, Carl Philpott4 1UK Cochrane Centre, -

Title 16. Crimes and Offenses Chapter 13. Controlled Substances Article 1
TITLE 16. CRIMES AND OFFENSES CHAPTER 13. CONTROLLED SUBSTANCES ARTICLE 1. GENERAL PROVISIONS § 16-13-1. Drug related objects (a) As used in this Code section, the term: (1) "Controlled substance" shall have the same meaning as defined in Article 2 of this chapter, relating to controlled substances. For the purposes of this Code section, the term "controlled substance" shall include marijuana as defined by paragraph (16) of Code Section 16-13-21. (2) "Dangerous drug" shall have the same meaning as defined in Article 3 of this chapter, relating to dangerous drugs. (3) "Drug related object" means any machine, instrument, tool, equipment, contrivance, or device which an average person would reasonably conclude is intended to be used for one or more of the following purposes: (A) To introduce into the human body any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (B) To enhance the effect on the human body of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (C) To conceal any quantity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; or (D) To test the strength, effectiveness, or purity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state. (4) "Knowingly" means having general knowledge that a machine, instrument, tool, item of equipment, contrivance, or device is a drug related object or having reasonable grounds to believe that any such object is or may, to an average person, appear to be a drug related object. -

United States Patent Office Patented Apr
3,505,222 United States Patent Office Patented Apr. 7, 1970 1. 2 3,505,222 product of a mercaptain with sulfur trioxide. Their metal LUBRICANT COMPOSITIONS salts are represented by the formula: Leonard M. Niebylski, Birmingham, Mich, assignor to O Ethyl Corporation, New York, N.Y., a corporation of Virginia (R-S-S-0--M No Drawing. Filed Mar. 29, 1967, Ser. No. 626,701 5 s (I) Int. C. C10m 5/14, 3/18, 7/36 wherein R is a hydrocarbon radical containing from 1 U.S. C. 252-17 2 Claims to about 30 carbon atoms, M is a metal, and n is the valence of metal M. For example, when M is the monova 0. lent sodium ion, n is 1. ABSTRACT OF THE DISCLOSURE The radical R can be an alkyl, cycloalkyl, aralkyl, The extreme pressure wear properties of base lubri alkaryl, or aryl radical. The radicals may contain other cants including water, hydrocarbons, polyesters, silicones, nonhydrocarbon substituents such as chloro, bromo, iodo, polyethers and halocarbons is enhanced by the addition fluoro, nitro, hydroxyl, nitrile, isocyanate, carboxyl, car of a synergistic mixture of a thiosulfate compound and 15 bonyl, and the like. a lead compound. The useful metals are all those capable of forming Bunte salts. Preferred metals are those previously listed as suitable for forming metal thiosulfates. Of these, the Background more preferred metals are sodium and lead, and lead is 20 the most preferred metal in the Bunte salts. This invention relates to improved lubricant composi Examples of useful Bunte salts include: tions. -

University of California Riverside
UNIVERSITY OF CALIFORNIA RIVERSIDE Natamycin, a New Postharvest Biofungicide: Toxicity to Major Decay Fungi, Efficacy, and Optimized Usage Strategies A Dissertation submitted in partial satisfaction of the requirements for the degree of Doctor of Philosophy in Plant Pathology by Daniel Sungen Chen September 2020 Dissertation Committee: Dr. James E. Adaskaveg, Chairperson Dr. Michael E. Stanghellini Dr. Alexander I. Putman Copyright by Daniel Sungen Chen 2020 The Dissertation of Daniel Sungen Chen is approved: Committee Chairperson University of California, Riverside AKNOWLEDGEMENTS Foremost, I thank my mentor Dr. James E. Adaskaveg for accepting me into his research program and teaching me the intricacies of the field of postharvest plant pathology and preparing me for a bright career ahead. His knowledge of the field is unmatched. A special thanks goes out to Dr. Helga Förster, whose expertise and attention to detail has helped me out tremendously in my research and writings. I thank my dissertation committee members, Dr. Michael Stanghellini and Dr. Alexander Putman, for their time spent reviewing my dissertation and their guidance during the pursuit of my doctoral degree. Special thanks also go out to my lab members Dr. Rodger Belisle, Dr. Wei Hao, Dr. Kevin Nguyen, and Nathan Riley for their companionship and much appreciated help with my projects. I would also like to thank my former laboratory members, Dr. Stacey Swanson and Dr. Morgan Thai for their guidance and help during the early years of my graduate program. Thanks go out to Dr. Lingling Hou, Dr. Yong Luo, and Doug Cary for their assistance with performing experimental packingline studies at the Kearney Agricultural Research and Extension Center. -

