MYOMECTOMY Are Copyright 2010 the British Fibroid Trust
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

720Bfaa8bc7b73a78aff36ddef00
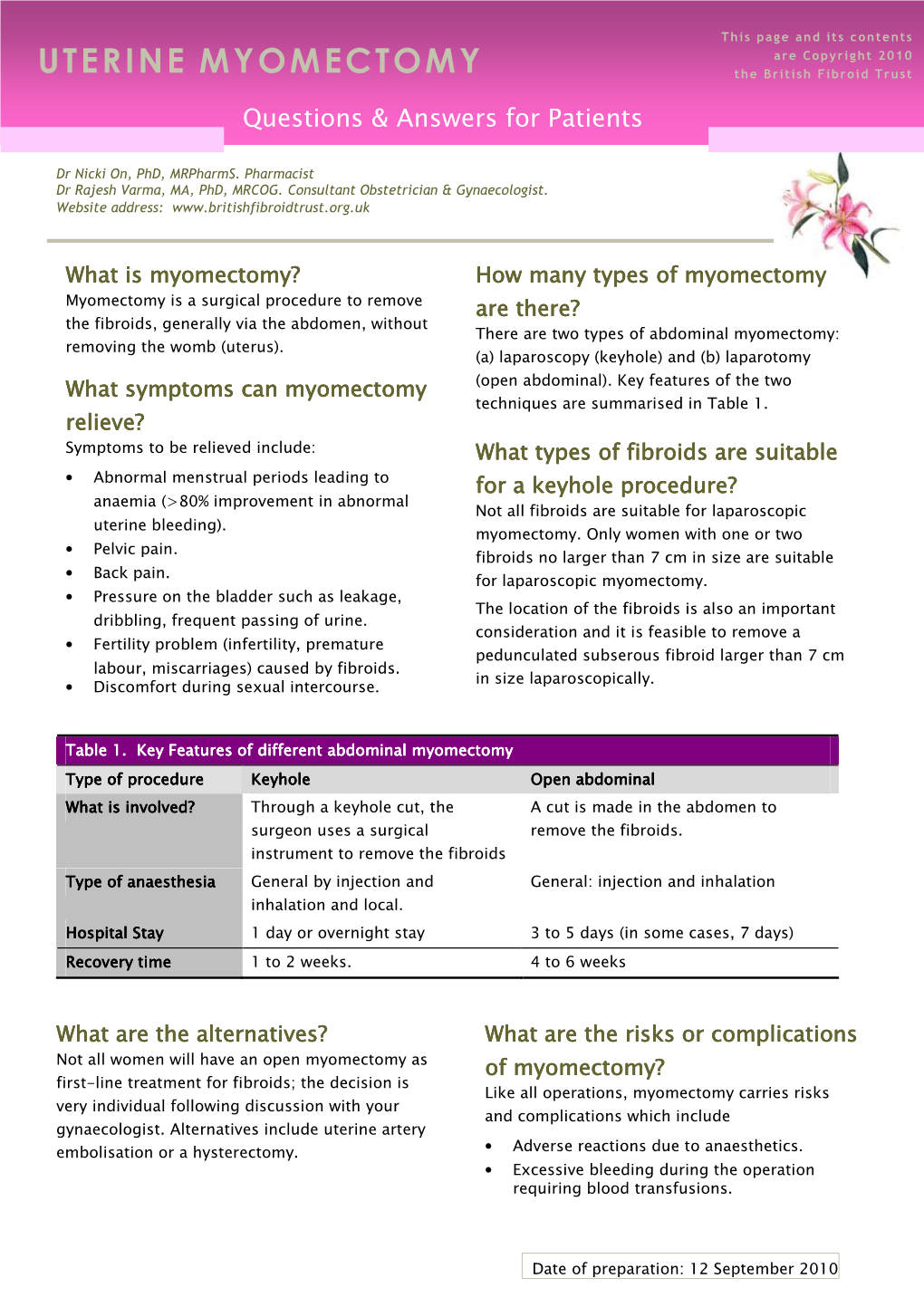
MOLECULAR AND CLINICAL ONCOLOGY 12: 237-243, 2020 A comparative study on the short‑term clinical efficacy of the modified laparoscopic uterine comminution technique and traditional methods XIAOJUN SHI1, LIBING SHI2 and SONGYING ZHANG2 1Department of Gynecology, The First Affiliated Hospital of Jiaxing University, Jiaxing, Zhejiang 314001; 2Assisted Reproduction Unit, Department of Obstetrics and Gynecology, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, Hangzhou, Zhejiang 310016, P.R. China Received April 28, 2019; Accepted December 13, 2019 DOI: 10.3892/mco.2020.1982 Abstract. To assess the value of the modified laparoscopic diagnosis and treatment. It has thus become one of the most uterine comminution technique in laparoscopic uterine surgery, commonly used techniques in the field of gynecology. Uterine a total of 82 cases of laparoscopic myomectomy were divided fibroids are common benign tumors of the female genital into the traditional group and modified group, according to organs and the prevalence has been reported as high as 20 to a random number table. During the same period, 92 patients 40% (1,2). The widespread application of pulverizers allows who underwent laparoscopic hysterectomy were divided into for removal of uterine fibroids under laparoscopy, which better the conventional group and the modified group, according to a reflects the superiority of minimally invasive techniques. random number table. The patients in the conventional group However, preoperative diagnosis of uterine fibroids and and modified group who underwent laparoscopic uterine uterine sarcoma is very difficult. The incidence of uterine fibroid removal showed no significant differences in the fibroid sarcoma is approximately 0.03 to 1.00% (3). -

