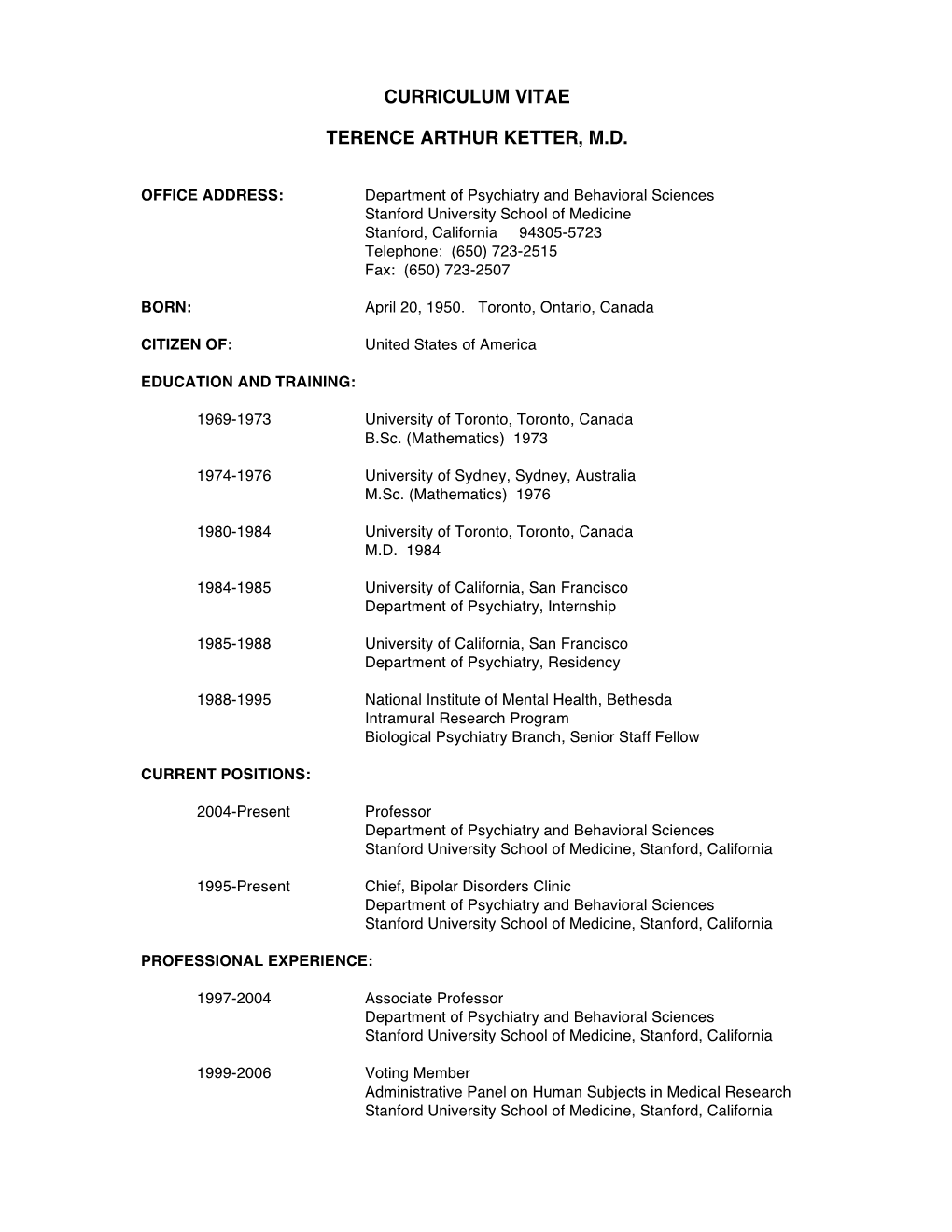
Curriculum Vitae Terence Arthur Ketter, M.D
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Olanzapine Versus Divalproex Sodium for the Treatment of Acute Mania and Maintenance of Remission: a 47-Week Study
Article Olanzapine Versus Divalproex Sodium for the Treatment of Acute Mania and Maintenance of Remission: A 47-Week Study Mauricio Tohen, M.D., Dr.P.H. Objective: Few double-blind trials have was significantly greater for the olanzapine compared longer-term efficacy and safety group. Median time to symptomatic ma- Terence A. Ketter, M.D. of medications for bipolar disorder. The nia remission was significantly shorter for authors report a 47-week comparison of olanzapine, 14 days, than for divalproex, olanzapine and divalproex. 62 days. There were no significant differ- Carlos A. Zarate, M.D. Method: This 47-week, randomized, ences between treatments in the rates of double-blind study compared flexibly symptomatic mania remission over the 47 Trisha Suppes, M.D., Ph.D. dosed olanzapine (5–20 mg/day) to dival- weeks (56.8% and 45.5%, respectively) and proex (500–2500 mg/day) for manic or subsequent relapse into mania or depres- Mark Frye, M.D. mixed episodes of bipolar disorder (N= sion (42.3% and 56.5%). Treatment-emer- 251). The only other psychoactive medi- gent adverse events occurring significantly Lori Altshuler, M.D. cation allowed was lorazepam for agita- more frequently during olanzapine treat- tion. The primary efficacy instrument was ment were somnolence, dry mouth, in- the Young Mania Rating Scale; a priori creased appetite, weight gain, akathisia, John Zajecka, M.D. protocol-defined threshold scores were and high alanine aminotransferase levels; ≥20 for inclusion, ≤12 for remission, and those for divalproex were nausea and ≥15 for relapse. Analytical techniques in- Leslie M. Schuh, Ph.D. -