NATACYN® (Natamycin Ophthalmic Suspension) 5% Sterile
NATACYN® (natamycin ophthalmic suspension) 5% Sterile DESCRIPTION: NATACYN® (natamycin ophthalmic suspension) 5% is a sterile, antifungal drug for topical ophthalmic administration. Each mL of NATACYN® (natamycin ophthalmic suspension) contains: Active: natamycin 5% (50 mg). Preservative: benzalkonium chloride 0.02%. Inactive: sodium hydroxide and/or hydrochloric acid (neutralized to adjust the pH), purified water. The active ingredient is represented by the chemical structure: Established Name: Natamycin Molecular Formula: C33H47NO13 Molecular Weight: 665.73 g/mol Chemical Name: Stereoisomer of 22-[(3-amino-3,6-dideoxy- β-D-mannopyranosyl)oxy]-1,3,26- trihydroxy-12-methyl-10-oxo-6,11,28-trioxatricyclo[22.3.1.05,7] octacosa-8,14,16,18,20-pentaene-25- carboxylic acid. Other: Pimaricin The pH range is 5.0-7.5. CLINICAL PHARMACOLOGY: Natamycin is a tetraene polyene antibiotic derived from Streptomyces natalensis. It possesses in vitro activity against a variety of yeast and filamentous fungi, including Candida, Aspergillus, Cephalosporium, Fusarium and Penicillium. The mechanism of action appears to be through binding of the molecule to the sterol moiety of the fungal cell membrane. The polyenesterol complex alters the permeability of the membrane to produce depletion of essential cellular constituents. Although the activity against fungi is dose-related, natamycin is predominantly fungicidal. Natamycin is not effective in vitro against gram-positive or gram- negative bacteria. Topical administration appears to produce effective concentrations of natamycin within the corneal stroma but not in intraocular fluid. Systemic absorption should not be expected following topical administration of NATACYN® (natamycin ophthalmic suspension) 5%. As with other polyene antibiotics, absorption from the gastrointestinal tract is very poor. -

Infectious Keratitis: Short Answers
Q Infectious keratitis: Short answers What is the #1 bacterium in CL-related K ulcer? A Infectious keratitis: Short answers What is the #1 bacterium in CL-related K ulcer? Pseudomonas Infectious keratitis: Short answers Pseudomonas corneal ulcer associated with CL wear Q Infectious keratitis: Short answers What is the #1 bacterium in CL-related K ulcer? Pseudomonas What is the #1 risk factor for Acanthamoeba keratitis? A Infectious keratitis: Short answers What is the #1 bacterium in CL-related K ulcer? Pseudomonas What is the #1 risk factor for Acanthamoeba keratitis? CL wear Infectious keratitis: Short answers Acanthamoeba keratitis associated with CL wear Q Infectious keratitis: Short answers What is the #1 bacterium in CL-related K ulcer? Pseudomonas What is the #1 risk factor for Acanthamoeba keratitis? CL wear What are the three main culprits in fungal keratitis? What is the topical antifungal of choice for each? Fusarium:fungus 1 Topical…natamycin Aspergillisfungus 2 and Candida:fungus 3 A Infectious keratitis: Short answers What is the #1 bacterium in CL-related K ulcer? Pseudomonas What is the #1 risk factor for Acanthamoeba keratitis? CL wear What are the three main culprits in fungal keratitis? What is the topical antifungal of choice for each? Candida: Topical…natamycin Aspergillis and Fusarium: Q Infectious keratitis: Short answers What is the #1 bacterium in CL-related K ulcer? Pseudomonas What is the #1 risk factor for Acanthamoeba keratitis? CL wear What are the three main culprits in fungal keratitis? -

Updates in Ocular Antifungal Pharmacotherapy: Formulation and Clinical Perspectives
Current Fungal Infection Reports (2019) 13:45–58 https://doi.org/10.1007/s12281-019-00338-6 PHARMACOLOGY AND PHARMACODYNAMICS OF ANTIFUNGAL AGENTS (N BEYDA, SECTION EDITOR) Updates in Ocular Antifungal Pharmacotherapy: Formulation and Clinical Perspectives Ruchi Thakkar1,2 & Akash Patil1,2 & Tabish Mehraj1,2 & Narendar Dudhipala1,2 & Soumyajit Majumdar1,2 Published online: 2 May 2019 # Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract Purpose of Review In this review, a compilation on the current antifungal pharmacotherapy is discussed, with emphases on the updates in the formulation and clinical approaches of the routinely used antifungal drugs in ocular therapy. Recent Findings Natamycin (Natacyn® eye drops) remains the only approved medication in the management of ocular fungal infections. This monotherapy shows therapeutic outcomes in superficial ocular fungal infections, but in case of deep-seated mycoses or endophthalmitis, successful therapeutic outcomes are infrequent, as a result of which alternative therapies are sought. In such cases, amphotericin B, azoles, and echinocandins are used off-label, either in combination with natamycin or with each other (frequently) or as standalone monotherapies, and have provided effective therapeutic outcomes. Summary In recent times, amphotericin B, azoles, and echinocandins have come to occupy an important niche in ocular antifungal pharmacotherapy, along with natamycin (still the preferred choice in most clinical cases), in the management of ocular fungal infections. -

