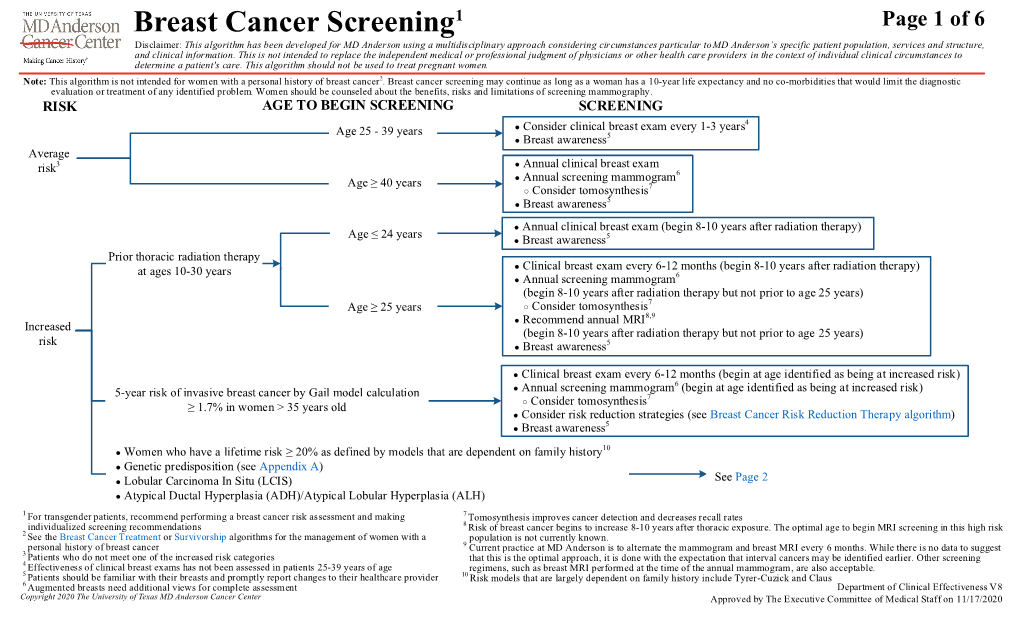
Breast Cancer Screening
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Medical Oncology and Breast Cancer
The Breast Center Smilow Cancer Hospital 20 York Street, North Pavilion New Haven, CT 06510 Phone: (203) 200-2328 Fax: (203) 200-2075 MEDICAL ONCOLOGY Treatment for breast cancer is multidisciplinary. The primary physicians with whom you may meet as part of your care are the medical oncologist, the breast surgeon, and often the radiation oncologist. A list of these specialty physicians will be provided to you. Each provider works with a team of caregivers to ensure that every patient receives high quality, personalized, breast cancer care. The medical oncologist specializes in “systemic therapy”, or medications that treat the whole body. For women with early stage breast cancer, systemic therapy is often recommended to provide the best opportunity to prevent breast cancer from returning. SYSTEMIC THERAPY Depending on the specific characteristics of your cancer, your medical oncologist may prescribe systemic therapy. Systemic therapy can be hormone pills, IV chemotherapy, antibody therapy (also called “immunotherapy”), and oral chemotherapy; sometimes patients receive more than one type of systemic therapy. Systemic therapy can happen before surgery (called “neoadjuvant therapy”) or after surgery (“adjuvant therapy”). If appropriate, your breast surgeon and medical oncologist will discuss the benefits of neoadjuvant and adjuvant therapy with you. As a National Comprehensive Cancer Network (NCCN) Member Institution, we are dedicated to following the treatment guidelines that have been shown to be most effective. We also have a variety of clinical trials that will help us find better ways to treat breast cancer. Your medical oncologist will recommend what treatment types and regimens are best for you. The information used to make these decisions include: the location of the cancer, the size of the cancer, the type of cancer, whether the cancer is invasive, the grade of the cancer (a measure of its aggressiveness), prognostic factors such as hormone receptors and HER2 status, and lymph node involvement. -
Exposure to Carcinogens and Work-Related Cancer: a Review of Assessment Methods
European Agency for Safety and Health at Work ISSN: 1831-9343 Exposure to carcinogens and work-related cancer: A review of assessment methods European Risk Observatory Report Exposure to carcinogens and work-related cancer: A review of assessment measures Authors: Dr Lothar Lißner, Kooperationsstelle Hamburg IFE GmbH Mr Klaus Kuhl (task leader), Kooperationsstelle Hamburg IFE GmbH Dr Timo Kauppinen, Finnish Institute of Occupational Health Ms Sanni Uuksulainen, Finnish Institute of Occupational Health Cross-checker: Professor Ulla B. Vogel from the National Working Environment Research Centre in Denmark Project management: Dr Elke Schneider - European Agency for Safety and Health at Work (EU-OSHA) Europe Direct is a service to help you find answers to your questions about the European Union Freephone number (*): 00 800 6 7 8 9 10 11 (*) Certain mobile telephone operators do not allow access to 00 800 numbers, or these calls may be billed. More information on the European Union is available on the Internet ( 48TU http://europa.euU48T). Cataloguing data can be found on the cover of this publication. Luxembourg: Publications Office of the European Union, 2014 ISBN: 978-92-9240-500-7 doi: 10.2802/33336 Cover pictures: (clockwise): Anthony Jay Villalon (Fotolia); ©Roman Milert (Fotolia); ©Simona Palijanskaite; ©Kari Rissa © European Agency for Safety and Health at Work, 2014 Reproduction is authorised provided the source is acknowledged. European Agency for Safety and Health at Work – EU-OSHA 1 Exposure to carcinogens and work-related cancer: -