Minimally Invasive Surgery for Uterine Fibroids
Ginekologia Polska 2020, vol. 91, no. 3, 149–157 Copyright © 2020 Via Medica REVIEW PAPER / GYNECOLOGY ISSN 0017–0011 DOI: 10.5603/GP.2020.0032 Minimally invasive surgery for uterine fibroids Yuehan Wang1 , Shitai Zhang1 , Chenyang Li2 , Bo Li1 , Ling Ouyang1 1Department of Obstetrics and Gynecology, Shengjing Hospital of China Medical University, Shenyang, China 2Shenyang Maternity and Child Health Hospital, Shenyang, China ABSTRACT The incidence of uterine fibroids, which comprise one of the most common female pelvic tumors, is almost 70–75% for women of reproductive age. With the development of surgical techniques and skills, more individuals prefer minimally invasive methods to treat uterine fibroids. There is no doubt that minimally invasive surgery has broad use for uterine fibroids. Since laparoscopic myomectomy was first performed in 1979, more methods have been used for uterine fibroids, such as laparoscopic hysterectomy, laparoscopic radiofrequency volumetric thermal ablation, and uterine artery emboliza- tion, and each has many variations. In this review, we compared these methods of minimally invasive surgery for uterine fibroids, analyzed their benefits and drawbacks, and discussed their future development. Key words: minimally invasive surgery; uterine fibroid; laparoscopic hysterectomy; laparoscopic myomectomy Ginekologia Polska 2020; 91, 3: 149–157 INTRODUCTION fibroids. They found that those two kinds of surgery did Uterine fibroids comprise one of the most common not have different recurrence risks, but that laparoscopic female pelvic tumors. When including the small, clinically myomectomy may be associated with less postoperative undetectable fibroids and microscopic fibroids, the incidence pain, lower postoperative fever, and shorter hospital stays is approximately 70–75% for those of reproductive age. -

Obstetrics and Gynecology Clinical Privilege List
Obstetrics and Gynecology Clinical Privilege List Description of Service Alberta Health Services (AHS) Medical Staff who are specialists in Obstetrics and Gynecology (or its associated subspecialties) and have privileges in the Department of Obstetrics and Gynecology provide safe, high quality care for obstetrical and gynecologic patients in AHS facilities across the province. The specialty encompasses medical, surgical, obstetrical and gynecologic knowledge and skills for the prevention, diagnosis and management of a broad range of conditions affecting women's gynecological and reproductive health. Working to provide a patient-focused, quality health system that is accessible and sustainable for all Albertans, the department also offers subspecialty care including gynecological oncology, reproductive endocrinology, maternal fetal medicine, urogynecology, and minimally invasive surgery.1 Obstetrics and Gynecology privileges may include admitting, evaluating, diagnosing, treating (medical and/or surgical management), to female patients of all ages presenting in any condition or stage of pregnancy or female patients presenting with illnesses, injuries, and disorders of the gynecological or genitourinary system including the ability to assess, stabilize, and determine the disposition of patients with emergent conditions consistent with medical staff policy regarding emergency and consultative call services. Providing consultation based on the designated position profile (clinical; education; research; service), and/or limited Medical Staff -

