Tomonli U Tua Haki Na
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Use of Electroanalgesia and Laser Therapies As Alternatives to Opioids for Acute and Chronic Pain Management[Version 1; Peer
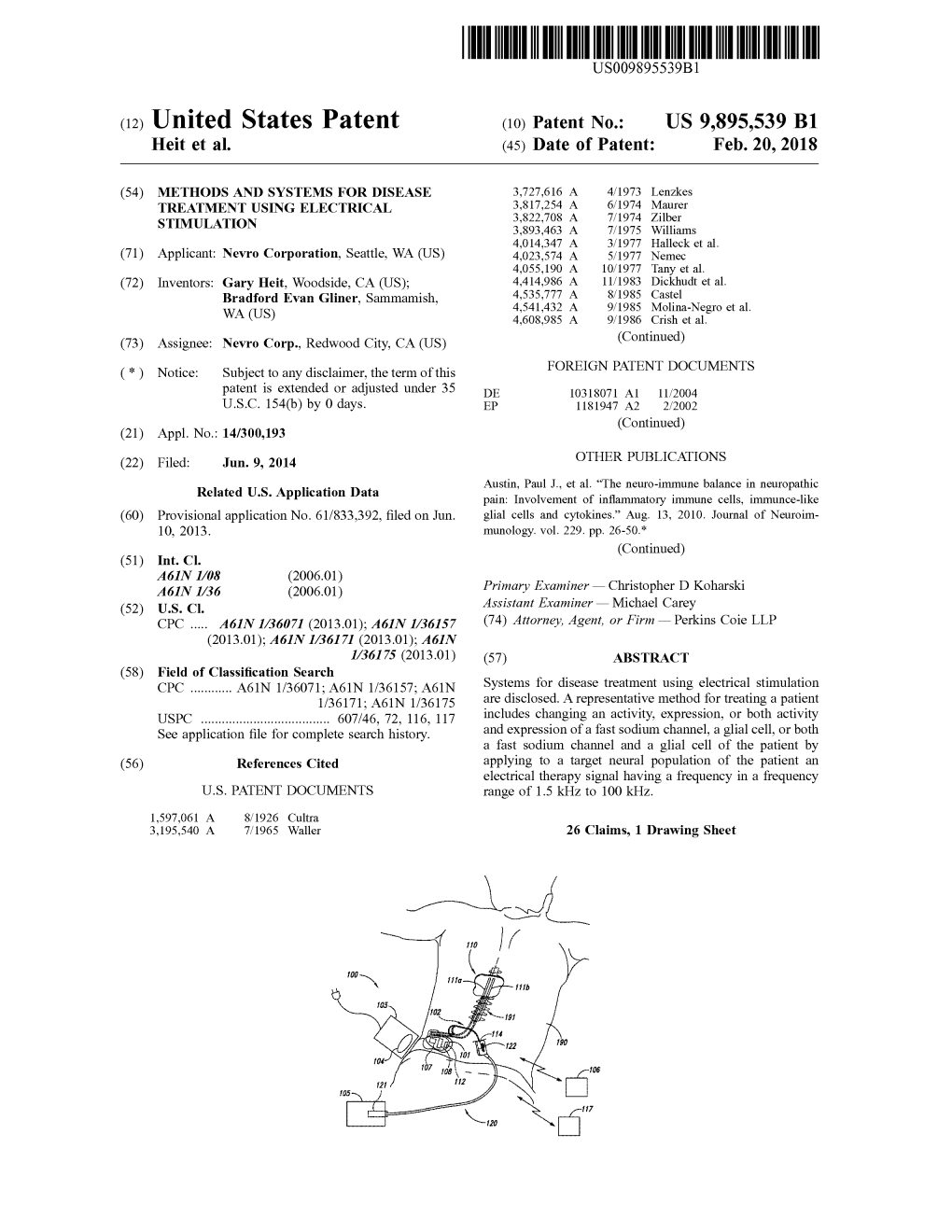
F1000Research 2017, 6(F1000 Faculty Rev):2161 Last updated: 04 AUG 2020 REVIEW Use of electroanalgesia and laser therapies as alternatives to opioids for acute and chronic pain management [version 1; peer review: 2 approved] Paul F. White1-3, Ofelia Loani Elvir-Lazo 3, Lidia Galeas4, Xuezhao Cao3,5 1P.O. Box 548, Gualala, CA 95445, USA 2The White Mountain Institute, The Sea Ranch, CA, USA 3Department of Anesthesiology, Cedars-Sinai Medical Center, 8700 Beverly Boulevard, Los Angeles, CA 95445, USA 4Orlando Family Medicine, Orlando, FL, USA 5First Hospital of China Medical University, Shenyang, China v1 First published: 21 Dec 2017, 6(F1000 Faculty Rev):2161 Open Peer Review https://doi.org/10.12688/f1000research.12324.1 Latest published: 21 Dec 2017, 6(F1000 Faculty Rev):2161 https://doi.org/10.12688/f1000research.12324.1 Reviewer Status Abstract Invited Reviewers The use of opioid analgesics for postoperative pain management has contributed to the global opioid epidemic. It was recently reported 1 2 that prescription opioid analgesic use often continued after major joint replacement surgery even though patients were no longer version 1 experiencing joint pain. The use of epidural local analgesia for 21 Dec 2017 perioperative pain management was not found to be protective against persistent opioid use in a large cohort of opioid-naïve patients Faculty Reviews are review articles written by the undergoing abdominal surgery. In a retrospective study involving prestigious Members of Faculty Opinions. The over 390,000 outpatients more than 66 years of age who underwent articles are commissioned and peer reviewed minor ambulatory surgery procedures, patients receiving a prescription opioid analgesic within 7 days of discharge were 44% before publication to ensure that the final, more likely to continue using opioids 1 year after surgery. -

VHA/Dod CLINICAL PRACTICE GUIDELINE for the MANAGEMENT of POSTOPERATIVE PAIN
VHA/DoD CLINICAL PRACTICE GUIDELINE FOR THE MANAGEMENT OF POSTOPERATIVE PAIN Veterans Health Administration Department of Defense Prepared by: THE MANAGEMENT OF POSTOPERATIVE PAIN Working Group with support from: The Office of Performance and Quality, VHA, Washington, DC & Quality Management Directorate, United States Army MEDCOM VERSION 1.2 JULY 2001/ UPDATE MAY 2002 VHA/DOD CLINICAL PRACTICE GUIDELINE FOR THE MANAGEMENT OF POSTOPERATIVE PAIN TABLE OF CONTENTS Version 1.2 Version 1.2 VHA/DoD Clinical Practice Guideline for the Management of Postoperative Pain TABLE OF CONTENTS INTRODUCTION A. ALGORITHM & ANNOTATIONS • Preoperative Pain Management.....................................................................................................1 • Postoperative Pain Management ...................................................................................................2 B. PAIN ASSESSMENT C. SITE-SPECIFIC PAIN MANAGEMENT • Summary Table: Site-Specific Pain Management Interventions ................................................1 • Head and Neck Surgery..................................................................................................................3 - Ophthalmic Surgery - Craniotomies Surgery - Radical Neck Surgery - Oral-maxillofacial • Thorax (Non-cardiac) Surgery.......................................................................................................9 - Thoracotomy - Mastectomy - Thoracoscopy • Thorax (Cardiac) Surgery............................................................................................................16 -

