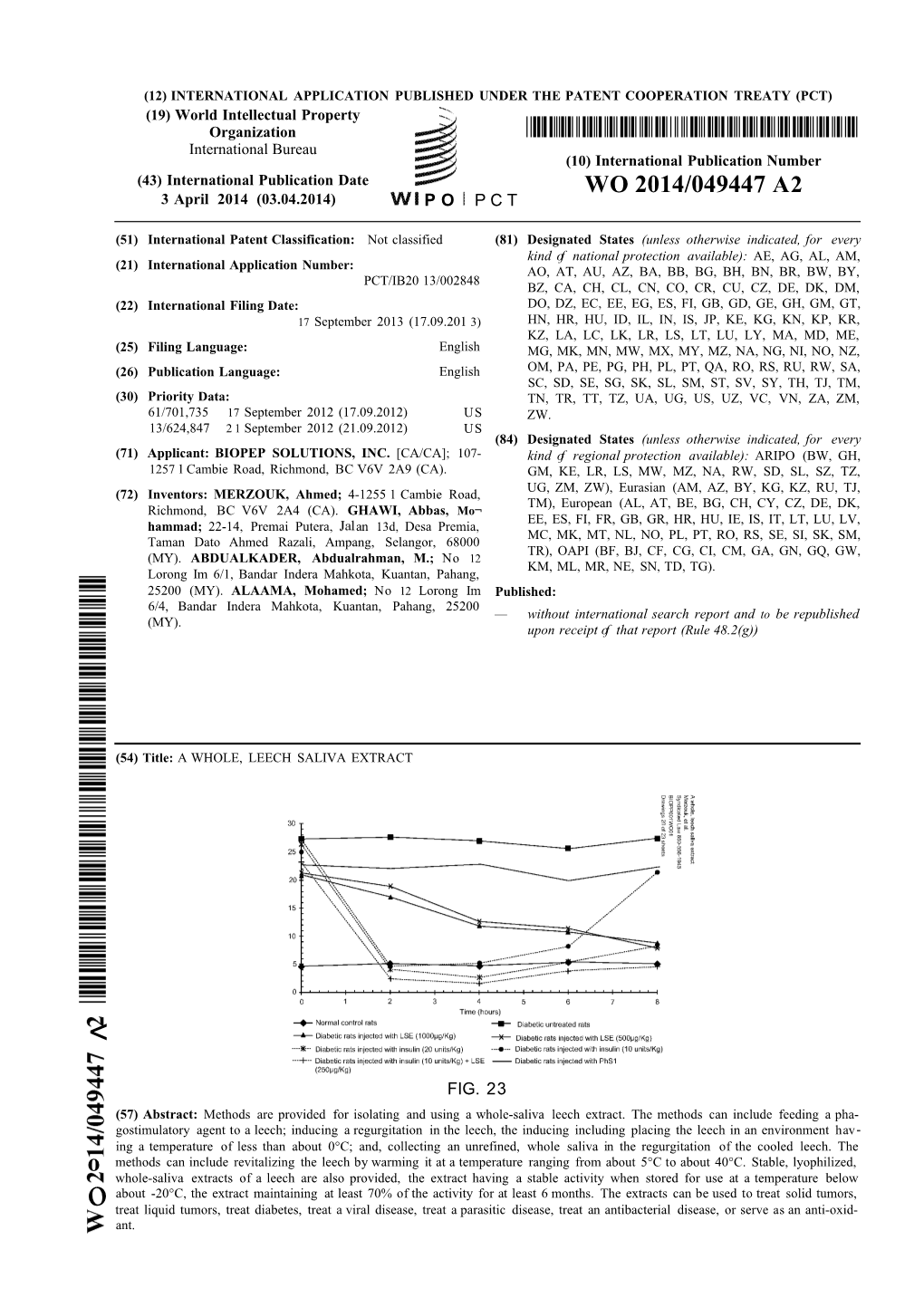
WO 2014/049447 A2 3 April 2014 (03.04.2014) P O P C T
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Review Article
Review Article Leech Therapeutic Applications A. M. ABDUALKADER*, A. M. GHAWI1, M. ALAAMA, M. AWANG AND A. MERZOUK2 Departments of Pharmaceutical Chemistry, and 1Basic Medical Science, Faculty of Pharmacy, International Islamic University Malaysia, Jalan Istana, 25200 Kuantan, Pahang, Malaysia, 2Biopep Solutions Inc., 235-11590 Cambie Road, Richmond, BC V6X 3Z5, Canada Abdualkader, et al.: Leeching Hematophagous animals including leeches have been known to possess biologically active compounds in their secretions, especially in their saliva. The blood‑sucking annelids, leeches have been used for therapeutic purposes since the beginning of civilization. Ancient Egyptian, Indian, Greek and Arab physicians used leeches for a wide range of diseases starting from the conventional use for bleeding to systemic ailments, such as skin diseases, nervous system abnormalities, urinary and reproductive system problems, inflammation, and dental problems. Recently, extensive researches on leech saliva unveiled the presence of a variety of bioactive peptides and proteins involving antithrombin (hirudin, bufrudin), antiplatelet (calin, saratin), factor Xa inhibitors (lefaxin), antibacterial (theromacin, theromyzin) and others. Consequently, leech has made a comeback as a new remedy for many chronic and life‑threatening abnormalities, such as cardiovascular problems, cancer, metastasis, and infectious diseases. In the 20th century, leech therapy has established itself in plastic and microsurgery as a protective tool against venous congestion and served -

Summary Record of the 26Th Meeting of the Animals Committee
Original language: English AC26 summary record CONVENTION ON INTERNATIONAL TRADE IN ENDANGERED SPECIES OF WILD FAUNA AND FLORA ____________ Twenty-sixth meeting of the Animals Committee Geneva (Switzerland), 15-20 March 2012 and Dublin (Ireland), 22-24 March 2012 SUMMARY RECORD Animals Committee matters 1. Opening of the meeting The Chair opened the meeting and welcomed all participants, before giving the floor to the Secretary- General, who also welcomed everyone and introduced new members of the Secretariat's scientific team (Mr De Meulenaer and Ms Kwitsinskaia) and enforcement team (Ms Garcia Ferreira, Ms Jonsson and Mr van Rensburg). He wished the Committee well in its deliberations. The Chair thanked the Secretary-General and invited suggestions as to how the Conference of the Parties could establish stronger measures to support the Committee as well as export countries, which deserved particular assistance. No other intervention was made during discussion of this item.1 2. Rules of Procedure The Secretariat introduced document AC26 Doc. 2 and proposed amending Rule 22 as follows: “On request, the Secretariat shall distribute printed and translated documents...”. The Secretariat explained that most members regularly indicated that they did not need printed copies and that this proposal was made to reduce costs. Although not opposed to the change in principle, a Party regretted that the suggestion had not been presented in the document, which would have given Parties time to consider it, and was concerned that this unannounced proposal might create a precedent. Another Party asked a question on the procedure to accept observers, but the Chair invited it to raise this topic under agenda item 4 on Admission of observers. -

AMNH-Scientific-Publications-2014