Gynaecology – Scope of Clinical Practice
Epworth HealthCare Gynaecology – Scope of Clinical Practice Gynaecology – Scope of Clinical Practice Clinical Institute: Women’s and Children’s Procedure Name Tier Adnexal surgery, including ovarian cystectomy, oophorectomy, salpingectomy, and Tier A conservative procedures for treatment of ectopic pregnancy Aspiration of breast masses Tier A Bladder biopsy and diathermy Tier A Cervical biopsy Tier A Colpocleisis Tier A Colpoplasty Tier A Colposcopy Tier A Consulting Tier A Cystoscopic injection of Botulinum Toxin Tier A Cystoscopy as part of gynaecological procedure Tier A D&C for abortion Tier A Delayed anal sphincter repair Tier A Diagnostic laparoscopy Tier A Endometrial ablation Tier A Exploratory laparotomy, for diagnosis and treatment of pelvic pain, pelvic mass, Tier A hemoperitoneum, endometriosis and adhesions Gynaecological sonography Tier A Hysterectomy, abdominal, vaginal, excluding laparoscopic Tier A Hysterosalpingography Tier A Hysteroscopic surgery Tier A Hysteroscopy Tier A I&D of bartholin cyst or perineal abscess Tier A I&D of pelvic abscess Tier A Incidental appendectomy Tier A Insertion and removal of IUCD Tier A Intrauterine myomectomy with power morcellation by hysteroscopic approach Tier A Laparoscopic surgery (excludes laparoscopic myomectomy with power morcellation) Tier A Laparotomy Tier A Marsupialisation of bartholin cysts Tier A Minor gynaecological surgical procedures (endometrial biopsy, dilation and curettage, Tier A treatment of Bartholin cyst and abscess) Myomectomy Tier A Operation for treatment of -

Case Report Uterine Fibroid Torsion During Pregnancy: a Case of Laparotomic Myomectomy at 18 Weeks’ Gestation with Systematic Review of the Literature
Hindawi Case Reports in Obstetrics and Gynecology Volume 2017, Article ID 4970802, 11 pages https://doi.org/10.1155/2017/4970802 Case Report Uterine Fibroid Torsion during Pregnancy: A Case of Laparotomic Myomectomy at 18 Weeks’ Gestation with Systematic Review of the Literature Annachiara Basso,1 Mariana Rita Catalano,1 Giuseppe Loverro,1 Serena Nocera,1 Edoardo Di Naro,1 Matteo Loverro,1 Mariateresa Natrella,2 and Salvatore Andrea Mastrolia1 1 Department of Obstetrics and Gynecology, Azienda Ospedaliera Universitaria Policlinico di Bari, School of Medicine, UniversitadegliStudidiBari“AldoMoro”,Bari,Italy` 2School of Nursing, Azienda Ospedaliera Universitaria Policlinico di Bari, School of Medicine, UniversitadegliStudidiBari“AldoMoro”,Bari,Italy` Correspondence should be addressed to Salvatore Andrea Mastrolia; [email protected] Received 15 January 2017; Revised 17 March 2017; Accepted 20 March 2017; Published 24 April 2017 Academic Editor: Maria Grazia Porpora Copyright © 2017 Annachiara Basso et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Uterine myomas are the most common benign growths affecting female reproductive system, occurring in 20–40% of women, whereas the incidence rate in pregnancy is estimated from 0.1 to 3.9%. The lower incidence in pregnancy is due to the association with infertility and low pregnancy rates and implantation rates after in vitro fertilization treatment. Uterine myomas, usually, are asymptomatic during pregnancy. However, occasionally, pedunculated fibroids torsion or other superimposed complications may cause acute abdominal pain. There are many controversies in performing myomectomy during cesarean section because of the risk of hemorrhage. -