Acutepain Evdoc 5.20
Treating acute pain without overusing opioids Evidence-based pain management approaches Principal Consultants: Brian Bateman M.D., M.Sc. and Julie Lauffenburger, PharmD, Ph.D. Series Editors: Jerry Avorn, M.D. (principal editor), Jing Luo, M.D., M.P.H., Michael Fischer, M.D., M.S., Ellen Dancel, PharmD, M.P.H. Medical Writers: Jenny Cai, Stephen Braun Alosa Health is a nonprofit organization which is not affiliated with any pharmaceutical company. None of the authors accepts any personal compensation from any pharmaceutical manufacturer. These are general recommendations only; specific clinical decisions should be made by the treating clinician based on an individual patient’s clinical condition. © 2019 Alosa Health. All rights reserved. For more information, see AlosaHealth.org. ii | Treating acute pain without overusing opioids Alosa Health Treating acute pain without overusing opioids Accreditation: This activity has been planned and implemented in accordance with the accreditation requirements and policies of the Accreditation Council for Continuing Medical Education through the joint providership of Harvard Medical School and Alosa Health. The Harvard Medical School is accredited by the ACCME to provide continuing medical education for physicians. Credit Designation: The Harvard Medical School designates this enduring material for a maximum of 1.25 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity. Activity Overview: The primary goal of this educational program is to address the need for safe, effective pain relief among older adults across a range of settings. Achieving functional goals while avoiding harm from side effects, addiction, or potential overdose is challenging in this patient population due to such issues as altered pharmacodynamics/pharmacokinetics with age; polypharmacy; potential cognitive deficits; and heightened risk of falls and organ-specific vulnerabilities. -
Pain Monograph 5/5/06 2:42 PM Page 59
Pain Monograph 5/5/06 2:42 PM Page 59 Section IV: Management of Acute Pain and Chronic Noncancer Pain Pain Monograph 5/5/06 2:42 PM Page 61 Section IV: Management of Acute Pain and Chronic Noncancer Pain A . A C U T E P A I N Table 32. Examples of This section reviews the general approach to the treatment of acute pain, including treatment Multimodal Therapy goals, therapeutic strategies, and elements of pain management. It also provides an overview Combination of Agents Example (i.e., summary tables) of the treatment of some Systemic NSAIDa plus PO Ibuprofen plus PO common types of acute pain. systemic opioid hydromorphone Systemic NSAID plus IV ketorolac plus epidural epidural opioid and local fentanyl and bupivacaine anesthetic Systemic NSAID plus local IV ketorolac plus lidocaine infiltration of anesthetic plus infiltration of surgical site systemic opioid plus IV PCA morphine Regional block plus systemic Intraoperative anesthetic 1. Treatment Goals NSAID plus epidural opioid plus IV ketorolac plus As addressed in Section I.C.1, acute pain is a and local anesthetic postoperative fentanyl and bupivacaine epidural complex multidimensional experience that usu- Source: Reference 6. ally occurs in response to tissue trauma. Whereas aNSAIDs need to be used with care in surgical patients due to responses to acute pain may be adaptive, they the risk of bleeding (“anti-platelet” effect). can have adverse physiologic and psychological IV: intravenous; NSAID: nonsteroidal anti-inflammatory drugs; consequences (e.g., reduced tidal volume, exces- PCA: patient-controlled analgesia; PO: per os (oral). sive stress response, progression to chronic pain, inability to comply with rehabilitation, patient suffering and dissatisfaction). -