AMERICAN MUSEUM OF NATURAL HISTORY Fiscal Year 2014 Scientific Publications Division of Anthropology 2 Division of Invertebrate Zoology 11 Division of Paleontology 28 Division of Physical Sciences 39 Department of Earth and Planetary Sciences and Department of Astrophysics Division of Vertebrate Zoology Department of Herpetology 58 Department of Ichthyology 62 Department of Mammalogy 65 Department of Ornithology 78 Center for Biodiversity and Conservation 91 Sackler Institute for Comparative Genomics 99 DIVISION OF ANTHROPOLOGY Berwick, R.C., M.D. Hauser, and I. Tattersall. 2013. Neanderthal language? Just-so stories take center stage. Frontiers in Psychology 4, article 671. Blair, E.H., and Thomas, D.H. 2014. The Guale uprising of 1597: an archaeological perspective from Mission Santa Catalina de Guale (Georgia). In L.M. Panich and T.D. Schneider (editors), Indigenous Landscapes and Spanish Missions: New Perspectives from Archaeology and Ethnohistory: 25–40. Tucson: University of Arizona Press. Charpentier, V., A.J. de Voogt, R. Crassard, J.-F. Berger, F. Borgi, and A. Al- Ma’shani. 2014. Games on the seashore of Salalah: the discovery of mancala games in Dhofar, Sultanate of Oman. Arabian Archaeology and Epigraphy 25: 115– 120. Chowns, T.M., A.H. Ivester, R.L. Kath, B.K. Meyer, D.H. Thomas, and P.R. Hanson. 2014. A New Hypothesis for the Formation of the Georgia Sea Islands through the Breaching of the Silver Bluff Barrier and Dissection of the Ancestral Altamaha-Ogeechee Drainage. Abstract, 63rd Annual Meeting, Geological Society of America, Southeastern Section, April 10–11, 2014. 2 DeSalle, R., and I. Tattersall. 2014. Mr. Murray, you lose the bet. -

Pdf (351.78 K)
Neglected rare human parasitic infections: Part IV: Hirudiniasis Review Article Wael M Lotfy Department of Community Health Nursing, Faculty of Nursing, Matrouh University, Egypt ABSTRACT Among all species of leeches, only true leeches especially jawed leeches are known to attack humans. These species are either freshwater or land dwellers. Freshwater leeches of medical importance may be divided into two groups: leeches which attack the mucous membranes (endoparasites), and those that attack the skin (ectoparasites). Some species of the former group have been incriminated in causing halazoun, while many species of the latter group were used in bloodletting. Leeches may be potential transmitters of human pathogens. The land leeches are much less fearsome than the aquatic leeches. However, the harm which land leeches cause to man and his domestic animals may be such that some infested foci become true leeches as human parasites and their medical uses, and the recommended methods of prevention almostand control. uninhabitable. This review summarizes current knowledge on the public health significance of Keywords: Annelida, leech, man, public health, segmented worms. Received: 17 January, 2021, Accepted: 22 February, 2021. Corresponding Author: Wael M Lotfy, Tel.: +20 1008154959, E-mail: [email protected] Print ISSN: 1687-7942, Online ISSN: 2090-2646, Vol. 14, No. 1, April, 2021. True leeches (Hirudinea: Euhirudinea) are They colonise freshwater (Hirudidae or Hirudinidae) segmented worms belonging to the phylum Annelida. and terrestrial (Haemadipsidae and Xerobdellidae) Some species are marine, others are terrestrial, and environments[1,3,5,7]. The hematophagous leeches are the majority are freshwater dwellers[1]. They are usually not particular about their victims. -

Seasonal Variation in the Occurrence of the Medicinal Leech Hirudo Orientalis in Guilan Province, Iran
