Surgical Specialties EUHM Surgical Specialties EUHM
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

Guidance for Image-Guided Procedures and Diagnostic Imaging Under Anesthesia During the COVID-19 Pandemic
Guidance for Image-Guided Procedures and Diagnostic Imaging under Anesthesia During the COVID-19 Pandemic Approved: 4/24/20 Revision: 5/7/20 – revised timing of COVID-19 testing for inpatients , Tables 1-4 Last Revision: 8/9/20 – revised timing of COVID-19 testing for asymptomatic pediatric patients, updated permissive use of N95s/PAPRs for aerosol-generating procedures in patients with negative tests, addition of COVID-19 (exposed) flag to guidance Background: This document provides guidance for the management of patients and facilities during image-guided interventions and diagnostic imaging performed under anesthesia in the Department of Radiology and Biomedical Imaging. This document represents an update to prior guidance published 5/7/20 and maintains alignment with anesthesia and perioperative practice at UCSF and national standards. Several important concepts underpin these guidelines. These include: 1) asymptomatic patients may be sources of SARS-CoV-2 disease transmission, 2) disease transmission may occur by aerosol inhalation in addition to droplet spread, 3) certain surgeries and procedures carry higher risk than others for disease transmission to healthcare workers due to aerosolization of virus, and 4) intubation, extubation, and certain forms of respiratory support are aerosol-generating. General information to be familiar with and new updates include: • COVID-19 PCR test results: Based on current estimates of COVID-19 prevalence among asymptomatic patients in San Francisco and surrounding areas and the performance of the UCSF RT-PCR test, the likelihood is very high that a patient with a negative test result does not have COVID-19 infection (~99.7% negative predictive value) (see Appendix A). -

Interventional Radiology
Patient Safety Framework for Mitigating Risk in Interventional Radiology RECOMMENDATIONS OF THE INTERVENTIONAL RADIOLOGY TASK FORCE Created: 2017 TABLE OF CONTENTS Executive Summary ........................................................................... 1 Introduction ..................................................................................... 3 Definitions .......................................................................................4 1. Introduction of New/Rare Procedures/Technologies ........................ 5 2. Pre-assessment & Clinical Decision-making ................................. 6 3. Staffing ....................................................................................... 9 4. Communications & Hand-Offs ................................................... 10 5. Production Issues ........................................................................12 6. Institutional & Executive Leadership Issues ..................................13 7. Emerging Issue: Hybrid Rooms .................................................... 15 Appendix: Interventional Radiology WHO Safety Checklist .................... 16 ABOUT THIS DOCUMENT The recommendations for Patient Safety Framework for Mitigating Risk in Interventional Radiology were developed under the auspices of the Academic Medical Center Patient Safety Organization (AMC PSO) Interventional Radiology Task Force. These consensus recommendations are for informational purposes only and should not be construed or relied upon as a standard of care. The AMC PSO recommends -