Guidelines for Prescribing Controlled Substances for Pain
GUIDELINES FOR PRESCRIBI NG CONTROLLED SUBSTANCE S FOR PAIN MEDICAL BOARD OF CALIFORNIA NOVEMBER 2014 Edmund G. Brown Jr., Governor David Serrano Sewell, J.D., President, Medical Board of California Kimberly Kirchmeyer, Executive Director, Medical Board of California Guidelines for Prescribing Controlled Substances for Pain Table of Contents PREAMBLE ..................................................................................................................... 1 UNDERSTANDING PAIN ................................................................................................ 2 Pain ............................................................................................................................. 2 Acute and Chronic Pain ............................................................................................... 3 Nociceptive and Neuropathic Pain ............................................................................... 3 Cancer and Non-Cancer Pain ...................................................................................... 3 Tolerance, Dependence and Addiction ........................................................................ 4 Pain as an Illness......................................................................................................... 4 SPECIAL PATIENT POPULATIONS............................................................................... 4 Acute Pain ................................................................................................................... 4 Emergency -

Electroanalgesia: Historical and Contelllporary Developlllents
Electroanalgesia: Historical and Contelllporary Developlllents PhD Thesis (VoluDle II) 1998 Joseph Gordon Gadsby BA(Hons) RGN RMN DipN(Lond) MISBM DHP DHS Department of Biological Sciences School of Applied Sciences De Montfort University Leicester Electroanalgesia: Historical and Conte:mporary Developntents A Thesis in Partial Fulfilntent of the Degree of Doctor of Philosophy Volume II Sections 7-8 Summary of Thesis Contents Title: Electroanalgesia: Historical and Contemporary Development Abstract: Acknowledgements: Contents list: Glossary: 1. Summary 2. Introduction 3. Historical and Experimental Studies 3.1 Introduction to the first stage of the study programme: historical developments in electro analgesia, mechanisms of electroanalgesia and clinical research 3.2 Early developments in electro analgesia 3.3 The Rev. John Wesley MA (1703-1791) Pioneer Electrotherapist: A History of Medicine Study 3.4 Mechanisms of pain 3.5 Mechanisms of electrical pain relief 3.6 Clinical Research - A randomised controlled trial of electroanalgesia in palliative medicine using acupuncture-like transcutaneous electrical nerve stimulation: A pilot study 3.7 Conclusions and recommendations 4.Tertiary Research: Systematic reviews and meta-analysis: 4.1 Introduction to the second stage of the study programme: systematic reviews and meta-analysis 4.2 Systematic reviews, meta-analysis and the Cochrane Collaboration 4.3 Developing a protocol for a Cochrane systematic review 4.4 Developing a Cochrane systematic review and meta-analysis 4.5 The effectiveness of Transcutaneous Electrical Nerve Stimulation (TENS) for chronic low back pain - A Cochrane Library Review 4.6 Improving and updating systematic reviews using the Cochrane Collaboration comments and criticisms mechanism 4.7 Conclusions and recommendations 5. -

