Therapeutic Class Overview Ophthalmic Antihistamines
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Allergies Your Amerigroup Community Care Patients May Experience a Pharmacy Claim Rejection When Prescribed Nonpreferred Products
Provider update Hot Tip: Allergies Your Amerigroup Community Care patients may experience a pharmacy claim rejection when prescribed nonpreferred products. To avoid additional steps or delays at the pharmacy, consider prescribing preferred products whenever possible. Utilization Management edits may apply to select preferred products. Coverage should be verified by reviewing the Preferred Drug List (PDL) on the Amerigroup provider website. The PDL is subject to change quarterly. Therapeutic class Preferred products Nonpreferred products Oral • Fexofenadine (generic Allegra) • Cetirizine (generic Zyrtec) antihistamines1 • Fexofenadine/ pseudoephedrine • Cetirizine/pseudoephedrine (generic Allegra-D) (generic Zyrtec D) • Loratadine (generic Claritin) • Zyrtec (cetirizine) • Loratadine/pseudoepherine • Zyrtec D (cetirizine/ (generic Claritin D) pseudoephedrine) • Clarinex (desloratadine) • Desloratadine (generic Clarinex) • Alegra (fexofenadine) • Allegra D (fexofenadine/ pseudoephedrine) • Levocetirizine (generic Xyzal) • Xyzal (levocetirizine) • Claritin (loratadine) • Claritin D (loratadine/ pseudoephedrine) Nasal steroids2 • OTC budesonide nasal spray • Flonase Sensimist (fluticasone (generic Rhinocort) furoate) • OTC Rhinocort Allergy • Flonase (fluticasone propionate) (budesonide) • Rx fluticasone propionate (generic • OTC fluticasone propionate Rx Flonase) (generic Flonase) • Mometasone furoate (generic • OTC triamcinolone acetonide Nasonex) (generic Nasacort) • Nasacort (triamcinolone acetonide) • Nasonex (mometasone furoate) • Omnaris -

Treatment of Allergic Conjunctivitis with Olopatadine Hydrochloride Eye Drops
REVIEW Treatment of allergic conjunctivitis with olopatadine hydrochloride eye drops Eiichi Uchio Abstract: Olopatadine hydrochloride exerts a wide range of pharmacological actions such as histamine H receptor antagonist action, chemical mediator suppressive action, and eosinophil Department of Ophthalmology, 1 Fukuoka University School of infi ltration suppressive action. Olopatadine hydrochloride 0.1% ophthalmic solution (Patanol®) Medicine, Fukuoka, Japan was introduced to the market in Japan in October 2006. In a conjunctival allergen challenge (CAC) test, olopatadine hydrochloride 0.1% ophthalmic solution signifi cantly suppressed ocular itching and hyperemia compared with levocabastine hydrochloride 0.05% ophthalmic solution, and the number of patients who complained of ocular discomfort was lower in the olopatadine group than in the levocabastine group. Conjunctival cell membrane disruption was observed in vitro in the ketotifen fumarate group, epinastine hydrochloride group, and