About Ovarian Cancer Overview and Types
cancer.org | 1.800.227.2345 About Ovarian Cancer Overview and Types If you have been diagnosed with ovarian cancer or are worried about it, you likely have a lot of questions. Learning some basics is a good place to start. ● What Is Ovarian Cancer? Research and Statistics See the latest estimates for new cases of ovarian cancer and deaths in the US and what research is currently being done. ● Key Statistics for Ovarian Cancer ● What's New in Ovarian Cancer Research? What Is Ovarian Cancer? Cancer starts when cells in the body begin to grow out of control. Cells in nearly any part of the body can become cancer and can spread. To learn more about how cancers start and spread, see What Is Cancer?1 Ovarian cancers were previously believed to begin only in the ovaries, but recent evidence suggests that many ovarian cancers may actually start in the cells in the far (distal) end of the fallopian tubes. 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 What are the ovaries? Ovaries are reproductive glands found only in females (women). The ovaries produce eggs (ova) for reproduction. The eggs travel from the ovaries through the fallopian tubes into the uterus where the fertilized egg settles in and develops into a fetus. The ovaries are also the main source of the female hormones estrogen and progesterone. One ovary is on each side of the uterus. The ovaries are mainly made up of 3 kinds of cells. Each type of cell can develop into a different type of tumor: ● Epithelial tumors start from the cells that cover the outer surface of the ovary. -

Preventive Health Care
PREVENTIVE HEALTH CARE DANA BARTLETT, BSN, MSN, MA, CSPI Dana Bartlett is a professional nurse and author. His clinical experience includes 16 years of ICU and ER experience and over 20 years of as a poison control center information specialist. Dana has published numerous CE and journal articles, written NCLEX material, written textbook chapters, and done editing and reviewing for publishers such as Elsevire, Lippincott, and Thieme. He has written widely on the subject of toxicology and was recently named a contributing editor, toxicology section, for Critical Care Nurse journal. He is currently employed at the Connecticut Poison Control Center and is actively involved in lecturing and mentoring nurses, emergency medical residents and pharmacy students. ABSTRACT Screening is an effective method for detecting and preventing acute and chronic diseases. In the United States healthcare tends to be provided after someone has become unwell and medical attention is sought. Poor health habits play a large part in the pathogenesis and progression of many common, chronic diseases. Conversely, healthy habits are very effective at preventing many diseases. The common causes of chronic disease and prevention are discussed with a primary focus on the role of health professionals to provide preventive healthcare and to educate patients to recognize risk factors and to avoid a chronic disease. nursece4less.com nursece4less.com nursece4less.com nursece4less.com 1 Policy Statement This activity has been planned and implemented in accordance with the policies of NurseCe4Less.com and the continuing nursing education requirements of the American Nurses Credentialing Center's Commission on Accreditation for registered nurses. It is the policy of NurseCe4Less.com to ensure objectivity, transparency, and best practice in clinical education for all continuing nursing education (CNE) activities. -

