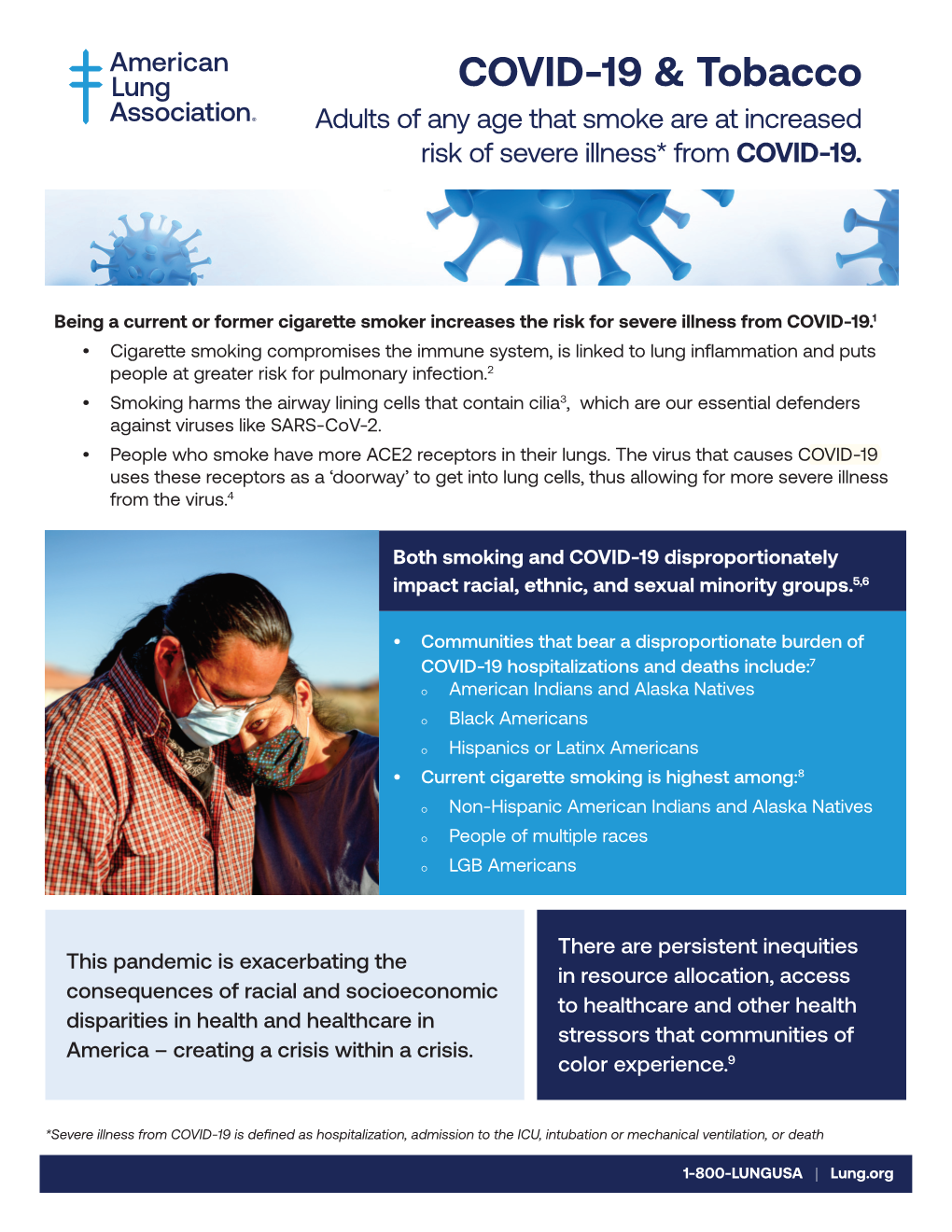
COVID-19 & Tobacco
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ethnic Smoking Fact Sheet -- Mtf Updated Version
TOBACCO USE AND HISPANICS Despite reductions in smoking prevalence achieved since the first Surgeon General’s report on the consequences of smoking in 1964, smoking remains the leading cause of preventable death in the United States.1 Smoking accounts for more than 480,000 deaths in the United States each year, and is a major risk factor for the four leading causes of death: heart disease, cancer, chronic obstructive pulmonary disease, and stroke.2 Tobacco Use Among Hispanic Adults According the 2019 National Health Interview Survey (NHIS) of adults ages 18 and over, 8.8 percent of Hispanic adults in the United States are current smokers, compared to 15.5 percent of Whites, 14.9 percent of African, Americans, 20.9 percent of American Indian/Alaska Natives, and 7.2 percent of Asian Americans. Overall, 14.0 percent of U.S. adults are current smokers.3 Current smoking prevalence among Hispanics reflects nearly 46 percent decrease from 2005, when the rate was 16.2 percent. Hispanic smokers also tend to consume fewer cigarettes per day than non-Hispanic white smokers and are less likely to be daily smokers than smokers of all other racial/ethnic groups. 4 However, research also shows that—as with other immigrant groups—smoking behavior trends toward that of non-Hispanic whites as Hispanics acculturate to the United States, particularly for female Hispanics.5 While Hispanic smoking rates are low overall, differences exist within Hispanic subpopulations that are masked when surveys group Hispanics as a single population. For example, according to combined NHIS data from 2009-2013, 21.6 percent of Puerto Ricans, 18.2 percent of Cubans, 13 percent of Mexicans, and 9.2 percent of Central or South Americans are current smokers (the overall smoking prevalence for Hispanics during this time period was 13.5%).6 In addition, smoking rates are significantly higher for U.S.-born Hispanics than for foreign- born Hispanics in the U.S. -

CIGARETTE SMUGGLING Wednesday, 22 January 2014 9:00 - 12:30 Altiero Spinelli Building, Room ASP 5G3
DIRECTORATE GENERAL FOR INTERNAL POLICIES POLICY DEPARTMENT D: BUDGETARY AFFAIRS WORKSHOP ON CIGARETTE SMUGGLING Wednesday, 22 January 2014 9:00 - 12:30 Altiero Spinelli Building, Room ASP 5G3 PE490.681 18/01/2014 EN TABLE OF CONTENTS WORKSHOP PROGRAMME 5 EU POLICY AND ILLICIT TOBACCO TRADE: ASSESSING THE IMPACTS 7 Briefing Paper by Luk Joossens, Hana Ross and Michał Stokłosa EU AGREEMENTS WITH FOUR CIGARETTE MANUFACTURERS - MAIN 56 FACTS Table by Policy Department D ANNEX I: BIOGRAPHIES OF INVITED SPEAKERS 57 ANNEX