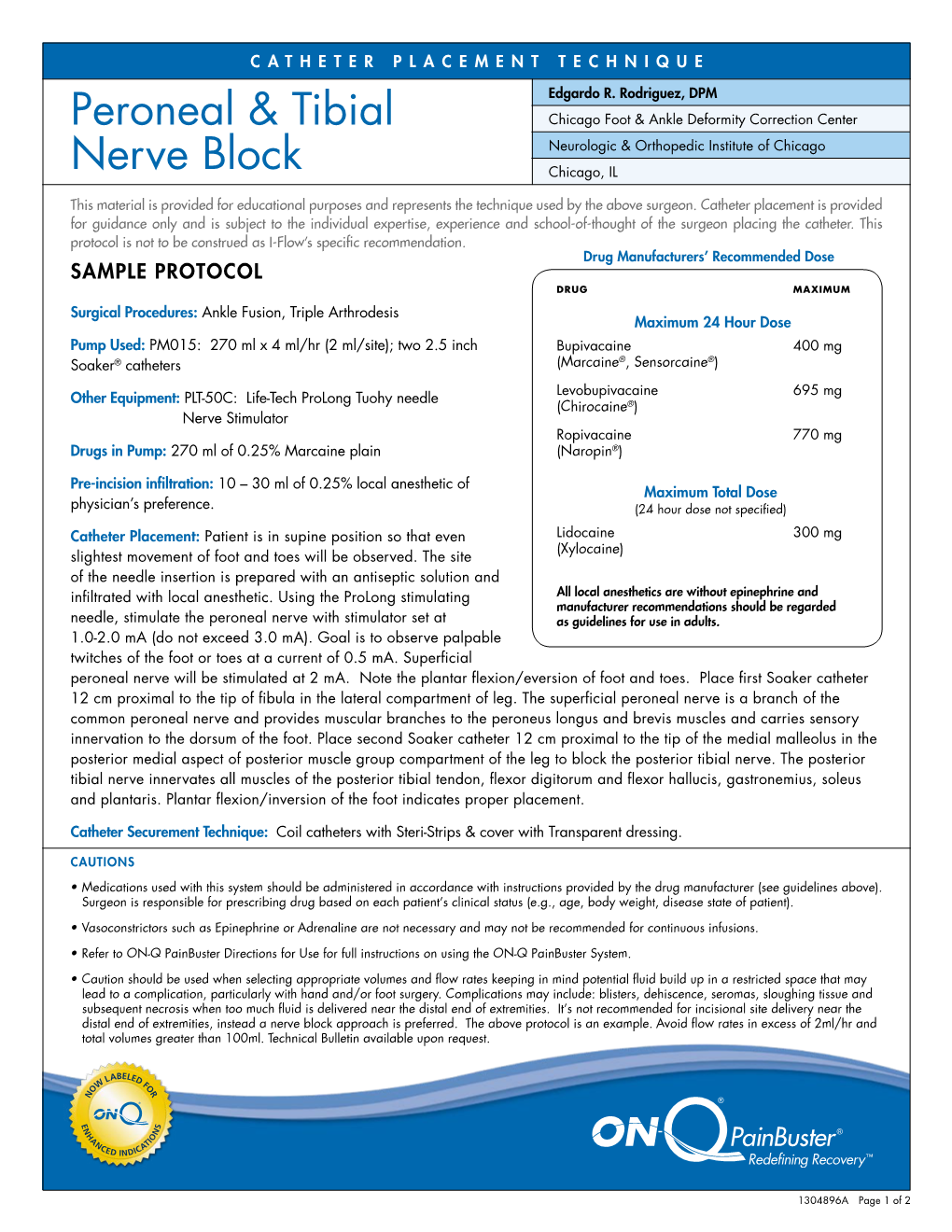
Peroneal & Tibial Nerve Block
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clinical Presentations of Lumbar Disc Degeneration and Lumbosacral Nerve Lesions
Hindawi International Journal of Rheumatology Volume 2020, Article ID 2919625, 13 pages https://doi.org/10.1155/2020/2919625 Review Article Clinical Presentations of Lumbar Disc Degeneration and Lumbosacral Nerve Lesions Worku Abie Liyew Biomedical Science Department, School of Medicine, Debre Markos University, Debre Markos, Ethiopia Correspondence should be addressed to Worku Abie Liyew; [email protected] Received 25 April 2020; Revised 26 June 2020; Accepted 13 July 2020; Published 29 August 2020 Academic Editor: Bruce M. Rothschild Copyright © 2020 Worku Abie Liyew. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Lumbar disc degeneration is defined as the wear and tear of lumbar intervertebral disc, and it is mainly occurring at L3-L4 and L4-S1 vertebrae. Lumbar disc degeneration may lead to disc bulging, osteophytes, loss of disc space, and compression and irritation of the adjacent nerve root. Clinical presentations associated with lumbar disc degeneration and lumbosacral nerve lesion are discogenic pain, radical pain, muscular weakness, and cutaneous. Discogenic pain is usually felt in the lumbar region, or sometimes, it may feel in the buttocks, down to the upper thighs, and it is typically presented with sudden forced flexion and/or rotational moment. Radical pain, muscular weakness, and sensory defects associated with lumbosacral nerve lesions are distributed on -
LECTURE (SACRAL PLEXUS, SCIATIC NERVE and FEMORAL NERVE) Done By: Manar Al-Eid Reviewed By: Abdullah Alanazi
CNS-432 LECTURE (SACRAL PLEXUS, SCIATIC NERVE AND FEMORAL NERVE) Done by: Manar Al-Eid Reviewed by: Abdullah Alanazi If there is any mistake please feel free to contact us: [email protected] Both - Black Male Notes - BLUE Female Notes - GREEN Explanation and additional notes - ORANGE Very Important note - Red CNS-432 Objectives: By the end of the lecture, students should be able to: . Describe the formation of sacral plexus (site & root value). List the main branches of sacral plexus. Describe the course of the femoral & the sciatic nerves . List the motor and sensory distribution of femoral & sciatic nerves. Describe the effects of lesion of the femoral & the sciatic nerves (motor & sensory). CNS-432 The Mind Maps Lumber Plexus 1 Branches Iliohypogastric - obturator ilioinguinal Femoral Cutaneous branches Muscular branches to abdomen and lower limb 2 Sacral Plexus Branches Pudendal nerve. Pelvic Splanchnic Sciatic nerve (largest nerves nerve), divides into: Tibial and divides Fibular and divides into : into: Medial and lateral Deep peroneal Superficial planter nerves . peroneal CNS-432 Remember !! gastrocnemius Planter flexion – knee flexion. soleus Planter flexion Iliacus –sartorius- pectineus – Hip flexion psoas major Quadriceps femoris Knee extension Hamstring muscles Knee flexion and hip extension gracilis Hip flexion and aids in knee flexion *popliteal fossa structures (superficial to deep): 1-tibial nerve 2-popliteal vein 3-popliteal artery. *foot drop : planter flexed position Common peroneal nerve injury leads to Equinovarus Tibial nerve injury leads to Calcaneovalgus CNS-432 Lumbar Plexus Formation Ventral (anterior) rami of the upper 4 lumbar spinal nerves (L1,2,3 and L4). Site Within the substance of the psoas major muscle. -

Lower Extremity Focal Neuropathies