Pain: Current Understanding of Assessment, Management, and Treatments
Pain: Current Understanding of Assessment, Management, and Treatments NATIONAL PHARMACEUTICAL COUNCIL, INC This monograph was developed by NPC as part of a collaborative project with JCAHO. December 2001 DISCLAIMER: This monograph was developed by the National Pharmaceutical Council (NPC) for which it is solely responsible. Another monograph relat- ed to measuring and improving performance in pain management was developed by the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) for which it is solely responsible. The two monographs were produced under a collaborative project between NPC and JCAHO and are jointly dis- tributed. The goal of the collaborative project is to improve the quality of pain management in health care organizations. This monograph is designed for informational purposes only and is not intended as a substitute for medical or professional advice. Readers are urged to consult a qualified health care professional before making decisions on any specific matter, particularly if it involves clinical practice. The inclusion of any reference in this monograph should not be construed as an endorsement of any of the treatments, programs or other information discussed therein. NPC has worked to ensure that this monograph contains useful information, but this monograph is not intended as a comprehensive source of all relevant information. In addi- tion, because the information contain herein is derived from many sources, NPC cannot guarantee that the information is completely accurate or error free. NPC is not responsible for any claims or losses arising from the use of, or from any errors or omissions in, this monograph. Editorial Advisory Board Patricia H. Berry, PhD, APRN, BC, CHPN Jeffrey A. -

Control of Pain in Adults with Cancer 106 a National Clinical Guideline
SIGN Scottish Intercollegiate Guidelines Network Control of pain in adults with cancer 106 A national clinical guideline November 2008 KEY TO EVIDENCE STATEMENTS AND GRADES OF RECOMMENDATIONS LEVELS OF EVIDENCE 1++ High quality meta-analyses, systematic reviews of RCTs, or RCTs with a very low risk of bias 1+ Well conducted meta-analyses, systematic reviews, or RCTs with a low risk of bias 1 - Meta-analyses, systematic reviews, or RCTs with a high risk of bias 2++ High quality systematic reviews of case control or cohort studies High quality case control or cohort studies with a very low risk of confounding or bias and a high probability that the relationship is causal 2+ Well conducted case control or cohort studies with a low risk of confounding or bias and a moderate probability that the relationship is causal 2 - Case control or cohort studies with a high risk of confounding or bias and a significant risk that the relationship is not causal 3 Non-analytic studies, eg case reports, case series 4 Expert opinion GRADES OF RECOMMENDATION Note: The grade of recommendation relates to the strength of the evidence on which the recommendation is based. It does not reflect the clinical importance of the recommendation. A At least one meta-analysis, systematic review, or RCT rated as 1++, and directly applicable to the target population; or A body of evidence consisting principally of studies rated as 1+, directly applicable to the target population, and demonstrating overall consistency of results B A body of evidence including studies rated -

Practice Guidelines for Acute Pain Management in the Perioperative Setting: Bibliography American Society of Anesthesiologists