azelastine hydrochloride group, but not in the olopatadine hydrochloride 0.1% ophthalmic solution group, which may potentially explain the lower discomfort felt by patients on instillation. Many other studies in humans have revealed the superiority of olopatadine 0.1% hydrochloride eye drops to several other anti-allergic eye drops. Overseas, olopatadine hydrochloride 0.2% ophthalmic solution for a once-daily regimen has been marketed under the brand name of Pataday®. It is expected that olopatadine hydrochloride ophthalmic solutions may be used in patients with a more severe spectrum of allergic conjunctival diseases, such as vernal keratoconjunctivitis or atopic keratoconjunctivitis, in the near future. Keywords: olopatadine, eye drop, allergic conjunctivitis, anti-histaminergic Introduction The prevalence of allergic conjunctival diseases (ACD) in Japan is estimated to be as high as 15%–20% of the population and is on the rise. -

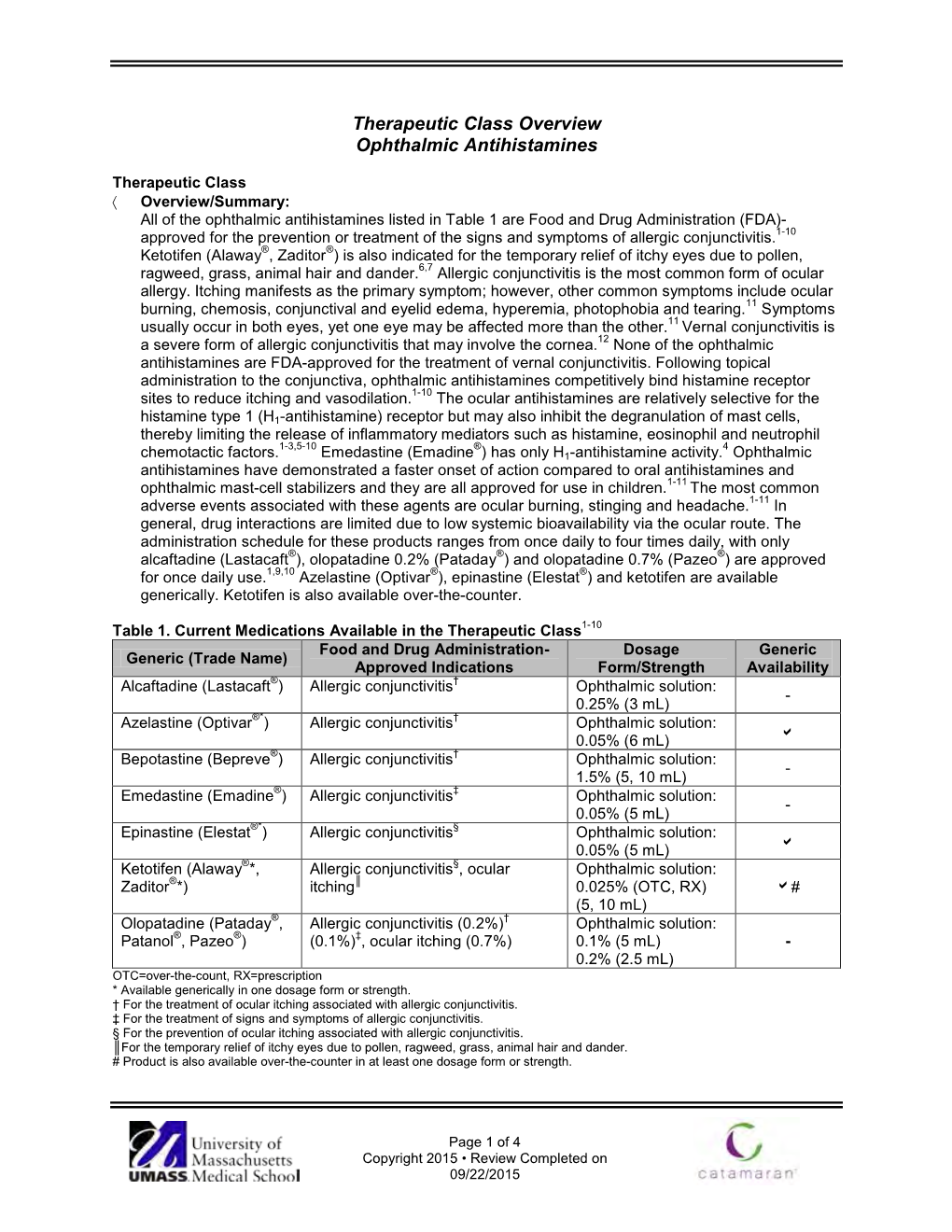
Ophthalmic Antihistamines
Ophthalmics for Allergic Conjunctivitis Review 04/12/2011 Copyright © 2004 - 2011 by Provider Synergies, L.L.C. All rights reserved. Printed in the United States of America. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage and retrieval system without the express written consent of Provider Synergies, L.L.C. All requests for permission should be mailed to: Attention: Copyright Administrator Intellectual Property Department Provider Synergies, L.L.C. 10101 Alliance Rd, Ste 201 Cincinnati, Ohio 45242 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, -

Medication Instructions for Allergy Patients
MEDICATION INSTRUCTIONS FOR ALLERGY PATIENTS Drugs which contain antihistamine or have antihistaminic effects can result in negative reactions to skin testing. As a result, it may not be possible to properly interpret skin test results, and testing may have to be repeated at a later date. While this list is extensive, it is NOT all inclusive (particularly of the various brand names). Discontinue ALL antihistamines including the following medications seven (7) days prior to skin testing (unless longer time specified): Antihistamines – Generic name (Brand name(s)): Cetirizine (Zyrtec, Zyrtec-D) Hydroxyzine (Vistaril, Atarax) Desloratadine (Clarinex) Levocetirizine (Xyzal) Fexofenadine (Allegra, Allegra-D) Loratadine (Claritin, Claritin-D, Alavert) Diphenhydramine (Aleve PM, Benadryl, Bayer P.M., Benylin, Contac P.M., Doans P.M, Excedrin PM, Legatrin P.M.. Nytol, Tylenol Nighttime, Unisom, Zzzquil) Chlorpheniramine (Aller-Chlor, Allerest, Alka Seltzer Plus, Chlor-Trimeton, Comtrex, Contac, Co-Pyronil, Coricidin, CTM, Deconamine, Dristan, Dura-tap, Naldecon, Ornade Spansules, Rondec, Sinutab, Teldrin, Triaminic, Triaminicin, Tylenol Allergy) Azatadine (Optimine, Trinalin) Doxylamine (Nyquil) Brompheniramine (Bromfed, Dimetane, Dimetapp) Meclizine (Antivert) Carbinoxamine (Clistin, Rondec) Pheniramine Clemastine (Tavist) Phenyltoloxamine (Nadecon) Cyclizine (Marezine) Promethazine (Phenergan) Cyprohepatidine (Periactin) (9 days) Pyrilamine (Mepyramine) Dexbrompheniramine (Drixoral) Quinacrine (Atabrine) Dexchlorpheniramine (Extendryl, Polaramine) -