LOWER EXTREMITY FOCAL NEUROPATHIES Lower Extremity Focal Neuropathies Arturo A. Leis, MD S.H. Subramony, MD Vettaikorumakankav Vedanarayanan, MD, MBBS Mark A. Ross, MD AANEM 59th Annual Meeting Orlando, Florida Copyright © September 2012 American Association of Neuromuscular & Electrodiagnostic Medicine 2621 Superior Drive NW Rochester, MN 55901 Printed by Johnson Printing Company, Inc. 1 Please be aware that some of the medical devices or pharmaceuticals discussed in this handout may not be cleared by the FDA or cleared by the FDA for the specific use described by the authors and are “off-label” (i.e., a use not described on the product’s label). “Off-label” devices or pharmaceuticals may be used if, in the judgment of the treating physician, such use is medically indicated to treat a patient’s condition. Information regarding the FDA clearance status of a particular device or pharmaceutical may be obtained by reading the product’s package labeling, by contacting a sales representative or legal counsel of the manufacturer of the device or pharmaceutical, or by contacting the FDA at 1-800-638-2041. 2 LOWER EXTREMITY FOCAL NEUROPATHIES Lower Extremity Focal Neuropathies Table of Contents Course Committees & Course Objectives 4 Faculty 5 Basic and Special Nerve Conduction Studies of the Lower Limbs 7 Arturo A. Leis, MD Common Peroneal Neuropathy and Foot Drop 19 S.H. Subramony, MD Mononeuropathies Affecting Tibial Nerve and its Branches 23 Vettaikorumakankav Vedanarayanan, MD, MBBS Femoral, Obturator, and Lateral Femoral Cutaneous Neuropathies 27 Mark A. Ross, MD CME Questions 33 No one involved in the planning of this CME activity had any relevant financial relationships to disclose. -

Human Distal Sciatic Nerve Fascicular Anatomy: Implications for Ankle Control Using Nerve-Cuff Electrodes
Volume 49, Number 2, 2012 JRRDJRRD Pages 309–322 Human distal sciatic nerve fascicular anatomy: Implications for ankle control using nerve-cuff electrodes Kenneth J. Gustafson, PhD;1–2* Yanina Grinberg, MS;1 Sheeba Joseph, BS;3 Ronald J. Triolo, PhD1–2,4 1Department of Biomedical Engineering, Case Western Reserve University, Cleveland, OH; 2Louis Stokes Cleveland Department of Veterans Affairs Medical Center, Cleveland, OH; 3Case Western Reserve University School of Medicine, Cleveland, OH; 4Department of Orthopedics, Case Western Reserve University, Cleveland, OH Abstract—The design of neural prostheses to restore standing eversion of the talocrural (ankle) joint and are therefore balance, prevent foot drop, or provide active propulsion during critical for standing balance and walking functions. The ambulation requires detailed knowledge of the distal sciatic sciatic nerve originates in the lumbar and sacral spinal nerve anatomy. Three complete sciatic nerves and branches cord and supplies motor and sensory innervation to the were dissected from the piriformis to each muscle entry point lower limb. It has two major terminal branches, the tibial to characterize the branching patterns and diameters. Fascicle nerve and common fibular nerve. The common fibular maps were created from serial sections of each distal terminus (common peroneal) branches into the deep and superfi- below the knee through the anastomosis of the tibial and com- cial fibular (SF) nerves and is commonly targeted in neu- mon fibular nerves above the knee. Similar branching patterns ral prostheses used to correct foot drop [1–5]. The deep and fascicle maps were observed across specimens. Fascicles innervating primary plantar flexors, dorsiflexors, invertors, and fibular (DF) branch innervates the tibialis anterior mus- evertors were distinctly separate and functionally organized in cle, which dorsiflexes and inverts the foot. -

Tarsal Tunnel Syndrome Secondary to the Posterior Tibial Nerve Schwannoma