Practice Guidelines for Acute Pain Management in the Perioperative Setting: Bibliography American Society of Anesthesiologists 1. Abboud T.K., Dror A., Mosaad P., Zhu J., Mantilla M., Swart F.,Gangolly J., Silao P., Makar A., Moore J., Davis H, Lee J: Mini-dose intrathecal morphine for the relief of post-cesarean section pain: Safety, efficacy, and ventilatory responses to carbon dioxide. Anesth Analg 67:137-143, 1988 2. Aguilar JL, Montero A, Lopez FV, Llamazares JF: Bilateral interpleural injection of local anesthetics. Reg Anesth 14, 93-94, 1989 3. Ahn H., Bronge A., Johansson K., Ygge H., Lindhagen J: Effect of continuous postoperative epidural analgesia on intestinal motility. Br J Surg 75:1176-1178, 1988. 4. Ali J, Yaffe CS, Serrette C: The effect of transcutaneous electric nerve stimulation on postoperative pain and pulmonary function. Surgery 89:507-512, 1981 5. Allen PD, Walman T, Concepcion M, Sheskey M, Patterson MK, Cullen D, Covino BG: Epidural morphine provides postoperative pain relief in peripheral vascular and orthopedic surgical patients: A dose-response study. Anesth Analg 65:165-170, 1986 6. Amaranath L, Andrish JT, Gurd AR, Weiker GG, Yoon H: Efficacy of intermittent epidural morphine following posterior spinal fusion in children and adolescents. Clin Orthopaed Rel Res 249:223-226, 1989 7. Anand KJS, Sippell Wg, Aynsley-Green A: Randomized trial of fentanyl anaesthesia in preterm babies undergoing surgery. Lancet, 1, 243-247, 1987 8. Ananthanarayan C, Kashtan H: Pneumothorax after interpleural block in a spontaneously breathing patient. Anesthesia, 45:392, 1990 9. Arvidsson I, Eriksson E, Knutsson E, Arner S: Reduction of pain inhibition on voluntary muscle activation by epidural analgesia. -
Transcranial Electrical Stimulation Research Articles, Abstracts, and Reports TABLE of CONTENTS
Transcranial Electrical Stimulation Research Articles, Abstracts, and Reports TABLE OF CONTENTS PREFACE: ................................................................................................................................................................... 5 NEXALIN TRANSCRANIAL ELECTRICAL STIMULATION ............................................................................................... 5 SECTION 1: THE EVOLUTION AND DEVELOPMENT OF THE NEXALIN TECHNOLOGY ................................................ 6 TRANSCRANIAL ELECTRIC STIMULATION: ANALGESIA AND ALLIED EFFECTS ............................................................ 7 ANESTHESIA IN LABORATORY ANIMALS ACHIEVED WITH THE COMBINED EFFECTS OF DIRECT AND IMPULSE CURRENTS ............................................................................................................................................................... 11 TRANSCRANIAL ELECTROANALGESIA IN THE TREATMENT OF SPONDYLOGENOUS PAIN SYNDROMES .................. 27 ARRESTING OF PAIN SYNDROME AND AUTONOMIC RESPONSES DURING PNEUMOENCEPHALOGRAPHY WITH THE USE OF TRANSCRANIAL ELECTROANALGESIA .......................................................................................................... 32 TRANSCRANIAL ELECTROSTIMULATION OF THE BRAIN OPIOID STRUCTURE IN THE TREATMENT OF ULCERATIVE DISEASE OF THE STOMACH AND THE DUODENUM ................................................................................................. 35 METABOLISM OF BIOGENIC AMINES DURING THE TREATMENT OF ALCOHOL WITHDRAWAL -

Electroanalgesia for the Postoperative Control Pain in Dogs Eletroanalgesia Para O Controle Da Dor Pós-Operatória Em Cães