22134 Alcaftadine Clinical PREA
Clinical Review Martin P Nevitt M.D., M.P.H NDA 22-134 (b) (4) (alcaftadine ophthalmic solution) 0.25% CLINICAL REVIEW Application Type NDA Application Number(s) 22-134 Priority or Standard S Submit Date(s) September 29, 2009 Received Date(s) September 29, 2009 PDUFA Goal Date July 28, 2010 Division / Office DAIOP Reviewer Name(s) Martin P. Nevitt, M.D.,M.P.H. Review Completion Date April 2, 2010 Established Name alcaftadine ophthalmic solution, 0.25% (Proposed) Trade Name Lastacaft Therapeutic Class histamine H1 receptor antagonist Applicant Vistakon Pharmaceuticals, LLC Formulation(s) Topical ophthalmic Dosing Regimen One drop each eye daily Indication(s) Prevention of itching associated with allergic conjunctivitis Intended Population(s) Patients ≥ 2 years old 1 Clinical Review Martin P Nevitt M.D., M.P.H NDA 22-134 (b) (4) (alcaftadine ophthalmic solution) 0.25% Table of Contents 1 RECOMMENDATIONS/RISK BENEFIT ASSESSMENT......................................... 5 1.1 Recommendation on Regulatory Action ............................................................. 5 1.2 Risk Benefit Assessment.................................................................................... 5 1.3 Recommendations for Postmarket Risk Evaluation and Mitigation Strategies ... 5 1.4 Recommendations for Postmarket Requirements and Commitments ................ 5 2 INTRODUCTION AND REGULATORY BACKGROUND ........................................ 5 2.1 Product Information ........................................................................................... -

Medications That May Interfere with Skin Testing
MEDICATIONS THAT MAY INTERFERE WITH SKIN TESTING • Due to continued advances, not all medications may be listed at time of printing. • For your safety and accurate results, at each visit, please list all your current medications (including non-prescription and those prescribed elsewhere). • It is important to let us know if you are pregnant or could be pregnant. STOP THESE MEDICATIONS FIVE DAYS BEFORE SKIN TESTING: ORAL ANTIHISTAMINES: ANTIHISTAMINE NOSE SPRAYS: • Allegra (Fexofenadine) • Astelin, Astepro, Dymista (Azelastine) • Benadryl (Diphenhydramine) • Patanase (Olopatadine) • Claritin, Alavert (Loratadine) • Clarinex (Desloratadine) ANTIHISTAMINE EYE DROPS: • Xyzal (Levocetirizine) • Alaway, Claritin, Zaditor, Zyrtec (Ketotifen) • Zyrtec (Cetirizine) • Bepreve (Bepotastine) • Cyproheptadine • Elestat (Epinastine) · All over-the-counter medications for allergy, cough, cold, sleep, • Emadine (Emedastine) or nausea that include: • Lastacaft (Alcaftadine) oAcrivastine (ex. Semprex) • Livostin (Levocabastine) oAzatadine (ex. Optimine, Trinalin) • Naphcon-A, Opcon-A, Visine-A oBrompheniramine (ex. Dimetapp) (Pheniramine) oCarbinoxamine (ex. Palgic, Arbinoxa) • Optivar (Azelastine) oChlorpheniramine (ex. Actifed, Aller-chlor, Chlor- • Pataday, Patanol (Olopatadine) Trimeton, Tylenol Allergy) oDimenhydrinate (ex. Dramamine) HEARTBURN MEDICATIONS (H2 BLOCKERS): oDiphenhydramine (ex. Unisom, Sominex, • Axid (Nizatidine) Triaminic, many with “PM” in the title) • Pepcid, Tums Dual Action (Famotidine) oDoxylamine (ex. Nyquil, Unisom) • Tagament -
![Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set](https://docslib.b-cdn.net/cover/8870/ehealth-dsi-ehdsi-v2-2-2-or-ehealth-dsi-master-value-set-1028870.webp)
Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set
MTC eHealth DSI [eHDSI v2.2.2-OR] eHealth DSI – Master Value Set Catalogue Responsible : eHDSI Solution Provider PublishDate : Wed Nov 08 16:16:10 CET 2017 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 1 of 490 MTC Table of Contents epSOSActiveIngredient 4 epSOSAdministrativeGender 148 epSOSAdverseEventType 149 epSOSAllergenNoDrugs 150 epSOSBloodGroup 155 epSOSBloodPressure 156 epSOSCodeNoMedication 157 epSOSCodeProb 158 epSOSConfidentiality 159 epSOSCountry 160 epSOSDisplayLabel 167 epSOSDocumentCode 170 epSOSDoseForm 171 epSOSHealthcareProfessionalRoles 184 epSOSIllnessesandDisorders 186 epSOSLanguage 448 epSOSMedicalDevices 458 epSOSNullFavor 461 epSOSPackage 462 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 2 of 490 MTC epSOSPersonalRelationship 464 epSOSPregnancyInformation 466 epSOSProcedures 467 epSOSReactionAllergy 470 epSOSResolutionOutcome 472 epSOSRoleClass 473 epSOSRouteofAdministration 474 epSOSSections 477 epSOSSeverity 478 epSOSSocialHistory 479 epSOSStatusCode 480 epSOSSubstitutionCode 481 epSOSTelecomAddress 482 epSOSTimingEvent 483 epSOSUnits 484 epSOSUnknownInformation 487 epSOSVaccine 488 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 3 of 490 MTC epSOSActiveIngredient epSOSActiveIngredient Value Set ID 1.3.6.1.4.1.12559.11.10.1.3.1.42.24 TRANSLATIONS Code System ID Code System Version Concept Code Description (FSN) 2.16.840.1.113883.6.73 2017-01 A ALIMENTARY TRACT AND METABOLISM 2.16.840.1.113883.6.73 2017-01 -

Association of Pediatric Atopic Dermatitis and Cataract Development and Surgery
Supplementary Online Content Jeon HS, Choi M, Byun SJ, Hyon JY, Park KH, Park SJ. Association of pediatric atopic dermatitis and cataract development and surgery. JAMA Ophthamol. Published online June 7, 2018. doi:10.1001/jamaophthalmol.2018.2166 eTable 1. List of diagnostic codes used for defining subjects eTable 2. Drug lists used for defining atopic dermatitis eTable 3. Baseline characteristics of atopic dermatitis cohort and control