Medical Staff Rules and Regulations Page 1 of 49
NWH Medical Staff Rules and Regulations Page 1 of 49 Rules and Regulations of THE MEDICAL STAFF OF NORTHERN WESTCHESTER HOSPITAL Approved by the Medical Board on December 4, 2006 Approved by the Governing Board on January 25, 2007 Revisions: General - Medical Board: 06/07; 03/08; 10/08; 07/10; 9/10; 07/12; 01/13; 11/13 04/14; 01/15 BOT: 06/07; 04/08; 10/08; 07/10; 9/10; 07/12; 01/13; 12/13; 05/14 Anesthesiology – Medical Board: 02/09; 09/09; 01/10; 05/11; 04/12; 10/14 BOT: 04/09; 09/09; 01/10; 05/11; 04/12; 10/14 Emergency Medical Board: 09/07; 05/08; 03/09; 04/10; 12/10; 10/11; 12/12; Medicine - 02/13; 11/13; 01/15 BOT: 10/07; 05/08; 04/09; 05/10; 12/10; 10/11; 12/12; 03/13; 12/13 Medicine – Medical Board: 10/08; 01/10; 11/13 BOT: 10/08; 01/10; 12/13 Obstetrics & Medical Board: 05/08; 10/08; 04/12; 06/14 Gynecology - BOT: 05/08; 10/08; 04/12; 06/14 Pathology - Medical Board: 03/12 BOT: 03/12 Pediatrics – Medical Board: 05/08; 06/11 BOT: 05/08; 06/11 Psychiatry – Medical Board: 09/08; 03/13; 11/13 BOT: 09/08; 03/13; 12/13 Surgical Services – Medical Board: 09/08; 01/10; 12/10; 11/11; 04/12; 06/12; 02/13; 11/13 BOT: 09/08; 01/10; 12/10; 12/11; 04/12; 07/12; 03/13; 12/13 NWH Medical Staff Rules and Regulations Page 2 of 49 GENERAL The management of Northern Westchester Hospital (NWH) is the responsibility of the Governing Board. -
Sedation Safety at CCH Sector Hospitals
Sedation Safety At CCH Sector Hospitals Learning package for Registered Nurses CSK17376 Developed By: Reviewed By: Jackie Colgan, Cardiac Clinical Julie Howse Nurse Consultant Nurse Educator Central Coast Health Division of Centre for Training and Medicine Development Northern Sydney Central Coast Northern Sydney Central Coast Health Health Created 2009, revised 2012 1 CONTENTS PAGE Prerequisites for successfully undertaking the sedation safety module 3 Aims & expected learning outcomes 4 Introduction/background 5 Sedation safety as a contemporary health care issue 6 Scope of practice 7 Examples of sedation procedures at central coast sector hospitals 8 What is conscious /procedural sedation? 9 Environment for sedation 9 Staffing for sedation 10 Pre-Sedation: patient assessment 11 Physical assessment: whose role is it anyway? 12 Focussed patient assessment: airway 14 Medications used in sedation procedures: 18 Clinical monitoring 21 Assessment of conscious level 22 Documentation standards 24 Recovery from sedation 26 Discharge instructions 26 Escalation/deteriorating patient 28 Clinical Handover 29 Troubleshooting 30 Conclusion 31 Practical assessment advanced airway management 32 References 33-34 Acknowledgements 35 Created 2009, revised 2012 2 PREREQUISITES FOR SUCCESSFULLY UNDERTAKING THE SEDATION SAFETY MODULE 1. All participants must be registered nurses with at least 6 months post qualification experience. 2. Each participant must work in an area where there is a clinical need for this skill. 3. Participants must be accredited to administer intravenous medications. 4. Participants must be currently accredited in basic or, where applicable, advanced life support. The module is a mixture of reading material and self-directed learning activities. The activities relate theoretical concepts to real life situations that you may encounter in your clinical practice. -

Download COVID-19 Interventional Platform: Testing Criteria for Surgeries and Procedures
COVID-19 Interventional Platform Testing Criteria for Surgeries and Procedures Purpose: To provide lab requirements and patient criteria for high and low risk infectivity procedural and surgical cases Applicable Locations: 500P, 300P, Lane Surgery Center, Cath Lab, Endoscopy, Pavilion D, CCSB, Emeryville, OSC Surgeries/Procedures with Anesthesiology Procedures with RN Sedation Lab Requirements Results required prior to determining to proceed* Results required prior to determining to proceed Sedation Type General Anesthesia/MAC RN Sedation • Endoscopy/Colonoscopy Cardiology • Bronchoscopy (Flexible or Rigid) • TEE (with A-Fib, VT ablations) • OHNS • Esophageal temperature probe during A-Fib ablations • Airway Surgery • Over night stay including procedures: Pacemakers, ICD, AF ablations, SVT ablations • CT Surgery • Exercise Stress Test • Thoracic Surgery • Right Heart Catheterization • TEE • Coronary Angiogram • Endomyocardial Biopsy • Left Heart Catheterization Patient and Procedure Powered Instrumentation of the Airway (COVID Test 1 midnight PRIOR to procedure): • Pericardiocentesis Criteria • Endonasal procedures • PCI (including CTO) • Transsphenoidal procedures • ASD/PFO Closure • FESS due to fungal sinusitis • Maxillary Artery Ligation (Embolization) Interventional Radiology • All Otology Surgeries • Lung Biopsy TBA/23 Hour Observation • Lung Cryoablations • New G or GJ Tubes Placement • All patients scheduled to stay at least one midnight • Overnight stay including procedures: UFE ALL Inpatients will be COVID tested before • Chest -