Colorectal Cancer Screening Algorithm
Colorectal Cancer Screening Page 1 of 6 Disclaimer: This algorithm has been developed for MD Anderson using a multidisciplinary approach considering circumstances particular to MD Anderson’s specific patient population, services and structure, and clinical information. This is not intended to replace the independent medical or professional judgment of physicians or other health care providers in the context of individual clinical circumstances to determine a patient's care. This algorithm should not be used to treat pregnant women. This algorithm is not intended for individuals with a personal history of colorectal cancer 1. Note: Screening for adults age 76 to 85 years old should be evaluated on an individual basis by their health care provider to assess the risks and benefits of screen ing. Colorectal cancer screening is not recommended over age 85 years. TABLE OF CONTENTS Average Risk …………..………………...……………………..………………………………...Page 2 Increased Risk ………………………...…………………...………….………………………….Page 3 High Risk ………………………………………………………………………………………....Page 4 Suggested Readings …………………………………...……...………………………………….Page 5 Development Credits ………………………………………………….........................................Page 6 1 See the Colon or Rectal Cancer Treatment or Survivorship algorithms for the management of individuals with a personal history of colorectal cancer Department of Clinical Effectiveness V9 Approved by the Executive Committee of the Medical Staff on 09/21/2021 Colorectal Cancer Screening – Average Risk Page 2 of 6 Disclaimer: This algorithm has been developed for MD Anderson using a multidisciplinary approach considering circumstances particular to MD Anderson’s specific patient population, services and structure, and clinical information. This is not intended to replace the independent medical or professional judgment of physicians or other health care providers in the context of individual clinical circumstances to determine a patient's care. -

Primary Screening for Breast Cancer with Conventional Mammography: Clinical Summary
Primary Screening for Breast Cancer With Conventional Mammography: Clinical Summary Population Women aged 40 to 49 y Women aged 50 to 74 y Women aged ≥75 y The decision to start screening should be No recommendation. Recommendation Screen every 2 years. an individual one. Grade: I statement Grade: B Grade: C (insufficient evidence) These recommendations apply to asymptomatic women aged ≥40 y who do not have preexisting breast cancer or a previously diagnosed high-risk breast lesion and who are not at high risk for breast cancer because of a known underlying genetic mutation Risk Assessment (such as a BRCA1 or BRCA2 gene mutation or other familial breast cancer syndrome) or a history of chest radiation at a young age. Increasing age is the most important risk factor for most women. Conventional digital mammography has essentially replaced film mammography as the primary method for breast cancer screening Screening Tests in the United States. Conventional digital screening mammography has about the same diagnostic accuracy as film overall, although digital screening seems to have comparatively higher sensitivity but the same or lower specificity in women age <50 y. For women who are at average risk for breast cancer, most of the benefit of mammography results from biennial screening during Starting and ages 50 to 74 y. While screening mammography in women aged 40 to 49 y may reduce the risk for breast cancer death, the Stopping Ages number of deaths averted is smaller than that in older women and the number of false-positive results and unnecessary biopsies is larger. The balance of benefits and harms is likely to improve as women move from their early to late 40s. -