Antipsychotic Agents and Bipolar Disorder
Tohen and Zarate Antipsychotic Agents and Bipolar Disorder Mauricio Tohen, M.D., Dr.P.H., and Carlos A. Zarate, Jr., M.D. Antipsychotic agents have been used commonly in the treatment of bipolar disorder. This article © Copyrightreviews the evolution 1998of the use ofPhysicians antipsychotic agents andPostgraduate their role in the acute and Press, maintenance Inc. treatment of bipolar disorder. The focus is on neuroleptic drugs, the atypical antipsychotic drugs (ris- peridone and clozapine), and two of the new atypical antipsychotic drugs that were recently approved. (J Clin Psychiatry 1998;59[suppl 1]:38–48) ntipsychotic drugs have been utilized for the man- clozapine) in the treatment of bipolar disorder,4 and the A agement of patients with bipolar disorder for sev- new atypical antipsychotic drugs that have been approved eral decades. A number of alternative somatic treatments recently. approaches have been reported for patients who do not re- spond well to or who are intolerant to lithium treatment.1,2 ANTIPSYCHOTICS IN BIPOLAR DISORDER Somatic treatments other than lithiumOne reported personal to have copy a may be printed role in the management of bipolar disorder include neuro- Prior to the lithium era, the pharmacologic strategies for leptics, anticonvulsant agents (carbamazepine, valproate, bipolar disorder primarily included neuroleptics and anti- lamotrigine, gabapentin), calcium channel blockers, anti- depressants. Antipsychotic agents have been used in the depressants, cholinergic agents, adrenergic blockers, thy- treatment of bipolar disorder for close to 40 years. The use roid hormones, phototherapy, and electroconvulsive ther- of the neuroleptic drug chlorpromazine to control agitated apy.1,2 Still, in spite of all these alternatives, a proportion states was introduced by Delay and Deniker in 1952.7 Neu- of patients with bipolar disorder continue to fail or roleptic drugs then were found to be quite instrumental in be intolerant to these agents. -

Direct-To-Consumer Ads Are Misleading: Concise Statements of Effectiveness Should Be Required
California Western School of Law CWSL Scholarly Commons Faculty Scholarship 2019 Direct-To-Consumer Ads are Misleading: Concise Statements of Effectiveness Should Be Required Robert A. Bohrer California Western School of Law, [email protected] Follow this and additional works at: https://scholarlycommons.law.cwsl.edu/fs Part of the First Amendment Commons, Food and Drug Law Commons, Health Law and Policy Commons, and the Pharmacy Administration, Policy and Regulation Commons Recommended Citation Robert A. Bohrer, Direct-To-Consumer Ads are Misleading: Concise Statements of Effectiveness Should Be Required, 22 J. Health Care L. & Pol'y 209 (2019). Available at: https://scholarlycommons.law.cwsl.edu/fs/330 This Article is brought to you for free and open access by CWSL Scholarly Commons. It has been accepted for inclusion in Faculty Scholarship by an authorized administrator of CWSL Scholarly Commons. For more information, please contact [email protected]. DIRECT-TO-CONSUMER ADS ARE MISLEADING: CONCISE STATEMENTS OF EFFECTIVENESS SHOULD BE REQUIRED ROBERT A. BOHRER, J.D., LL.M.* INTRODUCTION: THE PROBLEM WITH PHARMACEUTICAL ADVERTISING The issue of required disclaimers in direct-to-consumer (DTC) advertising of pharmaceuticals boiled to the surface in May 2019, when the Centers for Medicare and Medicaid Services (CMS) published a final rule requiring the disclosure of a drug's price in DTC ads.' The idea is not a new one-the American Medical Association (AMA) adopted a resolution recommending just such a required disclosure in June 2017.2 For a number of reasons, even if the proposal is implemented it may not have much effect.3 Consumers may see price as an indicator of effectiveness, just as a high-priced car is expected to be superior to a lower-priced car, and insurance coverage may reduce patients' C2019 Robert A. -