II: PRESENTATIONS 66 Presentation by Leszek Bartłomiejczyk Presentation by Luk Joossens, Hana Ross and Michał Stokłosa 3 WORKSHOP ON CCIGARETTE SSMUGGLING Organised by the Policy Department D on Budgetary Affairs Wednesday, 22 January 2014, 9:00 - 12:30 European Parliament, Brussels Altiero Spinelli Building, Room ASP 5G3 DRAFT WORKSHOP PROGRAMME 9:00 - 9:10 Welcome and Introduction 9:00 - 9:05 Welcome by Michael Theurer 5 minutes Chair of the Committee on Budgetary Control 9:05 - 9:10 Introduction by Bart Staes 5 minutes Vice-Chair of the Committee on Budgetary Control ___________________________________________________________ 9:10 - 9:25 First speaker: Prof. Anna Gilmore (UK) Director, Tobacco Control Research Group (University of Bath) - evaluate impact of public health policy and the impact of broader policy changes. Part of UK Centre for Tobacco Control Studies (UKCTCS): The Current State of Smuggling of Cigarettes Followed by Q&A (15min) 9:40 - 9.55 Second speaker: Aamir Latif The International Consortium of Investigative Journalists (ICIJ): Terrorism and Tobacco: Extremists, Insurgents Turn to Cigarette Smuggling Followed by Q&A (15min) Programme version dated 26 November 2013, updated 09/01/2014 DV/1014866EN PE490.681v01-00 5 10:10 - 10:25 Third speaker: Howard Pugh (EUROPOL) Project Manager AWF Smoke: How Does EUROPOL Contribute to the Fight Against Global Cigarette Smuggling? Followed by Q&A (15min) 10:40 - 10:55: Fourth speaker: Leszek Bartłomiejczyk Warsaw School of Economics, expert in excise duties and border control, team of Prof. -

Cigarettes and Tobacco Products Removed from the California Tobacco Directory by Brand
Cigarettes and Tobacco Products Removed From The California Tobacco Directory by Brand Brand Manufacturer Date Comments Removed #117 - RYO National Tobacco Company 10/21/2011 5/6/05 Man. Change from RBJ to National Tobacco Company 10/20's (ten-twenty's) M/s Dhanraj International 2/6/2012 2/2/05 Man. Name change from Dhanraj Imports, Inc. 10/20's (ten-twenty's) - RYO M/s Dhanraj International 2/6/2012 1st Choice R.J. Reynolds Tobacco Company 5/3/2010 Removed 5/2/08; Reinstated 7/11/08 32 Degrees General Tobacco 2/28/2010 4 Aces - RYO Top Tobacco, LP 11/12/2010 A Touch of Clove Sherman 1400 Broadway N.Y.C. Inc. 9/25/2009 AB Rimboche' - RYO Daughters & Ryan, Inc. 6/18/2010 Ace King Maker Marketing 5/21/2020 All American Value Philip Morris, USA 5/5/2006 All Star Liberty Brands, LLC 5/5/2006 Alpine Philip Morris, USA 8/14/2013 Removed 5/4/07; Reinstated 5/8/09 Always Save Liberty Brands, LLC 5/4/2007 American R.J. Reynolds Tobacco Company 5/6/2005 American Bison Wind River Tobacco Company, LLC 9/22/2015 American Blend Mac Baren Tobacco Company 5/4/2007 American