Vol. 11: 289–294, 2011 AQUATIC BIOLOGY Published online February 23 doi: 10.3354/ab00310 Aquat Biol Seasonal variation in the occurrence of the medicinal leech Hirudo orientalis in Guilan Province, Iran K. Darabi-Darestani, M. Malek* University of Tehran, School of Biology, College of Science, University of Tehran, Tehran, Iran ABSTRACT: Two small populations of medicinal leeches Hirudo orientalis Utevsky & Trontelj, 2005 were sampled monthly over the course of a year (November 2008 to October 2009) in 2 separate regions of Guilan Province in northern Iran. Environmental factors, including host availability, tem- perature and vegetation density (biomass in g km–2) were analyzed to assess their impact on leech populations. The study areas supported only low densities (ind. km–2) of medicinal leeches, mostly due to agricultural activity which has caused habitat destruction and has gradually limited the distri- bution of leeches to small, patchy bodies of water. Agricultural activity is seasonal, so leeches are not affected by this activity equally year round. Leeches were most abundant in May/June, were present in small numbers in July/August, and hibernated from December to March 2009 at both sites. Leech density was significantly correlated with amphibian density (biomass in g km–2), the major hosts in the sample areas. Temperature and aquatic vegetation densities affected leech numbers directly (temperature influencing leech growth rate and vegetation providing shelter from potential preda- tors) and indirectly (due to the impact of temperature and vegetation on the amphibian population, the leeches’ major prey). Leeches of <1 g were found mostly in April and May following hatching, while those >5 g were predominant in September. -

NRCEIM 2017 Proceeding
PROCEEDINGS National Research Conference and Exhibition on Indigenous Medicine NRCEIM-2017 Towards Healthy Life With Nature ABSTRACTS Unit of Siddha Medicine University of Jaffna Kaithady, Jaffna, Sri Lanka 27-29 January 2017 Proceedings of the National Research Conference & Exhibition on Indigenous Medicine (NRCEIM - 2017) © Copy Rights : Unit of Siddha Medicine, University of Jaffna. Published : Unit of Siddha Medicine, University of Jaffna, Kaithady, Jaffna, Sri Lanka Telephone No. : 021 20 57146 Web : www.siddha.jfn.ac.lk Printed by : Andra Printers No.379, Kasthuriyar Road, Jaffna, Sri Lanka. ISBN : 978-955-0585-13-7 This Proceeding book is the copy right property of the unit of Siddha Medicine, University of Jaffna, Kaithady, Sri Lanka. The Editorial Board has made considerable efforts to present accurate and reliable information in this Proceedings. However, Editorial Board does not take any legal responsibility for the accuracy, completeness, usefulness, plagiarism or copy right issues of the Information herein List of Reviewers Snr. Prof. (Ms.) V. Arasaratnam University of Jaffna Prof. G. Mikunthan University of Jaffna Prof. I. Sornamariammal Former Joint Director, Indian Medicine and Homoeopathy Prof. M. Logamanian National Institute of Siddha, Chennai, India. Prof. (Ms.) V. Thevanesam University of Peradeniya Prof. K. Sivapalan University of Jaffna Prof. S. V. Parameswaran Retired Professor, University of Jaffna Prof. S. Noble Surendran University of Jaffna Prof. R. Sivakanesan Retired Professor, University of Peradeniya Prof. (Mrs.) E. R. H. S. S. Ediri- Institute of Indigenous Medicine, University of Colombo weera Prof. P. Jeyadevan University of Jaffna Prof. Piyal Marasinghe Ministry of Health and Indigenous Medicine, Uva Prov- ince, Prof. -

Far Beyond Common Leeching: Insights Into an Ancient Medical Device Through Integrated Omics Data Vladislav V