Commentary Cariprazine in Bipolar Disorders
Commentary See article by Calabrese et al Cariprazine in Bipolar Disorders Mauricio Tohen, MD, DrPH, MBA his issue of JCP includes a report on the efficacy and duration (3 weeks) and the minimum YMRS severity safety of cariprazine for the treatment of bipolar mania score (> 20), although a minimum severity score for the T 1 from Calabrese and colleagues. Montgomery-Asberg Depression Rating Scale total score < 18 may limit the generalizability of findings in patients Key Study Findings with mixed features. Exclusion criteria were similar to those The authors report a multicenter (N = 497), randomized, of previous clinical trials as well.6 double-blind, placebo-controlled study (NCT01058668). Yildiz et al7 recently published a network meta-analysis, Patients were randomly assigned to placebo, cariprazine 3–6 with a Bayesian framework, comparing 18 active treatments mg/d, or cariprazine 6–12 mg/d for 3 weeks. The primary against placebo including the current cariprazine study outcome was change from baseline to week 3 utilizing the (NCT01058668)1 from data available from meeting Young Mania Rating Scale (YMRS). Both cariprazine groups abstracts.8 Cariprazine appears to compare well with other were statistically significantly superior to placebo on the treatments, with an effect size of 0.62 and a number needed primary outcome, all 11 YMRS single items, and Clinical to treat (NNT) of 5 for response and 7 for remission. Yildiz Global Impressions-Severity of Illness scores. The most and colleagues’7 effect size estimations put cariprazine common (≥ 5% and twice the rate of placebo) treatment- toward the top: only topiramate, risperidone, and related adverse events for cariprazine were akathisia (both olanzapine had larger effect size estimations. -

Bipolar Depression
IndicationNew Join our expert faculty for this important National Broadcast, including a live Q&A session… Bipolar Depression Please see Important Safety Information, including Boxed Presentation, Diagnosis, and Treatment Warnings, below and accompanying full Prescribing This promotional, non-CME program is intended only for healthcare professionals Information. involved in the treatment of adult patients with bipolar disorder. Date: Location: FACULTY Thursday, August 15, 2013 Novita Wine Bar and Trattoria 860 Franklin Avenue Time: Joseph R. Calabrese, MD Garden City, NY 11530 Professor of Psychiatry 6:30 PM (516) 739-7660 Department of Psychiatry Case Western Reserve University School Meeting Code: of Medicine 19064 Director Mood Disorders Program Attendees will have the option to accept the Sunovion-provided food and beverage Department of Psychiatry service, opt out of all food and beverage, or purchase their own food and beverage. University Hospitals Case Medical Center Cleveland, OH Gary S. Sachs, MD Program Objectives: Founder • Address key challenges in the diagnosis and management of bipolar depression Collaborative Care Initiative Rules: Lincoln, MA • E xplore the broader impact of bipolar depression on patients Mauricio Tohen, MD 1-• WithinP resent the relevant codeline, data thefor LATUDA, prism mustnow indicated be shown for monotherapyin and adjunctive green, even on a dark background - Professor and Chairman therapy with either lithium or valproate for the treatment of patients with major Department of Psychiatry itdepressive cannot beepisodes shown associated in white. with bipolar I disorder (bipolar depression) University of New Mexico Albuquerque, NM 2-Please The seeprism Important should Safety be 40% Information, larger thanincluding the Boxed cap Warnings, below and accompanyingheight of the full letter Prescribing A. -