Hematopoietic and Lymphoid Neoplasm Coding Manual
Hematopoietic and Lymphoid Neoplasm Coding Manual Effective with Cases Diagnosed 1/1/2010 and Forward Published August 2021 Editors: Jennifer Ruhl, MSHCA, RHIT, CCS, CTR, NCI SEER Margaret (Peggy) Adamo, BS, AAS, RHIT, CTR, NCI SEER Lois Dickie, CTR, NCI SEER Serban Negoita, MD, PhD, CTR, NCI SEER Suggested citation: Ruhl J, Adamo M, Dickie L., Negoita, S. (August 2021). Hematopoietic and Lymphoid Neoplasm Coding Manual. National Cancer Institute, Bethesda, MD, 2021. Hematopoietic and Lymphoid Neoplasm Coding Manual 1 In Appreciation NCI SEER gratefully acknowledges the dedicated work of Drs, Charles Platz and Graca Dores since the inception of the Hematopoietic project. They continue to provide support. We deeply appreciate their willingness to serve as advisors for the rules within this manual. The quality of this Hematopoietic project is directly related to their commitment. NCI SEER would also like to acknowledge the following individuals who provided input on the manual and/or the database. Their contributions are greatly appreciated. • Carolyn Callaghan, CTR (SEER Seattle Registry) • Tiffany Janes, CTR (SEER Seattle Registry) We would also like to give a special thanks to the following individuals at Information Management Services, Inc. (IMS) who provide us with document support and web development. • Suzanne Adams, BS, CTR • Ginger Carter, BA • Sean Brennan, BS • Paul Stephenson, BS • Jacob Tomlinson, BS Hematopoietic and Lymphoid Neoplasm Coding Manual 2 Dedication The Hematopoietic and Lymphoid Neoplasm Coding Manual (Heme manual) and the companion Hematopoietic and Lymphoid Neoplasm Database (Heme DB) are dedicated to the hard-working cancer registrars across the world who meticulously identify, abstract, and code cancer data. -

Understanding the Randomized Controlled Trials By
Breast Cancer Screening: Understanding the Randomized Controlled Trials By: Phoebe Freer, MD, Linda Moy, MD, FSBI, Wendy DeMartini, MD, FSBI, and the Screening Leadership Group Screening mammography has been shown to decrease breast cancer mortality across multiple trials, and across many different study designs. Despite this, some opponents continue to question the value of mammography. Thus, it is increasingly important that breast imaging care providers understand the nature and results of the randomized controlled trials (RCTs), which have definitively demonstrated that screening mammography in women 40-74 years of age decreases deaths from breast cancer. Cancer localized in the breast is not what causes death; it is breast cancer spread (metastasis) to other organs that causes mortality. The goal of mammographic screening (and other breast cancer screening tests) is to detect breast cancer earlier than it would otherwise manifest clinically, when it is less likely to have spread. Data clearly show that detection of breast cancers at smaller sizes and lower stages is associated with better patient outcomes from lower morbidity and reduced breast cancer deaths. RCTs are the gold standard for proving that early detection with mammography decreases mortality from breast cancer. It is important to understand that the key evidence measure is the breast cancer death rate observed in the experimental group (women invited to have screening mammography) compared to that in the control group (women not invited to have screening mammography). It is not sufficient to use survival time (the time of discovery of the cancer to the date of death) between the groups, as this may reflect “lead-time” bias, in which a cancer is found earlier so survival time appears longer, but the date of death is not altered. -

Evidence Synthesis Number 197 Screening for Hypertension in Adults
Evidence Synthesis Number 197 Screening for Hypertension in Adults: A Systematic Evidence Review for the U.S. Preventive Services Task Force Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 5600 Fishers Lane Rockville, MD 20857 www.ahrq.gov Contract No. HHSA-290-2015-000017-I-EPC5, Task Order No. 5 Prepared by: Kaiser Permanente Research Affiliates Evidence-based Practice Center Kaiser Permanente Center for Health Research Portland, OR Investigators: Janelle M. Guirguis-Blake, MD Corinne V. Evans, MPP Elizabeth M. Webber, MS Erin L. Coppola, MPH Leslie A. Perdue, MPH Meghan Soulsby Weyrich, MPH AHRQ Publication No. 20-05265-EF-1 June 2020 This report is based on research conducted by the Kaiser Permanente Research Affiliates Evidence-based Practice Center (EPC) under contract to the Agency for Healthcare Research and Quality (AHRQ), Rockville, MD (Contract No. HHSA-290-2015-000017-I-EPC5, Task Order No. 5). The findings and conclusions in this document are those of the authors, and do not necessarily represent the views of AHRQ. Therefore, no statement in this report should be construed as an official position of AHRQ or of the U.S. Department of Health and Human Services. The information in this report is intended to help health care decision makers—patients and clinicians, health system leaders, and policymakers, among others—make well-informed decisions and thereby improve the quality of health care services. This report is not intended to be a substitute for the application of clinical judgment. Anyone who makes decisions concerning the provision of clinical care should consider this report in the same way as any medical reference and in conjunction with all other pertinent information (i.e., in the context of available resources and circumstances presented by individual patients). -