Case Report http://dx.doi.org/10.12972/The Nerve.2015.01.01.034 www.thenerve.net Tarsal Tunnel Syndrome Secondary to the Posterior Tibial Nerve Schwannoma Jung Won Song1, Sung Han Oh1, Pyung Goo Cho1, Eun Mee Han2 Departments of 1Neurosurgey, 2Pathology, Bundang Jesaeng General Hospital, Seongnam, Korea A 77-year-old female presented with complaint of burning pain and paresthesia along the medial aspect of ankle, heel and sole of the left foot. An ankle MRI, electromyelogram (EMG) with nerve conduction velocity (NCV) and pathologic findings were all compatible with Tarsal tunnel syndrome caused by the posterior tibial nerve Schwannoma. Operative release of the Tarsal tunnel and surgical excision of Schwannoma were performed under the microscopy. It is necessary to have a possible lump in mind when Tarsal tunnel syndrome is suspected, such as posterior tibial nerve Schwannoma. Key Words: Posterior Tibial NerveㆍSchwannomaㆍTarsal Tunnel Syndrome diagnose neurofibromatosis was insufficient. An ankle magne- tic resonance imaging (MRI) revealed about a 22×19×9 mm- INTRODUCTION sized ovoid soft tissue mass in the posterior ankle connected to the posterior tibial nerve. The mass lies beneath the flexor Although Schwannomas are the most common peripheral retinaculum of ankle and showed relatively strong enhance- nerve sheath tumor, Schwannoma of the posterior tibial nerve ment (Fig. 1). and it branch is a rare etiology causing Tarsal tunnel syndrome. The NCV study showed no response sensory nerve action We report a case of Tarsal tunnel syndrome caused by the pos- potentials of the left medial and lateral plantar nerves. Motor terior tibial nerve Schwannoma and mention surgical strategy conduction study of the deep peroneal and tibial nerves was with literature review. -

Tibial Nerve Block: Supramalleolar Or Retromalleolar Approach? a Randomized Trial in 110 Participants
International Journal of Environmental Research and Public Health Article Tibial Nerve Block: Supramalleolar or Retromalleolar Approach? A Randomized Trial in 110 Participants María Benimeli-Fenollar 1,* , José M. Montiel-Company 2 , José M. Almerich-Silla 2 , Rosa Cibrián 3 and Cecili Macián-Romero 1 1 Department of Nursing, University of Valencia, c/Jaume Roig s/n, 46010 Valencia, Spain; [email protected] 2 Department of Stomatology, University of Valencia, c/Gascó Oliag, 1, 46010 Valencia, Spain; [email protected] (J.M.M.-C.); [email protected] (J.M.A.-S.) 3 Department of Physiology, University of Valencia, c/Blasco Ibánez, 15, 46010 Valencia, Spain; [email protected] * Correspondence: [email protected] Received: 26 April 2020; Accepted: 23 May 2020; Published: 29 May 2020 Abstract: Of the five nerves that innervate the foot, the one in which anesthetic blocking presents the greatest difficulty is the tibial nerve. The aim of this clinical trial was to establish a protocol for two tibial nerve block anesthetic techniques to later compare the anesthetic efficiency of retromalleolar blocking and supramalleolar blocking in order to ascertain whether the supramalleolar approach achieved a higher effective blocking rate. A total of 110 tibial nerve blocks were performed. Location of the injection site was based on a prior ultrasound assessment of the tibial nerve. The block administered was 3 mL of 2% mepivacaine. The two anesthetic techniques under study provided very similar clinical results. The tibial nerve success rate was 81.8% for the retromalleolar technique and 78.2% for the supramalleolar technique. -

The Muscles That Act on the Lower Limb Fall Into Three Groups: Those That Move the Thigh, Those That Move the Lower Leg, and Those That Move the Ankle, Foot, and Toes