Non-Operating Room Anesthesia: Patient Safety, Scheduling, Efficiency and Effective Leadership
Non-Operating Room Anesthesia: Patient Safety, Scheduling, Efficiency and Effective Leadership Basem Abdelmalak, M.D.,FASA Professor of Anesthesiology, Departments of General Anesthesiology and Outcomes Research, Cleveland Clinic, Cleveland, Ohio Christopher M. Burkle, M.D., J.D. Professor of Anesthesiology Department of Anesthesiology and Perioperative Medicine, Mayo Clinic, Rochester, Minnesota Alan P. Marco, M.D., Professor of Anesthesiology, Department of Anesthesiology, Ohio State University, Columbus, Ohio Donald M. Mathews, M.D., Professor of Anesthesiology and Chair, Department of Anesthesiology, University of Vermont, Burlington, Vermont Financial disclosures: Donald M. Mathews - Masimo, Inc: Advisory Board and Consultancy. No financial disclosures for remaining authors. Conflicts of interest: None “The views, information, or opinions expressed in this manuscript are solely those of the authors and do not necessarily represent those of SAMBA. The authors, editors, and SAMBA, can make no warranties that the information contained herein is totally free from error, not least because clinical standards are constantly changing through research and regulations. The authors, editors, and SAMBA therefore disclaim all liability for direct or consequential damages resulting from the use of material contained in this website” 1 Abdelmalak et al. NORA Safety, Scheduling, Efficiency and Leadership ABSTRACT: Non-Operating Room Anesthesia (NORA) is a services for the growing volume and complexity practice becoming increasingly established of -

Peri-Procedure Management of Antiplatelet Therapy
Peri-Procedure Management of Antiplatelet Therapy Page 1 of 17 Disclaimer: This algorithm has been developed for MD Anderson using a multidisciplinary approach considering circumstances particular to MD Anderson’s specific patient population, services and structure, and clinical information. This is not intended to replace the independent medical or professional judgment of physicians or other health care providers in the context of individual clinical circumstances to determine a patient's care. This algorithm should not be used to treat pregnant women. TABLE OF CONTENTS Interventional Spine/Pain Procedures and Regional Anesthesia Procedures…………………..……..…….…..…………. Page 2 All Other Procedures.……………………………………………………………..……..…….…..……………………………Page 3 APPENDIX A: Procedure Bleeding Risk…………………………….………………………………………………………..Pages 4-9 APPENDIX B: Procedure Bleeding Risk and Management of Antiplatelet Therapy for Interventional Spine and Pain Procedures.…….…………………………………….…….…..………………………………………………Pages 10-11 APPENDIX C: Management of Antiplatelet Therapy for Regional Anesthesia (neuraxial and deep peripheral nerve procedures, including lumbar puncture)..……………………………………………….……….…............ Page 12 APPENDIX D: Management of Antiplatelet Therapy for Other Procedures…………………………………………........Page 13 APPENDIX E: Recommendations for Delaying Elective Procedures……………………………………………………….Page 14 Suggested Readings..……………………………………………………………………………………………………………Pages 15-16 Development Credits...………………………………………………………………………………………………………….Page 17 Department of Clinical Effectiveness -