bioRxiv preprint doi: https://doi.org/10.1101/357681; this version posted June 28, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Far beyond common leeching: insights into an ancient medical device through integrated omics data Vladislav V. Babenko1*, Oleg V. Podgorny1,2, Valentin A. Manuvera1,3, Artem S. Kasianov3,4, Alexander I. Manolov1, Ekaterina N. Grafskaia1,3, Dmitriy A. Shirokov1, Alexey S. Kurdyumov1, Dmitriy V. Vinogradov5,6, Anastasia S. Nikitina1, Sergey I. Kovalchuk1,7, Nickolay A. Anikanov1,7, Ivan O. Butenko1, Maria T. Vakhitova1,3, Olga V. Pobeguts1, Daria S. Matushkina1, Daria V. Rakitina1, Daria D. Kharlampieva1, Nadezhda F. Polina1, Pavel A. Bobrovsky1, Elena S. Kostryukova1, Victor G. Zgoda8, Isolda P. Baskova9, Mikhail S. Gelfand5,6,10,11, Vadim M. Govorun1,3,, Vassili N. Lazarev 1,3 1Federal Research and Clinical Centre of Physical-Chemical Medicine of Federal Medical Biological Agency, 1a Malaya Pirogovskaya Str., Moscow 119435, Russia 2Koltzov Institute of Developmental Biology, Russian Academy of Sciences, 26 Vavilov str., Moscow 119334, Russia 3Moscow Institute of Physics and Technology, 9 Institutskiy per., Dolgoprudny, Moscow Region 141700, Russia 4Vavilov Institute of General Genetics, Russian Academy of Sciences, 3 Gubkina str., Moscow 119991, Russia 5A.A.Kharkevich Institute for Information Transmission Problems, Russian Academy of Sciences, 19 Bol'shoi Karetnyi per., Moscow 127051, Russia 6Skolkovo Institute of Science and Technology, 3 Nobelya Ulitsa str., Moscow 121205, Russia 7Shemyakin-Ovchinnikov Institute of Bioorganic Chemistry, Russian Academy of Sciences, 16/10 Miklukho-Maklaya str., Moscow 117997, Russia 8V.N. -

Freshwater Leeches (Clitellata: Hirudinida) of South-Western Iran: Small Area - High Diversity
Correspondence ISSN 2336-9744 (online) | ISSN 2337-0173 (print) The journal is available on line at www.biotaxa.org/em Freshwater leeches (Clitellata: Hirudinida) of south-western Iran: Small area - High diversity SARA RAHMANIPANAH1, HAMID BELGHEISZADEH2*, KAVEH DARABI DARESTANI3 & HORA JALAI TEHRANI4 1 Department of Biology, School of advanced sciences in regenerative medicine, Tehran Medical Sciences Branch, Islamic Azad University, Tehran, Iran. Email address: [email protected] 2* Department of Parasitology and Entomology, Islamic Azad University Tehran Medical Branch, Tehran, Iran 3Zoology Department, School of Biological Sciences and Center of Excellence in Phylogeny of Living Organisms, College of Sciences, University of Tehran, Tehran, Iran. Email: [email protected] 4 Department of Biology, School of advanced sciences in regenerative medicine, Tehran Medical Sciences Branch, Islamic Azad University, Tehran, Iran. Email: [email protected] *Corresponding author: [email protected] Received 29 October 2015 │ Accepted 11 November 2015 │ Published online 15 November 2015. Leeches (Annelida: Hirudinida) are one of the most important benthic invertebrates in different aquatic habitats since they have different roles such as predators, preys or parasites (Sawyer 1986). Iran is a country in Middle East (south western part of Palaearctic) that has not been studied comprehensively regarding leech diversity (e.g. Bennike 1940; Gholami 2005; Grosser & Pešić 2006; Grosser & Pešić 2008; Grosser et al. 2011, Salimi et al. 2011; Mirzaei et al. 2007; Darabi Darestani & Malek 2011a, b). Esfahan freshwater eco-region is considered as one of the smallest eco-regions (out of 11 eco- regions in Iran, Abell et al. 2008) and it has one basin named as Isfahan which is an endorheic basin for Zayande Rood River. -