group eTable 4. Cox analysis-derived hazard ratios (HRs) and 95% confidence intervals (CIs) of cataract development associated with atopic dermatitis (AD) and its covariates eTable 5. Cox analysis-derived hazard ratios (HRs) and 95% confidence intervals (CIs) of cataract surgery associated with atopic dermatitis (AD) and its covariates This supplementary material has been provided by the authors to give readers additional information about their work. © 2018 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 09/24/2021 eTable 1. List of diagnostic codes used for defining subjects Diagnoses Code numbers in KCD-6a Atopic dermatitis L20 Cataract H25, H26 Congenital malformation of eyes (anopthalmos, microphthalmos, and Q11 macrophthalmos) Congenital lens malformation Q12 Congenital malformation of anterior segment of eyes Q13 Congenital malformation of posterior segment of eyes Q14 Other congenital malformations of eyes Q15 Cataract surgery S5110, S5111, S5112, S5119 Asthma J45.0, J45.9 Allergic rhinitis J30.1, J30.2, J30.3, J30.4 aThe diagnosis was coded according to the Korean Classification of Disease, 6th edition (KCD-6, a version of the International Classification of Diseases, 10th edition, adapted for the Korean healthcare system). © 2018 American Medical Association. -

ยากลุ่ม Ophthalmic Anti-Allergics No. ชื่อยา รูปแบบ สรุปเหตุผลกา 1
ยากลุ่ม Ophthalmic Anti-allergics No. ชื่อยา รูปแบบ สรุปเหตุผลการเลือกยา 1 Sodium cromoglicate eye drop บัญชี ค (Disodium เงื่อนไข (ไม่ระบุ) Cromoglycate /Cromolyn sodium ) 2 Lodoxamide eye drop ไม่คัดเลือกไว้ในบัญชี trometramine เหตุผล ไม่คัดเลือกตามบัญชียาหลัก พศ.2551 3 Naphazoline HCl eye drop ไม่คัดเลือกไว้ในบัญชี เหตุผล ไม่คัดเลือกตามบัญชียาหลัก พศ.2551 4 Naphazoline HCl+ eye drop และไม่ผ่าน ISafE score Pheniramine maleate 5 Naphazoline nitrate + eye drop zinc sulfate 6 Olopatadine eye drop ไม่คัดเลือกไว้ในบัญชี hydrochloride เหตุผล ไม่มีข้อมูลหลักฐานที่ชัดเจนว่ามีประสิทธิภาพ 7 Ketotifen fumarate eye drop หรือความปลอดภัยเหนือกว่ายา Sodium cromoglicate 8 Antazoline HCl eye drop บัญชี ก +Tetrahydrozoline HCl เงื่อนไข (ไม่ระบุ) 9 Tetrahydrozoline HCl eye drop ไม่คัดเลือกไว้ในบัญชี เหตุผล ไม่คัดเลือกตามบัญชียาหลัก พ.ศ.2551 10 Epinastine HCl eye drop และไม่ผ่าน ISafE score 11 Pemirolast potassium eye drop 12 Emedastine fumarate eye drop ไม่คัดเลือกไว้ในบัญชี เหตุผล ไม่คัดเลือกตามบัญชียาหลัก พ.ศ.2551 และผู้ผลิตได้ยกเลิกทะเบียนแล้ว ส่วนท่ ี 1 ข้อมูลโดยสรุป กลุ่มยาทางเลือกแรกในการรักษาอาการเยื่อบุตาอักเสบจากการแพ้ ได้แก่ topical antihistamines และ mast cell stabilizers ยาทางเลือกอื่นเป็นสูตรผสม separate topical mast cell stabilizer และ topical antihistamine ได้แก่ olopatadine, azelastine HCl, epinastine,pemirolast potassium, และ ketotifen fumarate ข้อมูลด้านประสิทธิผลพบว่า US.FDA อนุมัติ Olopatadine ข้อบ่งใช้ Allergic conjunctivitis ในผู้ใหญ่และ เด็กอายุ 3 ปีขึ้นไป, Ketotifen ข้อบ่งใช้ Allergic conjunctivitis - Itching; Prophylaxis ในผู้ใหญ่และเด็กอายุ -