SJH Procedures
SJH Procedures - Gynecology and Gynecology Oncology Services New Name Old Name CPT Code Service ABLATION, LESION, CERVIX AND VULVA, USING CO2 LASER LASER VAPORIZATION CERVIX/VULVA W CO2 LASER 56501 Destruction of lesion(s), vulva; simple (eg, laser surgery, Gynecology electrosurgery, cryosurgery, chemosurgery) 56515 Destruction of lesion(s), vulva; extensive (eg, laser surgery, Gynecology electrosurgery, cryosurgery, chemosurgery) 57513 Cautery of cervix; laser ablation Gynecology BIOPSY OR EXCISION, LESION, FACE AND NECK EXCISION/BIOPSY (MASS/LESION/LIPOMA/CYST) FACE/NECK General, Gynecology, Plastics, ENT, Maxillofacial BIOPSY OR EXCISION, LESION, FACE AND NECK, 2 OR MORE EXCISE/BIOPSY (MASS/LESION/LIPOMA/CYST) MULTIPLE FACE/NECK 11102 Tangential biopsy of skin (eg, shave, scoop, saucerize, curette); General, Gynecology, single lesion Aesthetics, Urology, Maxillofacial, ENT, Thoracic, Vascular, Cardiovascular, Plastics, Orthopedics 11103 Tangential biopsy of skin (eg, shave, scoop, saucerize, curette); General, Gynecology, each separate/additional lesion (list separately in addition to Aesthetics, Urology, code for primary procedure) Maxillofacial, ENT, Thoracic, Vascular, Cardiovascular, Plastics, Orthopedics 11104 Punch biopsy of skin (including simple closure, when General, Gynecology, performed); single lesion Aesthetics, Urology, Maxillofacial, ENT, Thoracic, Vascular, Cardiovascular, Plastics, Orthopedics 11105 Punch biopsy of skin (including simple closure, when General, Gynecology, performed); each separate/additional lesion -

Uterine Fibroids and Sepsis
DISCLAIMER: Results of database and or Internet searches are subject to the limitations of both the database(s) searched, and by your search request. It is the responsibility of the requestor to determine the accuracy, validity and interpretation of the results. Date: 13 November 2018 Sources Searched: Embase, Medline. Uterine Fibroids and Sepsis See full search strategy 1. Spontaneous Ruptured Pyomyoma in a Nulligravid Female: A Case Report and Review of the Literature. Author(s): Read, S; Mullins, J Source: Case reports in obstetrics and gynecology; 2018; vol. 2018 ; p. 1026287 Publication Date: 2018 Publication Type(s): Journal Article PubMedID: 30057837 Available at Case reports in obstetrics and gynecology - from Europe PubMed Central - Open Access Abstract:IntroductionPyomyoma, or suppurative leiomyoma, is a rare complication of uterine fibroids. It occurs most commonly in the setting of pregnancy, the immediate postpartum period, or postmenopausal status. It may also arise after recent uterine instrumentation, after uterine artery embolization, or in immunocompromised patients. The most likely cause of pyomyoma is vascular compromise followed by bacterial seeding from direct, hematogenous, or lymphatic spread. Diagnosis is difficult, as the condition is rare, presents with vague symptoms, and is difficult to identify on imaging. Definitive diagnosis is only possible with surgery. Pathology shows a degenerating fibroid with hemorrhage, necrosis, cystic degeneration, and/or inflammatory change. Cultures of the pus contained within often show polymicrobial infection.Case PresentationOur patient is a 24-year-old nulligravid female who presented with a surgical abdomen, fever, hypotension, and leukocytosis. She had no significant prior medical or surgical history, no history of uterine instrumentation, and no history of pelvic infection; she was not currently sexually active at the time of presentation. -