MUSCLES OF THE APPENDICULAR SKELETON LOWER LIMB The muscles that act on the lower limb fall into three groups: those that move the thigh, those that move the lower leg, and those that move the ankle, foot, and toes. Muscles Moving the Thigh (Marieb / Hoehn – Chapter 10; Pgs. 363 – 369; Figures 1 & 2) MUSCLE: ORIGIN: INSERTION: INNERVATION: ACTION: ANTERIOR: Iliacus* iliac fossa / crest lesser trochanter femoral nerve flexes thigh (part of Iliopsoas) of os coxa; ala of sacrum of femur Psoas major* lesser trochanter --------------- T – L vertebrae flexes thigh (part of Iliopsoas) 12 5 of femur (spinal nerves) iliac crest / anterior iliotibial tract Tensor fasciae latae* superior iliac spine gluteal nerves flexes / abducts thigh (connective tissue) of ox coxa anterior superior iliac spine medial surface flexes / adducts / Sartorius* femoral nerve of ox coxa of proximal tibia laterally rotates thigh lesser trochanter adducts / flexes / medially Pectineus* pubis obturator nerve of femur rotates thigh Adductor brevis* linea aspera adducts / flexes / medially pubis obturator nerve (part of Adductors) of femur rotates thigh Adductor longus* linea aspera adducts / flexes / medially pubis obturator nerve (part of Adductors) of femur rotates thigh MUSCLE: ORIGIN: INSERTION: INNERVATION: ACTION: linea aspera obturator nerve / adducts / flexes / medially Adductor magnus* pubis / ischium (part of Adductors) of femur sciatic nerve rotates thigh medial surface adducts / flexes / medially Gracilis* pubis / ischium obturator nerve of proximal tibia rotates -

Sacral Plexus and the Pudendal Nerve in Man by Use of Computer Aided Three-Dimensional Reconstruction
Okajimas Folia Anat. Jpn., 72(1): 29-36, May, 1995 An Anatomical Analysis of the Dorsoventral Relationship between the Sacral Plexus and the Pudendal Nerve in Man by Use of Computer Aided Three-Dimensional Reconstruction By Keiichi AKITA and Hitoshi YAMAMOTO Department of Anatomy, School of Medicine, Tokyo Medical and Dental University, 1-5-45 Yushima, Bunkyo-ku, Tokyo, 113, Japan -Received for Publication, January 30, 1995- Key Words: Pudendal nerve, Sacral Plexus, 3-D reconstruction, Human gross anatomy Summary: In order to investigate the dorsoventral relationship between the sacral plexus and the pudendal nerve in man, morphological examination was performed on one pelvic half of a male cadaver. The second and third spinal nerves were removed en bloc and sectioned serially for three-dimensional reconstruction imaging of the selected sections. Comparison of the sequential images revealed that the root of the pudendal nerve is first situated ventral to the caudal root of the sacral plexus, and that the former and the latter are shifted cranialward and caudalward, respectively, at the point of exit from the second anterior sacral foramen. Abbreviation (Macaw mulatta) in order to determine the detailed relationships between the innervation of the pelvic Bis nerveto the short head of the bicepsfemoris limb and the pelvic outlet muscles. These findings Br (ex. Br1) branchof the spinalnerve revealed that the origins of the pudendal nerves Cfp posteriorfemoral cutaneous nerve were situated ventrocaudal to the sacral plexus. Co nerveto the coccygeus D dorsalprimary rami The present study was undertaken to confirm the Fx femoralflexor nerve dorsoventral relationship between the sacral plexus Gi inferiorgluteal nerve and the pudendal nerve in man by using computer Gs superiorgluteal nerve aided three-dimensional reconstruction imaging of La nerveto the levatorani serial sections of the second sacral nerve. -

Differential Movement of the Sciatic Nerve and Hamstrings During The