Hirudinea: Arhynchobdellida: Hirudinidae) in Romania
Travaux du Muséum National d’Histoire Naturelle © Décembre Vol. LIII pp. 7–11 «Grigore Antipa» 2010 DOI: 10.2478/v10191-010-0001-z THE FIRST RECORDED OCCURRENCE OF HIRUDO VERBANA CARENA, 1820 (HIRUDINEA: ARHYNCHOBDELLIDA: HIRUDINIDAE) IN ROMANIA ADRIAN GAGIU Abstract. In 2005, a Hirudo verbana specimen was observed in Stracoº Valley, within the Tãºad Reserve (Bihor county, north-western Romania). Since the coloration pattern of this once forgotten species matches its genetic differentiation, the identification of the specimen as belonging to the south- eastern European H. verbana appears plausible. The species was previously cited in southern, central and eastern Europe, but not in Romania. Therefore, the present observation might be its first recognized occurrence in the country. As recently pointed out, H. verbana is one of the three species commonly known as the European medicinal leech and the most abundant as such. Most international and national conservation legislation containing only H. medicinalis (including IUCN, CITES, Berne Convention) needs completion, according to the new taxonomy. Résumé. Un spécimen d’Hirudo verbana a été observé en 2005 dans la vallée Stracoº de la réservation naturelle Tãºad (Bihor, dans le nord-ouest de la Roumanie). Lorsque le modèle de la coloration de cette espèce récemment révalidée correspond à sa caractérisation génétique, l’identification du spécimen observé est plausible. L’aréal connu d’Hirudo verbana comprend le sud, le centre et l’est de l’Europe, mais pas la Roumanie, donc cette obsérvation est la première occurence documentée dans ce pays. Récemment a été démontré que H. verbana est une des trois espèces de sangsues médicinales européennes et la plus utilisée. -
Conservation, Acquisition, and Maturation of Gut and Bladder Symbioses in Hirudo Verbana
Conservation, Acquisition, and Maturation of Gut and Bladder Symbioses in Hirudo verbana a dissertation presented by Emily Ann McClure to The Department of Cell and Molecular Biology in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the subject of Microbiology University of Connecticut Storrs, Connecticut August 2019 ©2019 – Emily Ann McClure all rights reserved. Thesis advisor: Professor Joerg Graf Emily Ann McClure Conservation, Acquisition, and Maturation of Gut and Bladder Symbioses in H. verbana Abstract The medicinal leech is a developing experimental model of gut symbioses. Aeromonas veronii and Mucinivorans hirudinis are core members of the gut microbial community in H. verbana and may aid the leech in digesting the blood meal, preserving the blood meal, and keeping invading bacteria from coloniz- ing the gut. The bladders of H. verbana contain an entirely different microbial consortium. The scientific interest in this symbiosis is currently due to its simple nature and the extreme dietary habits of the leech. In order to increase the usefulness of this model, a more sophisticated understanding of processes by which the microbiome is acquired and develops is necessary. In my dissertation I have compared the gut and blad- der microbiomes of H. verbana to that of Macrobdella decora (the North American medicinal leech) in order to determine the conservation of symbionts. I have additionally examined the potential for horizontal and vertical transmission of gut and bladder symbionts to hatchling and juvenile H. verbana. With such information, future researchers will be able to draw parallels between processes occurring in the leech to those occurring in other organisms. -