Wehealth Plus Benefit Schedule
WeHealth Plus Benefit Schedule [Applicable to Scheme 1] Benefit items(1) Benefit limit (in HKD) (a) Room and board $1,000 per day Maximum 180 days per Policy Year (b) Miscellaneous charges $14,000 per Policy Year (c) Attending doctor's visit fee $750 per day Maximum 180 days per Policy Year (d) Specialist's fee(2) $4,300 per Policy Year (e) Intensive care $3,500 per day Maximum 25 days per Policy Year (f) Surgeon's fee Per surgery, subject to surgical category for the surgery/procedure in the Schedule of Surgical Procedures – • Complex $50,000 • Major $25,000 • Intermediate $12,500 • Minor $5,000 (g) Anaesthetist's fee 35% of Surgeon's fee payable (5) (h) Operating theatre charges 35% of Surgeon's fee payable (5) (i) Prescribed Diagnostic Imaging Tests(2) (3) $20,000 per Policy Year Subject to 30% Coinsurance (j) Prescribed Non-surgical Cancer $80,000 per Policy Year Treatments(4) (k) Pre- and post-Confinement/Day Case $580 per visit, up to $3,000 per Policy Year Procedure outpatient care (2) • 1 prior outpatient visit or Emergency consultation per Confinement/Day Case Procedure • 3 follow-up outpatient visits per Confinement/Day Case Procedure (within 90 days after discharge from Hospital or completion of Day Case Procedure) (l) Psychiatric treatments $30,000 per Policy Year Enhanced benefits (1) Home nursing benefit(2) $600 per day Below Age 60: Maximum 15 days per Policy Year Age 60 and/or above: Maximum 30 days per Policy Year (within 90 days after discharge from Hospital or completion of Day Case Procedure) (2) Kidney dialysis treatment benefit(2) $60,000 per Policy Year (Effective after 90 days from Policy Issuance Date / Policy Effective Date, whichever is earlier) (3) Emergency outpatient treatment benefit $5,000 per Policy Year (4) Cardiac rehabilitation treatment $10,000 per Policy Year benefit (2) (within 90 days after discharge from Hospital or completion of Day Case Procedure) The content on this page is part of the Terms and Benefits of Certified Plan (No. -

Final Program
SCIENTIFIC PROGRAM CHAIR Arnold P. Advincula, M.D. 43rd AAGL PRESIDENT Ceana H. Nezhat, M.D. GLOBAL CONGRESS HONORARY CHAIR ON MINIMALLY INVASIVE GYNECOLOGY Farr R. Nezhat, M.D. NOV. 17-21, 2014 | Vancouver, British Columbia HONORARY MEMBER Victor Gomel, M.D. FINAL PROGRAM Experience Excellence in Education The AAGL Global Congress is the pre-eminent meeting for physicians interested in providing optimal patient care through minimally invasive gynecology. Designed to meet the needs of practicing surgeons, residents and fellows, operating room personnel and other allied healthcare professionals, the Congress covers traditional topics as well as presentations of “cutting edge” material. With opportunities to discuss and share discoveries, you will experience excellence in formal, informal and collegial education. Take control of port site closure with the Weck EFx® Closure System SUPPORT WOMEN’S HEALTH AT AAGL 2014 Visit Teleflex booth 431 and support women’s health with the Weck EFx Quick Closure Challenge. Teleflex will donate $10,000 to help support the advancement of gynecological laparoscopy to the organization with the highest number of votes submitted by successful Challenge participants.* Confidence. Clarity. Control. Universal design accommodates Consistent and uniform 1 cm A TRUE unassisted approach both standard and bariatric fascial purchase 180 degrees to port site closure. anatomy for 10–15 mm defects. across the defect. *For complete rules and eligibility, visit us at www.weckefx.com/QuickClosureChallenge Teleflex, Weck EFx -

Leiomyomatoid Angiomatous Neuroendocrine Tumor of the Myometrium
Asian Biomedicine Vol. 7 No. 3 June 2013; 443-448 DOI: 10.5372/1905-7415.0703.198 Clinical report Leiomyomatoid angiomatous neuroendocrine tumor of the myometrium Jing Luoa, Can Sunb, Wei Sunc aDepartment of Pathology, Fuxing Hospital, Capital Medical University, Beijing 100038, bPeking University Health Science Center, Beijing 100191, cDepartment of Neurosurgery, Beijing Charity Hospital, China Rehabilitation Research Centre, Capital Medical University School of Rehabilitation Medicine, Beijing 100068, China Background: Only a few cases of Leiomyomatoid angiomatous neuroendocrine tumor (LANT) have been reported in the literature. Our case adds clinical, pathological, and immunohistochemical features. Objective: To investigate the clinicopathological characteristics of LANT. Material and Method: One case of LANT of the myometrium was reported in a review of literature. The morphological and immunohistochemical features were analyzed. Results: In the course of an annual health examination of a 40-year-old woman, ultrasound results revealed a mass in the myometrium, which was clinically diagnosed as uterine leiomyoma. The patient underwent hysterectomy. Histological examination demonstrated that the tumor was composed of prominent vasculature and cellular stromal around vessels. Mitotic activity was absent. Both vascular and stromal cells showed diffusely expressed CD56 and chromogranin A. Stromal cells also expressed actin, SMA, and desmin, but not CK or HMB45. The pathological diagnosis was LANT of the myometrium. Follow up reported no evidence of recurrence three months after surgery. Conclusion: LANT is a possible new disease entity. LANT is a dimorphic tumor consisting of smooth muscle and neurosecretory phenotype cells surrounding intratumoral vessels. Surgery may be the best treatment, resulting in good prognosis. Keywords: Immunohistochemistry, neuroendocrine neoplasm, pathology, uterus In a recent inspection, a case of uterine muscle leiomyoma, and uterine myomectomy was performed. -