USP Medicare Model Guidelines V6.0 Page 1 of 56
USP Medicare Model Guidelines v6.0 Page 1 of 56 ABCDE Example Part D USP Category USP Class Salt/Ester Change language 2 Eligible Drugs* 3 Analgesics Nonsteroidal Anti-inflammatory 4 Drugs 5 Celecoxib 6 Diclofenac Potassium 7 Diflunisal 8 Etodolac 9 Fenoprofen Calcium 10 Flurbiprofen 11 Ibuprofen 12 Indomethacin 13 Ketoprofen 14 Ketorolac Tromethamine 15 Meclofenamate 16 Mefenamic Acid 17 Meloxicam 18 Nabumetone 19 Naproxen 20 Oxaprozin 21 Piroxicam 22 Sulindac 23 Tolmetin 24 Opioid Analgesics, Long-acting 25 Hydromorphone 26 Fentanyl 27 Levorphanol Tartrate 28 Methadone Hydrochloride 29 Morphine Sulfate 30 Oxycodone Hydrochloride 31 Oxymorphone Hydrochloride 32 Tramadol Hydrochloride 33 Opioid Analgesics, Short-acting 34 Butorphanol Tartrate 35 Codeine Phosphate 36 Fentanyl Citrate 37 Hydromorphone Hydrochloride * This list is illustrative of Part D eligible drugs only, and does not infer CMS coverage Changes from USP MMGv5.0 marked in red USP Medicare Model Guidelines v6.0 Page 2 of 56 ABCDE Example Part D USP Category USP Class Salt/Ester Change language 2 Eligible Drugs* 38 Meperidine Hydrochloride 39 Nalbuphine Hydrochloride 40 Oxycodone Hydrochloride 41 Oxymorphone Hydrochloride 42 Pentazocine Lactate 43 Tapentadol 44 Tramadol Hydrochloride 45 Anesthetics 46 Local Anesthetics 47 Lidocaine Hydrochloride 48 Lidocaine and Prilocaine Anti-Addiction/ Substance Abuse Treatment Agents 49 50 Alcohol Deterrents/Anti-craving 51 Acamprosate Calcium 52 Disulfiram 53 Naltrexone Hydrochloride Nomenclature change; New Class Opioid Dependence Treatments -

2 Conjunctiva Lect
Dr Parul Ichhpujani Assistant Professor Deptt. Of Ophthalmology, Government Medical College and Hospital, Sector 32, Chandigarh Bacterial Chlamydial Viral Allergic Chemical/toxic or irritative Associated with systemic disease, Rickettsial, fungal, parasitic Etiology unknown Common, usually self‐limited, mostly children Direct contact or from nasal and sinus mucosa Conjunctival inflammation and purulent discharge PATHOGENS THAT CAUSE BACTERIAL CONJUNCTIVITIS Acute Hyperacute Chronic Staphylococcus Neisseria Staphylococcus aureus gonorrhoeae aureus Streptococcus Neisseria Moraxella lacunata pneumoniae meningitidis Haemophilus Enteric bacteria influenzae Gram (‐) diplococcus;Neisseria gonorrhoeae Adult: . Self contamination, . Acute onset with marked . Purulence, may progress to severe keratitis Children: . Ophthalmia neonatorum . 