Magnetic Graphene Oxide Modified by Chloride Imidazole Ionic Liquid For
RSC Advances View Article Online PAPER View Journal | View Issue Magnetic graphene oxide modified by chloride imidazole ionic liquid for the high-efficiency Cite this: RSC Adv.,2017,7,9079 adsorption of anionic dyes† Huan Wangab and Yinmao Wei*a Magnetic graphene oxide modified with 1-amine-3-methyl imidazole chloride ionic liquid (LI-MGO) was prepared through chemical co-precipitation and modified using 1-amine-3-imidazolium chloride ionic liquid. The as-prepared LI-MGO was characterized using X-ray diffraction (XRD), transmission electron microscopy (TEM) and Fourier transform infrared spectrometry (FT-IR). The adsorption properties were evaluated through adsorption experiments with two kinds of anionic dyes, orange IV (OIV) and glenn black R (GR) and two kinds of cationic dyes, acridine orange (AO) and crystal violet (CV). The results indicated that the adsorption data fitted the Langmuir isotherm and followed pseudo-second-order kinetics. The maximum adsorption capacities for GR, OIV, AO and CV were 588.24, 57.37, 132.80 and Received 29th November 2016 À1 Creative Commons Attribution 3.0 Unported Licence. 69.44 mg g at 298 K, respectively. LI-MGO has better selective adsorption for anionic dyes than Accepted 17th January 2017 magnetic graphene oxide (MGO) due to electrostatic interactions. Moreover, the LI-MGO adsorbent can DOI: 10.1039/c6ra27530c be magnetic separated and is easy to prepare. It demonstrated that LI-MGO would have great potential rsc.li/rsc-advances as an efficient environmentally friendly adsorbent for the removal of anionic -

Natamycin Ophthalmic Suspension)5% Sterile
NDA 50-514/S-009 Page 3 Natacyn® (natamycin ophthalmic suspension)5% Sterile DESCRIPTION: NATACYN® (natamycin ophthalmic suspension) 5% is a sterile, antifungal drug for topical ophthalmic administration. Each mL of the suspension contains: Active: natamycin 5% (50mg). Preservative: benzalkonium chloride 0.02%. Inactive: sodium hydroxide and/or hydrochloric acid (neutralized to adjust the pH), purified water. The active ingredient is represented by the chemical structure: Established name: Natamycin Chemical Structure Molecular Formula: C33H47NO13 Molecular Weight: 665.73 Chemical name: Stereoisomer of 22-[(3-amino-3,6-dideoxy- β-D-mannopyranosyl)oxy]-1,3,26 trihydroxy-12- methyl-10-oxo-6,11,28- trioxatricyclo[22.3.1.05,7] octacosa-8,14,16,18,20-pentaene-25-carboxylic acid. Other: Pimaricin The pH range is 5.0 – 7.5. CLINICAL PHARMACOLOGY: Natamycin is a tetraene polyene antibiotic derived from Streptomyces natalensis. It possesses in vitro activity against a variety of yeast and filamentous fungi, including Candida, Aspergillus, Cephalosporium, Fusarium and Penicillium. The mechanism of action appears to be through binding of the molecule to the sterol moiety of the fungal cell membrane. The polyenesterol complex alters the permeability of the membrane to produce depletion of essential cellular constituents. Although the activity against fungi is dose-related, natamycin is predominantly fungicidal.* Natamycin is not effective in vitro against gram-positive or gram-negative bacteria. Topical administration appears to produce effective concentrations of natamycin within the corneal stroma but not in intraocular fluid. Systemic absorption should not be expected following topical administration of NATACYN® (natamycin ophthalmic suspension) 5%. As with other polyene antibiotics, absorption from the gastrointestinal tract is very poor. -
Synthesis of Photoreactive Imidazole Derivatives and Thermal Curing Reaction of Epoxy Resins Catalyzed by Photo-Generated Imidazole
Polymer Journal, Vol. 29, No. 5, pp 450-456 (1997) Synthesis of Photoreactive Imidazole Derivatives and Thermal Curing Reaction of Epoxy Resins Catalyzed by Photo-Generated Imidazole Tadatomi NrsHIKUBO,t Atsushi KAMEYAMA, and Yoshiyasu TOYA Department of' Applied Chemistry, Faculty of Engineering, Kanagawa University, Rokkakubashi, Kanagawa-ku, Yokohama, 221 Japan (Received November 6, 1996) ABSTRACT: Photoreactive blocked imidazoles such as N-(2-nitrobenzyloxycarbonyl)imidazole (2-NBCI), N-(3-nitro benzyloxycarbonyl)imidazole (3-NBCI), N-( 4-nitrobenzyloxycarbonyl)imidazole (4- NBCI), N-( 4-chloro-2-nitro benzyloxy carbonyl )imidazole (CNBCI), N-(5-methyl-2-nitrobenzyloxycarbonyl)imidazole (MNBCI), and N-(4,5-dimethoxy-2-ni trobenzyloxycarbonyl)imidazole (DNBCI) were synthesized in good yields by reactions of N,N'-carbonyldiimidazole (CDI) with corresponding benzyl alcohols. The prepared 2-NBCI decomposed smoothly to produce imidazole by UV-irradiation in tetrahydrofuran (THF) solution or poly(methyl methacrylate) (PMMA) film. Rates of photolysis of DNBCI, MNBCI and CNBCI were higher than that of 2-NBCI in PMMA film, although the rates of 3-NBCI and 4-NBCI were slower than that of 2-NBCI in PMMA film under the same conditions. Thermal curing reactions of epoxy resins and poly(glycidyl methacrylate-co-methyl methacrylate) [P(GMA55-MMA45)] using photo-generated imidazole were examined at I00-160°C. The ring opening reaction of epoxide groups, confirmed by IR spectra, in epoxy resins and P(GMA55-MMA45) proceeded smoothly by catalysis of the photo-generated imidazole. KEY WORDS Synthesis of Blocked Imidazole /Photo-Generation/ Imidazole / Thermal Curing Reaction / Epoxy Resin/ Poly(glycidyl methacrylate-co-methyl methac!ylate) / Epoxy resins are typical thermo-setting resins, and Tsunooka et al. -