Treatment Guidelines in Bipolar Disorders and the Importance of Proper Clinical Trial Design Mauricio Tohen
Copyedited by: oup International Journal of Neuropsychopharmacology (2017) 20(2): 95–97 doi:10.1093/ijnp/pyx002 Editorial EDITORIAL Treatment Guidelines in Bipolar Disorders and the Importance of Proper Clinical Trial Design Mauricio Tohen Department of Psychiatry & Behavioral Sciences, University of New Mexico Health Sciences Center, Albuquerque, New Mexico. Correspondence: Mauricio Tohen, MD, DrPH, MBA, Department of Psychiatry & Behavioral Sciences, University of New Mexico Health Sciences Center, 2400 Tucker Ave, Albuquerque, NM 87131, USA ([email protected]). A working group led by Dr. Konstantinos Fountoulakis developed (http://clinicaltrials.gov and http://www.clinicalstudyresults. the first International College of Neuropsychopharmacology org) as well as web pages of pharmaceutical companies with (CINP) clinical guidelines for the treatment of Bipolar Disorders compounds used in bipolar disorder up to March 25, 2016. in adult patients. Their work is very thoroughly described in The authors provide a critical analysis of the existing treat- four separate papers (parts) included in this issue of the journal. ment grading methods that led them to determine that there The first article is Background and Methods of the Development was no optimal method to grade treatments for bipolar disorder, of Guidelines (Fountoulakis et al., 2017d); part 2 is Review, therefore creating their own grading system. Their methodology Grading of the Evidence, and a Precise Algorithm (Fountoulakis provides 32 different levels of recommendations, starting with et al., 2017c); part 3 is The Clinical Guidelines (Fountoulakis the optimal: “At least 1 positive 2 active arm RCT vs placebo et al., 2017a); and Part 4 is Unmet Needs in the Treatment of exists, plus positive 1 active arm RCTs, and no negative RCTs.” Bipolar Disorder and Recommendations for Future Research Lower level scenarios take into account posthoc reports, meta- (Fountoulakis et al., 2017b). -

Management of Acute Mania
Management of Acute Mania Management of Acute Mania Mauricio Tohen, M.D., Dr.P.H., and Starr Grundy, B.Sc.Pharm. Bipolar disorder is a lifelong episodic condition characterized by mood swings between mania and depression. In the United States alone, approximately 4 million people are affected by this disorder. © CopyrightPharmacologic treatment 2000 for acute Physicians manic episodes or as Postgraduatemaintenance therapy includes Press, lithium, val- Inc. proate, carbamazepine, and typical antipsychotics. However, many patients fail to respond to these treatments due to lack of efficacy or production of side effects leading to patient noncompliance. Non- compliance with pharmacologic treatment is indeed a major risk factor in bipolar disorder patients and needs to be managed with ongoing education, psychotherapy, and a simplified but effective pharma- cologic treatment regimen. Recently introduced novel antipsychotics show much promise as mood- stabilizing agents in bipolar patients, with minimal risk of treatment-emergent extrapyramidal symp- toms and tardive dyskinesia. Nonetheless, further research is warranted to help clarify the role of novel antipsychotics in the treatment of bipolar disorder. (J Clin Psychiatry 1999;60[suppl 5]:31–34) ipolar disorder is a highly prevalentOne personal condition copythat mayare bedifficult printed to estimate. However, in recent years an in- Bcauses a great deal of human suffering. First system- creasing number of patients have been hospitalized with atically described in the scientific literature in 1921,1 bi- affective disorders.5 This increase might be explained by polar disorder has an episodic nature, characterized by changes in diagnostic criteria. Another explanation is manic or depressive episodes followed by symptom-free treatment-orientated diagnostic bias, which occurs when periods. -

(CINP) Treatment Guidelines for Bipolar Disorder in Adults (CINP-BD-2017), Part 1: Background and Methods of the Development of Guidelines Konstantinos N
Copyedited by: oup International Journal of Neuropsychopharmacology (2017) 20(2): 95–97 doi:10.1093/ijnp/pyx002 Editorial EDITORIAL Treatment Guidelines in Bipolar Disorders and the Importance of Proper Clinical Trial Design Mauricio Tohen Department of Psychiatry & Behavioral Sciences, University of New Mexico Health Sciences Center, Albuquerque, New Mexico. Correspondence: Mauricio Tohen, MD, DrPH, MBA, Department of Psychiatry & Behavioral Sciences, University of New Mexico Health Sciences Center, 2400 Tucker Ave, Albuquerque, NM 87131, USA ([email protected]). A working group led by Dr. Konstantinos Fountoulakis developed (http://clinicaltrials.gov and http://www.clinicalstudyresults. the first International College of Neuropsychopharmacology org) as well as web pages of pharmaceutical companies with (CINP) clinical guidelines for the treatment of Bipolar Disorders compounds used in bipolar disorder up to March 25, 2016. in adult patients. Their work is very thoroughly described in The authors provide a critical analysis of the existing treat- four separate papers (parts) included in this issue of the journal. ment grading methods that led them to determine that there The first article is Background and Methods of the Development was no optimal method to grade treatments for bipolar disorder, of Guidelines (Fountoulakis et al., 2017d); part 2 is Review, therefore creating their own grading system. Their methodology Grading of the Evidence, and a Precise Algorithm (Fountoulakis provides 32 different levels of recommendations, starting with et al., 2017c); part 3 is The Clinical Guidelines (Fountoulakis the optimal: “At least 1 positive 2 active arm RCT vs placebo et al., 2017a); and Part 4 is Unmet Needs in the Treatment of exists, plus positive 1 active arm RCTs, and no negative RCTs.” Bipolar Disorder and Recommendations for Future Research Lower level scenarios take into account posthoc reports, meta- (Fountoulakis et al., 2017b). -