Harvest Sandia Tobacco Manufacturers, Inc. 8/31/2016 American Harvest - RYO Truth & Liberty Manufacturing 8/2/2016 American Liberty Les Tabacs Spokan 5/12/2006 Amphora - RYO Top Tobacco, LP 11/18/2011 Andron's Passion VCT 5/4/2007 Andron's Passion VCT 5/4/2007 Arango Sportsman - RYO Daughters & Ryan, Inc. 6/18/2010 Arbo - RYO VCT 5/4/2007 Ashford Von Eicken Group 5/8/2009 Ashford - RYO Von Eicken Group 12/23/2011 Athey (Old Timer's) Daughters & Ryan, Inc. -

R Street Policy on Tobacco Harm Reduction (THR)
1728 Connecticut Ave, NW 2nd Floor Washington, DC 20009 Free Markets. Real Solutions. 202.525.5717 www.rstreet.org [email protected] R Street Policy on Tobacco Harm Reduction (THR) Tobacco Harm Reduction (THR) is a policy and process by which smokers who are unable or unwilling to quit smoking are enabled and encouraged to switch to a lower risk tobacco/nicotine product to reduce their future risk of potentially fatal cancer, heart and lung disease. All of the illness and death used to justify tobacco control programming in the USA is due to a single tobacco product – the cigarette. Despite lip service to the contrary, American tobacco control policy has the practical effect of reinforcing the cigarette as the primary means of nicotine delivery by protecting cigarettes against competition by far less hazardous non-prescription alternatives. R Street’s founding staff began work on THR when they worked for the Heartland Institute which, in turn, had worked on the issue since the early 1990s. On many issues—such as restrictions on sales of tobacco to minors and the overall dangers of smoking—the two organizations hold the same positions. That being said, R Street and Heartland do not have identical positions on tobacco-related policy or THR. For example, R Street generally supports laws that ban smoking in public places whereas Heartland generally opposes them. THR policy in the United States should be at least partly based on the research now completed showing that the smoke-free products that have been commonly available on the American market since the mid-1980s pose a risk of potentially fatal cancer, heart and lung disease that is less than 2 percent of the risk posed by cigarettes. -
Fiscal Impact Report Deschutes County
July 2017 Deschutes County Fiscal Impact Report Acknowledgments July 2017 This report was produced by the Rede Group for Deschutes County Health Services (DCHS). Stephanie Young-Peterson, MPH Robb Hutson, MA Erin Charpentier, MFA Caralee Oakey We would like to thank the following for their contribution to this project: Penny Pritchard, MPH This project was made possible through Tobacco Master Settlement Agreement grant funding provided by the State of Oregon, Oregon