Antifungal Drugs
Antifungal Drugs Antifungal or antimycotic drugs are those agents used to treat diseases caused by fungus. Fungicides are drugs which destroy fungus and fungistatic drugs are those which prevent growth and multiplication of fungi. Collectively these drugs are often referred to as antimycotic or antifungal drugs. General characteristics of fungus: Fungi of medical significance are of two groups: Yeast Unicellular (Candida, Crytococcus) Molds Multicellular; filamentous consist of hyphae (Aspergillus, Microsporum, Trichophyton) They are eukaryotic i.e. they have well defined nucleus and other nuclear materials. They are made of thin threads called hyphae. The hyphae have a cell wall (like plant cells) made of a material called chitin. The hyphae are often multinucleate. They do not have chlorophyll, can’t make own food by photosynthesis, therefore derive nutrients by means of saprophytic or parasitic existence. Cell membrane is made up of ergosterol. Types of fungal infections: Fungal infections are termed as mycoses and in general can be divided into: Superficial infections: Affecting skin, nails, scalp or mucous membranes; e.g. Tinea versicolor Dermatophytosis: Fungi that affect keratin layer of skin, hair and nail; e.g. Tinea pedis, rign worm infection. Candidiasis: Yeast infections caused by (Malassezia pachydermatis), oral thrush (oral candidiasis), vulvo-vaginitis, nail infection. Systemic/Deep infections: Affecting deeper tissues and organ they usually affect lungs, heart and brain leading to pneumonia, endocarditis and meningitis. Systemic infections are associated with immunocompromised patients, these diseases are serious and often life threatening due to the organ involved. Some of the serious systemic fungal infections in man are candidiasis, cryptococcal meningitis, pulmonary aspergillosis. -

Pharmaceuticals As Environmental Contaminants
PharmaceuticalsPharmaceuticals asas EnvironmentalEnvironmental Contaminants:Contaminants: anan OverviewOverview ofof thethe ScienceScience Christian G. Daughton, Ph.D. Chief, Environmental Chemistry Branch Environmental Sciences Division National Exposure Research Laboratory Office of Research and Development Environmental Protection Agency Las Vegas, Nevada 89119 [email protected] Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada Why and how do drugs contaminate the environment? What might it all mean? How do we prevent it? Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada This talk presents only a cursory overview of some of the many science issues surrounding the topic of pharmaceuticals as environmental contaminants Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada A Clarification We sometimes loosely (but incorrectly) refer to drugs, medicines, medications, or pharmaceuticals as being the substances that contaminant the environment. The actual environmental contaminants, however, are the active pharmaceutical ingredients – APIs. These terms are all often used interchangeably Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada Office of Research and Development Available: http://www.epa.gov/nerlesd1/chemistry/pharma/image/drawing.pdfNational