Reproduction Efficiency of the Medicinal Leech Hirudo Verbana Carena
www.trjfas.org ISSN 1303-2712 Turkish Journal of Fisheries and Aquatic Sciences 15: 411-418 (2015) DOI: 10.4194/1303-2712-v15_2_27 Reproduction Efficiency of the Medicinal Leech Hirudo verbana Carena, 1820 Mustafa Ceylan1,*, Osman Çetinkaya2, Ramazan Küçükkara1, Ufuk Akçimen1 1 Fisheries Research Institute, Eğirdir, Isparta, Turkey. 2 University of Süleyman Demirel, Eğirdir Fisheries Faculty, Isparta, Turkey. * Corresponding Author: Tel.:+90.246 3133460; Fax:+90.246 3133463; Received 14 January 2015 E-mail: [email protected] Accepted 21 May 2015 Abstract The aim of the study was to investigate the reproduction efficiency of a medicinal leech Hirudo verbana Carena, 1820. Totally 25 gravid medicinal leeches weighted 5.70±3.22 g were used. The leeches deposited 3.20±1.87 cocoons by losing 23.46±5.42% in body weight in every cocooning at 9.67±3.68 days intervals. The cocoons, having a weight 0.93±0.38 g, diameter 13.81±2.26 mm and length 21.44±3.81 mm, had 12.29±5.14 offspring weighted 29.11±13.62 mg. It was determined the negative correlation between the adult leeches weight and the weight loss percentage after each cocoon deposition, between the adult leeches weight and the cocoon deposition frequency, and between the number of offspring and the mean weight of them. The positive correlation was found between the adult leech weights and the number of the laid cocoons, between the adult leech weight and the laid cocoon weight, and between the cocoon weight and the number of offspring. H. verbena shows strong reproduction effort, it can reproduce even loosing 70% their initial weights. -

Draft Genome Sequences of Hirudo Medicinalis and Salivary Transcriptome of Three Closely Related Medicinal Leeches Vladislav V
Babenko et al. BMC Genomics (2020) 21:331 https://doi.org/10.1186/s12864-020-6748-0 RESEARCH ARTICLE Open Access Draft genome sequences of Hirudo medicinalis and salivary transcriptome of three closely related medicinal leeches Vladislav V. Babenko1* , Oleg V. Podgorny1,2, Valentin A. Manuvera1,3, Artem S. Kasianov3,4, Alexander I. Manolov1, Ekaterina N. Grafskaia1,3, Dmitriy A. Shirokov1, Alexey S. Kurdyumov1, Dmitriy V. Vinogradov5,6, Anastasia S. Nikitina1,3, Sergey I. Kovalchuk1,7, Nickolay A. Anikanov1,7, Ivan O. Butenko1, Olga V. Pobeguts1, Daria S. Matyushkina1, Daria V. Rakitina1, Elena S. Kostryukova1, Victor G. Zgoda8, Isolda P. Baskova9, Vladimir M. Trukhan10, Mikhail S. Gelfand5,6,11,12, Vadim M. Govorun1,3, Helgi B. Schiöth10,13 and Vassili N. Lazarev1,3 Abstract Background: Salivary cell secretion (SCS) plays a critical role in blood feeding by medicinal leeches, making them of use for certain medical purposes even today. Results: We annotated the Hirudo medicinalis genome and performed RNA-seq on salivary cells isolated from three closely related leech species, H. medicinalis, Hirudo orientalis, and Hirudo verbana. Differential expression analysis verified by proteomics identified salivary cell-specific gene expression, many of which encode previously unknown salivary components. However, the genes encoding known anticoagulants have been found to be expressed not only in salivary cells. The function-related analysis of the unique salivary cell genes enabled an update of the concept of interactions between salivary proteins and components of haemostasis. Conclusions: Here we report a genome draft of Hirudo medicinalis and describe identification of novel salivary proteins and new homologs of genes encoding known anticoagulants in transcriptomes of three medicinal leech species.