Health Authority to implement tobacco prevention and education Strategies for Policy And enviRonmental Change, Tobacco-Free (SPArC Tobacco-Free). Table of Contents Contents: Background & Introduction....................................................1 Retailer Survey Findings........................................................5 Estimation of TRL Implementation & Enforcement Costs.....15 Conclusion and Committee Recommendation...................21 How Other Jurisdictions are Tackling the Problem.................22 End Notes ..........................................................................23 Appendix: A. Timeline of TRL policy work..........................................26 B. Lane County TRL Ordinance.........................................27 C. Lane County TRL Application........................................37 D. Lane County TRL Inspection Form.................................38 E. Multnomah County TRL Ordinance...............................39 F. Multnomah County TRL Application.............................44 G. Multnomah County TRL Inspection Form......................48 -

Tobacco Harm Reduction
Tobacco Harm Reduction Brad Rodu Professor, Department of Medicine James Graham Brown Cancer Center University of Louisville The Smoking Status Quo: Unacceptable • The American Anti-Smoking Campaign is 45 Years Old • According to the CDC: 45 million smokers in the U.S. 443,000 deaths every year in the U.S. 5,800 in Oklahoma Lung Cancer (ICD 161-162) Mortality in Men and Women Age 35+, Oklahoma and the US, 1979-2009 250 OK Men 200 150 US Men OK Women 100 Deaths per 100,000 py 100,000 Deathsper US Women 50 0 Year If the Status Quo Continues In the next 20 years: • 8 million Americans will die from smoking All are adults over 35 years of age None of them are now children The Failed Anti-Smoking Campaign • The Campaign’s Only Message: Quit Nicotine and Tobacco, or Die • The Campaign’s Only Quitting Tactics: Ineffective Behavioral Therapy Ineffective Use of Nicotine Rodu and Cole. Technology 6: 17-21, 1999. Rodu and Cole. International J Cancer 97: 804-806, 2002. The Anti-Smoking Campaign- Behavioral Therapy • NCI Manual for Physicians- Counsel Patients to: – ”Keep your hands busy- doodle, knit, type a letter” – ”Cut a drinking straw into cigarette-sized pieces and inhale air” – ”Keep a daydream ready to go” Source: How to help your patients stop smoking. NIH Pub. No. 93-3064, 1993 The Anti-Smoking Campaign- Faulted Use of Nicotine • Temporary – 6 to 12 weeks • Expensive – per unit and per box • Very Low Dose – unsatisfying for smokers • 7% Success* – ”Efficacious”, ”Modest” *Hughes et al. Meta-analysis in Tobacco Control, 2003. -

Where Do Youth Smokers Get Their Cigarettes?