3‐5 days after parturition, . profuse purulent . discharge with swollen lids . Treatment: topical gentamicin Parenteral penicillin, 3rdcephalosporin CAUSES OF NEONATAL CONJUNCTIVITIS Causes Time of Onset (Postpartum) Chemical (silver nitrate) 1–36 hours Chlamydia 5–14 days Neisseria gonorrhoeae 24–48 hours Bacteria (Staphylococcus, 2–5 days Streptococcus, Haemophilus) Virus (herpes simplex virus 3–15 days types 1 and 2) Infection Treatment Chlamydia Oral erythromycin 50 mg/kg/day in four divided doses for 14 days Bacteria Gram‐positive Erythromycin 0.5% ointment four times a day Gram‐negative, gonococcal Penicillin G drops 10 000–20 000 units every hour and intravenous penicillin G drops 100 000 units/kg/day in four divided doses for 7 days Intravenous or intramuscular ceftriaxone 25–50 mg/kg/day once a day for 7 days Gram‐negative, others Gentamicin or tobramycin ointments Viral Trifluorothymidine drops every 2 hours for 7 days Staphylococcal blepharoconjunctivitis: Clinical signs include: . Diffuse conjunctival hyperemia with papillae or follicles, . Minimal mucopurulent discharge . Conjunctival thickening. -

National PBM Drug Monograph Epinastine (Elestat™) May 2004 VHA Pharmacy Benefits Management Strategic Healthcare Group and the Medical Advisory Panel
National PBM Drug Monograph Epinastine (Elestat™) May 2004 VHA Pharmacy Benefits Management Strategic Healthcare Group and the Medical Advisory Panel EXECUTIVE SUMMARY • Antihistamine ophthalmic drops provide quick relief from allergic conjunctivitis (AC) symptoms such as itching and redness, without the potential adverse effects associated with systemic absorption. • Epinastine is the fourth ophthalmic antihistamines/mast cell stabilizer approved for the itching associated with AC. Other ophthalmic preparations for allergic conjunctivitis include antihistamines, mast cell stabilizers, nonsteroidal anti-inflammatory agents (NSAIDs), corticosteroids, decongestants, and decongestant/antihistamines. • An ideal agent would offer improved efficacy and safety, reduce polypharmacy as a combination product or through replacing oral agents, and provide evidence for chronic AC prevention. INTRODUCTION1 The purposes of this monograph are to (1) evaluate the available evidence of safety, tolerability, efficacy, cost, and other pharmaceutical issues that would be relevant to evaluating epinastine ophthalmic solution for possible addition to the VA National Formulary (VANF); (2) define its role in therapy; and (3) identify parameters for its rational use in the VA. PHARMACOLOGY/PHARMACOKINETICS1, 2 Antihistamines are receptor antagonists used to avoid the inflammatory effects of histamine. Taken orally, these agents have been shown to be effective for treating allergic symptoms such as pruritis (itching). Epinastine in particular has been found to have a rapid onset of action.3 Topical antihistamine eye drops provide relief from ocular symptoms without systemic absorption or related adverse events, allowing for the combination of oral and topical agents when indicated. Ophthalmic antihistamine/mast cell stabilizers such as epinastine combine H1-receptor actions to block ocular itching and redness with H2-receptor affinity.