Monitored Anesthesia Care (MAC) During Gastrointestinal Endoscopy, Bronchoscopy, Or Interventional Pain Procedures in Outpatient Settings Corporate Medical Policy
Monitored Anesthesia Care (MAC) during Gastrointestinal Endoscopy, Bronchoscopy, or Interventional Pain Procedures in Outpatient Settings Corporate Medical Policy File Name: Monitored Anesthesia Care (MAC) during Gastrointestinal Endoscopy Bronchoscopy, or Interventional Pain Procedures in Outpatient Settings File Code: UM.ANES.01 Origination: 07/2009 Last Review: 05/2019 Next Review: 05/2020 Effective Date: 10/01/2019 Description/Summary Monitored anesthesia care (MAC) refers to a set of physician services, not a particular level of sedation. The services include the ability to convert a patient to general anesthesia if needed and to intervene in the event that a patient’s airway becomes compromised. Adequate sedation and analgesia are important parts of diagnostic and therapeutic endoscopic procedures. Various levels of sedation and analgesia (anesthesia) may be used, depending on the patient’s status and the procedure being performed. This policy addresses the clinical indications and risk factors that might necessitate the presence of dedicated anesthesia providers during procedures performed in a properly equipped and staffed outpatient setting. Policy Coding Information Click the links below for attachments, coding tables & instructions. Attachment I- CPT® Coding Table & Instructions When a service may be considered medically necessary Use of monitored anesthesia care may be considered medically necessary for gastrointestinal endoscopy, bronchoscopy, and interventional pain procedures, when there is documentation by the proceduralist -
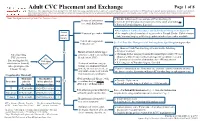
CVC Placement and Exchange
Adult CVC Placement and Exchange Page 1 of 8 Disclaimer: This algorithm has been developed for MD Anderson using a multidisciplinary approach considering circumstances particular to MD Anderson’s specific patient population, services and structure, and clinical information. This is not intended to replace the independent medical or professional judgment of physicians or other health care providers in the context of individual clinical circumstances to determine a patient's care. Note: This algorithm is used by Acute Care Procedures Team ● Discuss with primary team and on-call Vascular Surgery History of arrhythmias ● Consider deferring procedure especially if new-onset or unstable or (i.e., atrial fibrillation) ● Refer to Vascular Surgery, if needed ● See Implanted Cardiac Pacemaker and Defibrillator Management algorithm Assess History of pacemaker ● Line must be placed contralateral to pacemaker. Consult Cardiac Catheterization patient Lab, Vascular Surgery or IR if only ipsilateral side of pacemaker available. history Current anticoagulation See Peri-Procedure Management of Anticoagulants algorithm prior to procedure medication use Page thoracic fellow/Vascular Surgery to discuss the following: ● Safety of treatment No History of blood clots to upper Patient pending extremity central veins (axillary, ● Obtaining further imaging [venous ultrasound duplex study, CT chest CVC placement IJ, subclavian, SVC) obtained within 30 days (contact radiology for vasculature review)] Are ● If contralateral site is free of thrombus, then APP may attempt [internal jugular (IJ), vital signs subclavian or femoral]. unstable1? History of radiation, surgery, ● Referring case to Vascular Surgery, if needed All requests placed to trauma or lesion/mass/wound Infusion Therapy. to neck, chest or access site, or Consider contralateral site. -

Procedures in FM
7/24/2017 Procedures in Family Medicine Scott Stringfield, MD Via Christi Family Medicine Residency Audience Engagement System Poll Question #1 Step 1 Step 2 Step 3 What is your stage of career right now in your educational trajectory? A. MS1 B. MS2 C. MS3 D. MS4 E. R1 F. R2 G. R3 H. Faculty I. other Cnf1 Poll Question #2 What is your current geographic location? Poll: What is your stage of career right now in your educational A. North Central trajectory? B. Midwest C. South Central D. East E. Southeast F. South Central G. Southwest H. West I. Northwest J. Outside of United States 1 Slide 5 Cnf1 Poll: What is your stage of career right now in your educational trajectory? Cnf, 7/19/2016 7/24/2017 Cnf2 Poll Question #3 Poll: What is your current geographic location? What is your planned/desired trajectory for eventual practice? A. Traditional suburban B. Hospitalist C. Rural D. Urban-underserved E. Academic or F. International Cnf3 Poll Question #4 Poll: What is your planned/desired trajectory for eventual practice? Do you think the procedural needs of rural and underserved patients are being met by medicine? A. Yes B. No Cnf4 Overview • Mindset of a proceduralist Poll: Do you think the procedural needs of rural and underserved • “Advanced Family Medicine” patients are being met by medicine? • Why learn procedures? • Advantages and disadvantages • Possible procedural skills • Which procedures? • Financial issues • Where to begin? • Getting the training 2 Slide 7 Cnf2 Poll: What is your current geographic location? Cnf, 7/19/2016 Slide 9 Cnf3 Poll: What is your planned/desired trajectory for eventual practice? Cnf, 7/19/2016 Slide 11 Cnf4 Poll: Do you think the procedural needs of rural and underserved patients are being met by medicine? Cnf, 7/19/2016 7/24/2017 Mindset of a Proceduralist Poll Question #5 • Why choose Family Medicine? • Primary Care vs.