WHERE DO YOUTH SMOKERS GET THEIR CIGARETTES? According to the 2020 Monitoring the Future Survey, nearly two out of every five (38.1%) eighth graders and about half (50.4%) of tenth graders say cigarettes are easy for them to get.1 Where and how youth smokers get their cigarettes, however, can vary considerably from state to state or city to city, depending on factors such as whether the jurisdiction strictly enforces the laws prohibiting tobacco sales to minors or requires retailers to keep all tobacco products behind the counter. Some youth smokers buy the cigarettes they smoke, either directly from retailers or other kids, or by giving money to others to buy for them. Others get their cigarettes for free from social sources (usually other kids), and still others obtain their cigarettes by shoplifting or stealing. Nationwide, older youth smokers are more likely to buy their cigarettes directly than younger smokers, who are more likely to get their cigarettes from others or by stealing.2 Some of this difference is because kids who look older typically find it easier to buy cigarettes than younger kids; but another powerful factor is that older youth smokers are more likely to be regular smokers, and regular smokers are much more likely to purchase their own cigarettes than kids who smoke less frequently or are only "experimenting."3 Not surprisingly, older or regular youth smokers who buy their own cigarettes also supply them to kids who do not purchase their own but instead rely on getting them from others.4 Direct Purchases of Cigarettes -
Delegate Frank Turner
Delegate Frank Turner Members of the Committee - It’s come to my attention that the Legislature - in attempting to address the youth vaping epidemic - is considering a ban on menthol cigarettes in the state, and as a former Vice-Chair of the House Ways and Means Committee in particular, I’m very concerned about some of the unintended consequences of this legislation. Very simply, I’m afraid that this approach will expand illegal activity. Research confirms what common sense already tells us: because menthol restrictions amount to an outright ban for smokers who favor that variety, they will resort to illegal sources – an easy thing to do given the nearby presence of states like Virginia and Delaware that are already major suppliers, costing tens of millions of dollars in revenues. Increasing this loss of revenues, of course, would be one unintended consequence of bigger black markets – one estimate puts additional foregone taxes at more than $200 million. But there would be other, equally serious outcomes: • Potentially stopping and even reversing progress in preventing youth smoking. The youth smoking rate has been declining rapidly, especially in Maryland, where the most recent available figures show it dropping more than a third from 2011 to 2017. Black marketers selling loose cigarettes near schools are not going to check IDs or obey the new law restricting sales to 21 and older. • Tainting the cigarette supply. Cigarettes are deadly over time, but tainted supplies could be even more deadly and immediately. The recent fatal vaping lung disease outbreak has been mostly attributed to fake THC vape brands (also aimed at children) with a dangerous additive. -

Health Consequences of Smoking
The Health Consequences of Smoking Executive Summary This report of the Surgeon General on the health This approach separates the classification of the effects of smoking returns to the topic of active smok- evidence concerning causality from the implications ing and disease, the focus of the first Surgeon General’s of that determination. In particular, the magnitude of report published in 1964 (U.S. Department of Health, the effect in the population, the attributable risk, is Education, and Welfare [USDHEW] 1964). The first considered under “implications” of the causal deter- report established a model of comprehensive evidence mination. For example, there might be sufficient evi- evaluation for the 27 reports that have followed: for dence to classify smoking as a cause of two diseases those on the adverse health effects of smoking, the but the number of attributable cases would depend evidence has been evaluated using guidelines for as- on the frequency of the disease in the population and sessing causality of smoking with disease. Using this the effects of other causal factors. model, every report on health has found that smoking This report covers active smoking only. Passive causes many diseases and other adverse effects. Re- smoking was the focus of the 1986 Surgeon General’s peatedly, the reports have concluded that smoking is report and subsequent reports by other entities the single greatest cause of avoidable morbidity and (USDHHS 1986; U.S. Environmental Protection Agen- mortality in the United States. cy [EPA] 1992; California EPA 1997; International Agen- Of the Surgeon General’s reports published since cy for Research on Cancer [IARC] 2002). -