March 6-9, 2013 Grand Hyatt New York
103rd Annual Meeting of the American Psychopathological Association March 6-9, 2013 Grand Hyatt New York Jeanine Klein - Through the trees 2010 Long-term Outcomes in Psychopathology Research: Rethinking the Scientific Agenda 1 SPEAKERS Evelyn J. Bromet, PhD Kay Redfield Jamison, PhD Stony Brook University Johns Hopkins University School of Medicine Daniel N. Klein, PhD Anne Marie Albano, PhD Stony Brook University Columbia University John W. Finney, PhD Maria Kovacs, PhD VA Palo Alto Health Care System; University of Pittsburgh School of Medicine Stanford University Matthew K. Nock, PhD James J. Hudziak, MD Harvard University Vermont Center for Children, Youth and Families; University of Vermont Emil F. Coccaro, MD University of Chicago Peter Szatmari, MD, MSc University of Toronto James Kirkbride, PhD University of Cambridge Gabrielle A. Carlson, MD Stony Brook University Carlos N. Pato, MD, PhD University of Southern California Matthew J. Friedman, MD, PhD National Center for PTSD; Geisel School Yuval Neria, PhD of Medicine at Dartmouth Columbia University Kenneth S. Kendler, MD CHAIRS & DISCUSSANTS Virginia Commonwealth University Ramin Mojtabai, MD, PhD, MPH Johns Hopkins University Patrick McGorry, MD, PhD University of Melbourne; Orygen Youth Stephen L. Buka, ScD Health Brown University Zahava Solomon, PhD Roman Kotov, PhD Tel Aviv University Stony Brook University Mauricio Tohen, MD, DrPH, MBA Robert B. Zipursky, MD University of New Mexico McMaster University Karestan C. Koenen, PhD Lisa Dixon, MD, MPH Columbia University Columbia University Fred Frese, PhD Benedetto Vitiello, MD Northeast Ohio Medical University; Case National Institute of Mental Health Western Reserve University; Summit County (Ohio) Recovery Project Kathleen R. Merikangas, PhD National Institute of Mental Health 2 OFFICERS Evelyn J. -

Stigma and Functioning in Patients with Bipolar Disorder
Journal of Affective Disorders 130 (2011) 323–327 Contents lists available at ScienceDirect Journal of Affective Disorders journal homepage: www.elsevier.com/locate/jad Preliminary communication Stigma and functioning in patients with bipolar disorder G.H. Vázquez a,⁎, F. Kapczinski b, P.V. Magalhaes b, R. Córdoba c, C. Lopez Jaramillo d, A.R. Rosa e, M. Sanchez de Carmona f, M. Tohen g and The Ibero-American Network on Bipolar Disorders (IAN-BD) group a Department of Neuroscience, University of Palermo, Buenos Aires, Argentina b Bipolar Disorders Program & INCT Translational Medicine, Hospital de Clínicas de Porto Alegre, Universidade Federal do Rio Grande do Sul, Porto Alegre, Brazil c Chief postgrade mental health and psychiatric, Universidad del Rosario, General Director Grupo Cisne., Bogotá, Colombia d Director Mood Disorder Program HUSVP, Coordinator Research Group in Psychiatry, School of Medicine, University of Antioquia, Medellin, Colombia e Bipolar Disorders Program, Clinical Institute of Neuroscience, Hospital Clinic of Barcelona, Barcelona, Spain f ISBD Mexican Chapter, Mexico D.F., Mexico g University of Texas Health Science Center at San Antonio, USA article info abstract Article history: Objective: The aim of this study was to investigate the impact of self-rated stigma and Received 20 August 2010 functioning in patients with bipolar disorder in Latin-America. Accepted 10 October 2010 Methods: Two-hundred and forty-one participants with bipolar disorder were recruited from Available online 5 November 2010 three Latin American countries (Argentina, Brazil, and Colombia). Functional impairment was assessed with the Functioning Assessment Short Test (FAST) and experiences with and impact Keywords: of perceived stigma was evaluated using the Inventory of Stigmatizing Experiences (ISE). -