8 - ORIGINAL ARTICLE ANESTHESIA Electroanalgesia for the postoperative control pain in dogs Eletroanalgesia para o controle da dor pós-operatória em cães Renata Navarro CassuI, Daniele Alves da SilvaII, Túlio Genari FilhoII, Helaine StevaninIII IPhD, Full Professor, Department of Veterinary Surgery and Anestesiology, Scholl of Veterinary Medicine, Unoeste, Presidente Prudente-SP, Brazil. Mentor. Responsible for intelectual, scientific content, statistical analysis of the study and critical revision. IIGraduate student, Faculty of Veterinary Medicine, Unoeste, Presidente Prudente-SP, Brazil. Helped with technical procedures, collection and processing of study informations. IIIFull Professor, Department of Veterinary Surgery and Anestesiology, Scholl of Veterinary Medicine, Unoeste, Presidente Prudente-SP, Brazil. Responsible for surgical procedure. ABSTRACT PURPOSE: To evaluate the analgesic and neuroendocrine effects of electroanalgesia in dogs undergoing ovariohysterectomy. METHODS: Eighteen dogs were randomly distributed to three groups of six animals each and received either electrical stimuli at acupuncture points (EA), at peri-incisional dermatomes (DER) and at both acupuncture points and peri-incisional dermatomes (EAD). Pre-anesthetic medication was acepromazine (0.05mg kg-1, IV). Anesthesia was induced with propofol (4 to 5mg kg-1, IV) and maintained with isoflurane. Postoperatively pain degree was measured using a numerical rating scale. Dogs were scored at 1, 3, 6, 12 and 24 hours postoperative. If the pain score was ≥6, supplemental morphine (0.5mg kg-1, IM) was administered. Serum cortisol concentration was measured before pre-anesthetic medication (basal), and at 1, 12 and 24 hours postoperative. RESULTS: EA and EAD- treated dogs had lower pain scores than DER treated dogs one hour postoperatively. Fewer EA and EAD- treated dogs required rescue analgesia. -

ELECTRICAL NERVE STIMULATION for the TREATMENT of PAIN Provided By
WA Health Technology Assessment - HTA HEALTH TECHNOLOGY ASSESSMENT UPDATED HTA FINAL REPORT ELECTRICAL NERVE STIMULATION FOR THE TREATMENT OF PAIN UPDATED DATE: FRIDAY, NOVEMBER 13, 2009 Health Technology Assessment Program 676 Woodland Square Loop SE P.O. Box 42712 Olympia, WA 98504-2712 http://www.hta.hca.wa.gov Updated FINAL: ENS: 11-13-09 1 of 104 WA Health Technology Assessment - HTA ELECTRICAL NERVE STIMULATION FOR THE TREATMENT OF PAIN Provided by: Spectrum Research, Inc. Prepared by: Jocelyn M. Weiss, PhD, MPH Andrea C. Skelly, PhD, MPH Nora Henrikson, PhD, MPH Lisa Kercher, PhD, MPH Joseph R. Dettori, PhD, MPH With assistance from: Erika D. Ecker, BS This technology assessment report is based on research conducted by a contracted technology assessment center, with updates as contracted by the Washington State Health Care Authority. This report is an independent assessment of the technology question(s) described based on accepted methodological principles. The findings and conclusions contained herein are those of the investigators and authors who are responsible for the content. These findings and conclusions may not necessarily represent the views of the HCA/Agency and thus, no statement in this report shall be construed as an official position or policy of the HCA/Agency. The information in this assessment is intended to assist health care decision makers, clinicians, patients and policy makers in making sound evidence-based decisions that may improve the quality and cost- effectiveness of health care services. Information in this report is not a substitute for sound clinical judgment. Those making decisions regarding the provision of health care services should consider this report in a manner similar to any other medical reference, integrating the information with all other pertinent information to make decisions within the context of individual patient circumstances and resource availability.