Page 1 of 15
Updated September14, 2021– 9:00 p.m. Date of Next Known Updates/Changes: *Please print this page for your own records* If there are any questions regarding pricing of brands or brands not listed, contact Heather Lynch at (317) 691-4826 or [email protected]. EMAIL is preferred. For a list of licensed wholesalers to purchase cigarettes and other tobacco products from - click here. For information on which brands can be legally sold in Indiana and those that are, or are about to be delisted - click here. *** PLEASE sign up for GovDelivery with your EMAIL and subscribe to “Tobacco Industry” (as well as any other topic you are interested in) Future lists will be pushed to you every time it is updated. *** https://public.govdelivery.com/accounts/INATC/subscriber/new RECENTLY Changed / Updated: 09/14/2021- Changes to LD Club and Tobaccoville 09/07/2021- Update to some ITG list prices and buydowns; Correction to Pall Mall buydown 09/02/2021- Change to Nasco SF pricing 08/30/2021- Changes to all Marlboro and some RJ pricing 08/18/2021- Change to Marlboro Temp. Buydown pricing 08/17/2021- PM List Price Increase and Temp buydown on all Marlboro 01/26/2021- PLEASE SUBSCRIBE TO GOVDELIVERY EMAIL LIST TO RECEIVE UPDATED PRICING SHEET 6/26/2020- ***RETAILER UNDER 21 TOBACCO***(EFF. JULY 1) (on last page after delisting) Minimum Minimum Date of Wholesale Wholesale Cigarette Retail Retail Brand List Manufacturer Website Price NOT Price Brand Price Per Price Per Update Delivered Delivered Carton Pack Premier Mfg. / U.S. 1839 Flare-Cured Tobacco 7/15/2021 $42.76 $4.28 $44.00 $44.21 Growers Premier Mfg. -

JT Completes Share Transfer of Indonesian Kretek Cigarette Company and Its Distributor
FOR IMMEDIATE RELEASE Tokyo, October 31, 2017 JT Completes Share Transfer of Indonesian Kretek Cigarette Company and its Distributor Japan Tobacco Inc. (JT) (TSE: 2914) announced today that the JT Group has completed the transfer of the shares of PT. Karyadibya Mahardhika (KDM), a kretek cigarette company, and its distributor, PT. Surya Mustika Nusantara (SMN). The agreement to this acquisition was announced in the Company’s August 4, 2017 statement1. The transaction is expected to be fully completed in the fourth quarter of the fiscal year 2017 following remaining regulatory clearances. The acquisition is in line with the JT Group’s geographic expansion for sustainable growth. It provides immediate scale and presence on a nationwide level in the Indonesian kretek market and offers a strong distribution platform. The transaction will not have any material impact on the JT Group’s consolidated performance for the fiscal year 2017. ### Japan Tobacco Inc. is a leading international tobacco company. Its products are sold in over 120 countries and its globally recognized brands include Winston, Camel, Mevius, LD and Natural American Spirit. With diversified operations, JT is also actively present in pharmaceuticals and processed foods. The company’s revenue was ¥2.143 trillion (US$19,703 million(*)) in the fiscal year ended December 31, 2016. *Translated at the rate of ¥108.78 per $1 Contacts: Masahito Shirasu, General Manager Media and Investor Relations Division Japan Tobacco Inc. Tokyo: +81-3-5572-4292 E-mail: [email protected] 1 -
Let's Make the Next Generation Tobacco-Free: Your Guide to The
LET’S MAKE THE NEXT GENERATION SARY TOBACCO-FREE A N NIVER Your Guide to the 50th Anniversary Surgeon General’s Report on Smoking and Health U.S. Department of Health and Human Services 50 Years of Progress A Report of the Surgeon General NOTE FROM THE ACTING U.S. SURGEON GENERAL Rear Admiral Boris D. Lushniak, M.D., M.P.H., Acting Surgeon General I am pleased and honored to release The Health Consequences of Smoking: 50 Years of Progress, the 50th Anniversary Surgeon General’s Report on Smoking and Health. This new report: l looks back at the important gains we have made in reducing tobacco use over the last half-century; l catalogs the devastating effects smoking and exposure to secondhand smoke have on the human body; and l looks at the work still to be done to achieve our goal of a society free from tobacco-related disease and death. Because the report itself is written mostly for a scientific and medical audience, we have created this consumer guide to explain the report in language we can all understand. This guide details devastating effects of smoking including nicotine addiction and serious disease. It shows that 5.6 million of today’s children will ultimately die early from smoking if we do not do more to reduce current smoking rates. And it shows that 2.5 million nonsmokers have died from secondhand smoke since 1964. It also contains important facts on the benefits of quitting smoking and free resources that are available to smokers who want to quit.