Musculoskeletal Science and Practice 43 (2019) 91–95 Contents lists available at ScienceDirect Musculoskeletal Science and Practice journal homepage: www.elsevier.com/locate/msksp Original article Differential movement of the sciatic nerve and hamstrings during the straight leg raise with ankle dorsiflexion: Implications for diagnosis of T neural aspect to hamstring disorders Elena Bueno-Graciaa,*,1, Albert Pérez-Bellmuntb,1, Elena Estébanez-de-Miguela, Carlos López-de-Celisb, Michael Shacklockc, Santos Caudevilla-Poloa, Vanesa González-Ruedab a Faculty of Health Sciences, University of Zaragoza, Zaragoza, Spain b Faculty of Medicine and Health Sciences, International University of Catalonia, Barcelona, Spain c Neurodynamic Solutions, Adelaide, Australia ARTICLE INFO ABSTRACT Keywords: Introduction: In hamstrings injuries, sciatic nerve and muscle disorders can coexist. Therefore, differential di- Biomechanics: diagnosis agnosis to include or exclude nerve involvement is an important aspect of evaluation. The objective of this paper Hamstrings is to investigate the mechanical behaviour of the sciatic nerve and biceps femoris muscle in the proximal thigh Sciatic nerve with the ankle dorsiflexion manoeuvre at different degrees of hip flexion during the straight leg raise in cadavers. Material and methods: A cross-sectional study was carried out. Linear displacement transducers were inserted into the sciatic nerve and the biceps femoris muscle of 11 lower extremities from 6 fresh cadavers to measure potential strain of both structures during ankle dorsiflexion at 0°, 30°, 60° and 90° of hip flexion during the straight leg raise. Excursion was also measured with a digital calliper. Results: Ankle dorsiflexion resulted in significant strain and distal excursion of the sciatic nerve at all ranges of hip flexion during the straight leg raise (p < 0.05). -

Nerves of the Lower Limb
Examination Methods in Rehabilitation (26.10.2020) Nerves of the Lower Limb Mgr. Veronika Mrkvicová (physiotherapist) Nerves of the Lower Limb • The Lumbar Plexus - Iliohypogastricus nerve - Ilioinguinalis nerve - Lateral Cutaneous Femoral nerve - Obturator nerve - Femoral nerve • The Sacral Plexus - Sciatic nerve - Tibial nerve - Common Peroneal nerve Spinal Nerves The Lumbar Plexus The Lumbar Plexus • a nervous plexus in the lumbar region of the body which forms part of the lumbosacral plexus • it is formed by the divisions of the four lumbar nerves (L1- L4) and from contributions of the subcostal nerve (T12) • additionally, the ventral rami of the fourth lumbar nerve pass communicating branches, the lumbosacral trunk, to the sacral plexus • the nerves of the lumbar plexus pass in front of the hip joint and mainly support the anterior part of the thigh The Lumbar Plexus • it is formed lateral to the intervertebral foramina and passes through psoas major • its smaller motor branches are distributed directly to psoas major • while the larger branches leave the muscle at various sites to run obliquely downward through the pelvic area to leave the pelvis under the inguinal ligament • with the exception of the obturator nerve which exits the pelvis through the obturator foramen The Iliohypogastric Nerve • it runs anterior to the psoas major on its proximal lateral border to run laterally and obliquely on the anterior side of quadratus lumborum • lateral to this muscle, it pierces the transversus abdominis to run above the iliac crest between that muscle and abdominal internal oblique • it gives off several motor branches to these muscles and a sensory branch to the skin of the lateral hip • its terminal branch then runs parallel to the inguinal ligament to exit the aponeurosis of the abdominal external oblique above the external inguinal ring where it supplies the skin above the inguinal ligament (i.e. -

A Study of Tibial Nerve Bifurcation and Branching Pattern of Calcaneal