The CINP Guidelines on the Definition and Evidence-Based Interventions for Treatment-Resistant Bipolar Disorder Konstantinos N
applyparastyle "fig//caption/p[1]" parastyle "FigCapt" applyparastyle "fig" parastyle "Figure" International Journal of Neuropsychopharmacology (2020) 23(4): 230–256 doi:10.1093/ijnp/pyz064 Advance Access Publication: 5 December 2019 Review Review The CINP Guidelines on the Definition and Evidence-Based Interventions for Treatment-Resistant Bipolar Disorder Konstantinos N. Fountoulakis, Lakshmi N. Yatham, Heinz Grunze, Eduard Vieta, Allan H. Young, Pierre Blier, Mauricio Tohen, Siegfried Kasper, Hans Jurgen Moeller 3rd Department of Psychiatry, School of Medicine, Aristotle University of Thessaloniki, Thessaloniki, Greece (Dr Fountoulakis); Department of Psychiatry, University of British Columbia, Mood Disorders Centre of Excellence, Djavad Mowafaghian Centre for Brain Health, Vancouver, Canada (Dr Yatham); Psychiatrie Schwäbisch Hall & Paracelsus Medical University, Nuremberg, Germany (Dr Grunze); Hospital Clinic, Institute of Neuroscience, University of Barcelona, IDIBAPS, CIBERSAM, Barcelona, Catalonia, Spain (Dr Vieta); Centre for Affective Disorders, Institute of Psychiatry, Psychology and Neuroscience, King’s College, London, UK (Dr Young); The Royal Institute of Mental Health Research, Department of Psychiatry, University of Ottawa, Ottawa, Canada (Dr Blier); Department of Psychiatry and Behavioral Sciences, University of New Mexico Health Sciences Center, Albuquerque, NM (Dr Tohen); Department of Psychiatry and Psychotherapy, Medical University Vienna, MUV, AKH, Vienna and Center for Brain Research, Medical University Vienna, MUV, -

A Prospective Open-Label Treatment Trial of Olanzapine Monotherapy in Children and Adolescents with Bipolar Disorder
University of Massachusetts Medical School eScholarship@UMMS Psychiatry Publications and Presentations Psychiatry 2001-10-20 A prospective open-label treatment trial of olanzapine monotherapy in children and adolescents with bipolar disorder Jean A. Frazier University of Massachusetts Medical School Et al. Let us know how access to this document benefits ou.y Follow this and additional works at: https://escholarship.umassmed.edu/psych_pp Part of the Psychiatry Commons Repository Citation Frazier JA, Biederman J, Tohen MF, Feldman PD, Jacobs TG, Toma V, Rater MA, Tarazi RA, Kim GS, Garfield SB, Sohma M, Gonzalez-Heydrich J, Risser RC, Nowlin ZM. (2001). A prospective open-label treatment trial of olanzapine monotherapy in children and adolescents with bipolar disorder. Psychiatry Publications and Presentations. https://doi.org/10.1089/10445460152595568. Retrieved from https://escholarship.umassmed.edu/psych_pp/385 This material is brought to you by eScholarship@UMMS. It has been accepted for inclusion in Psychiatry Publications and Presentations by an authorized administrator of eScholarship@UMMS. For more information, please contact [email protected]. JOURNAL OF CHILD AND ADOLESCENT PSYCHOPHARMACOLOGY Volume 11, Number 3, 2001 Mary Ann Liebert, Inc. Pp. 239–250 A Prospective Open-Label Treatment Trial of Olanzapine Monotherapy in Children and Adolescents with Bipolar Disorder JEAN A. FRAZIER, M.D., 1–3 JOSEPH BIEDERMAN, M.D., 1–3 MAURICIO TOHEN, M.D., DrPH, 1,2,4 PETER D. FELDMAN, Ph.D., 4 THOMAS G. JACOBS, M.A.S., 4 VERNA TOMA, B.Sc., 4 MICHAEL A. RATER, M.D., 1,3 REEM A. TARAZI, B.A., 1,3 GRACE S. KIM, M.A.R., B.A., 1,3 STACEY B.