Role of Robot-Assisted Pelvic Surgery
Review Special Issue: Update on Lower Urinary Tract Symptoms TheScientificWorldJOURNAL (2009) 9, 479–489 TSW Urology ISSN 1537-744X; DOI 10.1100/tsw.2009.54 Role of Robot-Assisted Pelvic Surgery Iqbal Singh and Ashok K. Hemal* Department of Urology, Wake Forest University School of Medicine and Wake Forest University Baptist Medical Center, Medical Center Boulevard, Winston- Salem, NC E-mail : [email protected] Received July 23, 2008; Revised January 30, 2009; Accepted May 17, 2009; Published June 12, 2009 The purpose of this study was to assess the current role of robot-assisted urological surgery in the female pelvis. The recently published English literature was reviewed to evaluate this role, with special emphasis on reconstructive procedures. These included colposuspension for genuine female stress urinary incontinence, repair of female genitourinary fistulas, ureterosciatic hernias, sacrocolpopexy for vault prolapse, ureterolysis and omental wrap for retroperitoneal fibrosis, ureteric reimplantation, and bladder surgery. To date, a wide spectrum of urogynecological reconstructive procedures have been performed with the assistance of the surgical robot and have been reported worldwide. Currently, a number of female pelvic ablative and reconstructive procedures are technically feasible with the aid of the surgical robot. While the role of robot-assisted surgery for bladder cancer, ureterolysis, ureteric reimplantation, repair of genitourinary fistulas, colposuspension, and sacrocolpopexy is nearly established among urologists, other procedures, such as myomectomy, simple hysterectomy, trachelectomy, and Wertheim's hysterectomy, are still evolving with gynecologists. The advantages of robot assistance include better hand-eye coordination, three-dimensional magnified stereoscopic vision with depth perception, intuitive movements with increased precision, and filtering of hand tremors. -

Lehigh Valley Health Network R G C N Population
LEHIGH VALLEY HEALTH NETWORK CLINICAL PRIVILEGES IN OBSTETRICS AND GYNECOLOGY Initial Renewed Name______________________________________ Effective from ___/___/___ to ___/___/___ R = Requested G = Recommended As Requested C = Recommended with Conditions N = Not Recommended R G C N POPULATION Pediatric: Birth - 25 Years (Fairgrounds Surgical Center, LVHN Surgery Center-Tilghman - 6 months - 1 Year and LVHN Children's Surgery Center - 6 months - 1 Year) Adults: 13 - 65 Years Geriatrics: Over 65 Years R G C N GENERAL PRIVILEGES Admitting (includes inpatient, outpatient procedures, and observation) (1,2,3,4,5,6,7,8,9,10,11,12) History and Physical (1,2,3,4,5,6,7,8,9,10,11,12) Prescribing Privileges (1,2,3,4,5,6,7,8,9,10,11,12) Certifying of Medical Marijuana* (1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12) (*Must satisfy certain credentialing criteria to be approved) R G C N OBSTETRICS Amnio infusion (1,2,7,10) Amniocentesis, 2nd and 3rd Trimester (1,2,7,10) Amniotomy (1,2,7,10) Anesthesia - local block (1,2,3,4,7,9,10) Anesthesia - paracervical block (1,2,3,4,7,8,9,10) Anesthesia - pudenal block (1,2,7,10) Artery ligation: uterine, hypogastric (1,2,7,10) B Lynch Procedure (1,2,7,10) Cervical biopsy during pregnancy (1,2,3,7,8,10) Cervical cerclage (1,2,7,8,10) 9/9/2020 Page 1 of 17 LEHIGH VALLEY HEALTH NETWORK CLINICAL PRIVILEGES IN OBSTETRICS AND GYNECOLOGY Initial Renewed Name______________________________________ Effective from ___/___/___ to ___/___/___ R = Requested G = Recommended As Requested C = Recommended with Conditions N = Not Recommended