International Journal of Anatomy and Research, Int J Anat Res 2016, Vol 4(1):2034-36. ISSN 2321-4287 Original Research Article DOI: http://dx.doi.org/10.16965/ijar.2016.139 A STUDY OF TIBIAL NERVE BIFURCATION AND BRANCHING PATTERN OF CALCANEAL NERVE IN THE TARSAL TUNNEL D.Malar Assistant Professor, JSS Medical College, JSS University, Mysore, Karnataka,India. ABSTRACT Background: Tibial nerve in the distal part of the leg branches into the calcaneal branch, medial plantar nerve and lateral plantat nerve.These branches inervate calcaneal,the medial plantar and the lateral plantar areas of the foot, respectively and carry sensory information from these areas. Tibial nerve and its branches show variation in branching pattern, and level of bifurcation. Detail knowledge of the anatomical variation of tibial nerve and its branches is essential for diagnosis and therapy tarsal tunnel syndrome, fractures requiring external nailing and nerve blocks. Materials and Methods: Tibial nerve and its branches in the tarsal tunnel were dissected and studied in twenty adult cadavers. Bifurcation levels of tibial nerve in relation to the Medio-malleolar-calcaneal axis were noted. The ramification pattern of medial calcaneal nerve was observed and studied. Results: In the present study tibial nerve bifurcation occurred within the tunnel in 100% cases. According to the level of bifurcation, 85% cases was type I, 10% cases was type II and 5%cases was type III. Medial calcaneal branches showed variations in number and origin, one medial calcaneal nerve was observed in 50% case , two in 20% cases and three in 10% of cases. The medial calcaneal nerve originated from the tibial nerve in85% cases. -

Low Level Division of the Sciatic Nerve and Its Clinical Significance - Case Report
Brunei Darussalam Journal of Health, 2015 6(1): 35-38 Low Level Division of the Sciatic Nerve and Its Clinical Significance - Case Report Rajendiran, R ¹ and Manivasagam, M² ¹Malliga College of Nursing, India ² Jerudong Park Medical Centre, Brunei Darussalam Abstract The anatomical knowledge regarding variation of the Sciatic nerve in the level of division and its location is of great importance in medical practise of neurology, orthopaedics, rehabilitation and anaesthesia. We report here a rare case of trifurcation of the Sciatic nerve of 50 year old male cadaver in the lower part of the popliteal fossa on the right side. Normally, the Sciatic nerve bifurcates into tibial and common peroneal nerve at the junction of the middle and lower thirds of the thigh, near the apex of the popliteal fossa. Low level division of the Sciatic nerve into three branches rarely occurs. In this case, the Sciatic nerve divided into tibial, common peroneal and peroneal communicating nerve. There was an absence of the Lateral sural nerve from the common peroneal nerve. This finding is of academic interest and clinical significance in performing effective injections at the popliteal crease for tibial and common peroneal nerve blocks and popliteal artery aneurysm surgeries. Key words: Sciatic nerve, trifurcation, popliteal fossa, nerve block, variation Introduction Sciatic nerve , the largest nerve of the body , is In the popliteal fossa, the tibial nerve gives branches derived from the anterior division of the L4 -S3 of muscular, genicular and medial sural cutaneous spinal roots and is nearly 2cm wide at its origin.1 It nerve. The common peroneal gives genicular divides into two terminal branches, namely the tibial branch, lateral sural nerve or lateral cutaneous (ventral division of ventral rami L4-S3) and common nerve of calf and peroneal communicating nerve peroneal nerve (Dorsal division of the ventral rami (PCN).