Early Detection and Screening for Breast Cancer
Seminars in Oncology Nursing, Vol 33, No 2 (May), 2017: pp 141-155 141 EARLY DETECTION AND SCREENING FOR BREAST CANCER CATHY COLEMAN OBJECTIVE: To review the history, current status, and future trends related to breast cancer screening. DATA SOURCES: Peer-reviewed articles, web sites, and textbooks. CONCLUSION: Breast cancer remains a complex, heterogeneous disease. Serial screening with mammography is the most effective method to detect early stage disease and decrease mortality. Although politics and economics may inhibit organized mammography screening programs in many countries, the judi- cious use of proficient clinical and self-breast examination can also identify small tumors leading to reduced morbidity. IMPLICATIONS FOR NURSING PRACTICE: Oncology nurses have exciting oppor- tunities to lead, facilitate, and advocate for delivery of high-quality screening services targeting individuals and communities. A practical approach is needed to translate the complexities and controversies surrounding breast cancer screen- ing into improved care outcomes. KEY WORDS: breast cancer, screening, early stage, quality, breast centers, advocacy. he future is hopeful for the public, pro- fessionals, and interdisciplinary teams as multifaceted progress continues to reveal new insights in carcinogenesis, ge- Cathy Coleman, DNP, MSN, PHN, OCN®, CPHQ, CNL: T nomics, tumor biology, translational research, and Assistant Professor, University of San Francisco School quality improvement from prevention to pallia- of Nursing and Health Professions, San Francisco, CA. tion and survivorship for cancer care.1-8 Oncology Address correspondence to Cathy Coleman, DNP, nurses are on the front line of care delivery across MSN, PHN, OCN®, CPHQ, CNL, University of San settings; they also assert a strong leadership voice Francisco School of Nursing and Health Professions, 2130 Fulton Street, San Francisco, CA 94117. -

State of Science Breast Cancer Fact Sheet
Patient Version Breast Cancer Fact Sheet About Breast Cancer Breast cancer can start in any area of the breast. In the US, breast cancer is the most common cancer (after skin cancer) and the second-leading cause of cancer death (after lung cancer) in women. Risk Factors Risk factors for breast cancer that you cannot change Lifestyle-related risk factors for breast cancer include: • Drinking alcohol Being born female • Being overweight or obese, especially after menopause This is the main risk factor for breast cancer. But men can get breast cancer, too. • Not being physically active Getting older • Getting hormone therapy after menopause with As a person gets older, their risk of breast cancer estrogen and progesterone therapy goes up. Most breast cancers are found in women • Starting menstruation early or having late menopause age 55 or older. • Never having children or having first live birth after Personal or family history age 30 A woman who has had breast cancer in the past or has a • Using certain types of birth control close blood relative who has had breast cancer (mother, • Having a history of non-cancerous breast conditions father, sister, brother, daughter) has a higher risk of getting it. Having more than one close blood relative increases the risk even more. It’s important to know that Prevention most women with breast cancer don’t have a close blood There is no sure way to prevent breast cancer, and relative with the disease. some risk factors can’t be changed, such as being born female, age, race, and personal or family history of the Inheriting gene changes disease. -

Lung Cancer Screening with Sputum Cytologic Examination, Chest Radiography, and Computed Tomography: an Update for the U.S
Lung Cancer Screening with Sputum Cytologic Examination, Chest Radiography, and Computed Tomography: An Update for the U.S. Preventive Services Task Force Linda L. Humphrey, MD, MPH; Steven Teutsch, MD, MPH; Mark S. Johnson, MD, MPH Screening for lung cancer is not currently increasing in epidemic proportions,3,4 with an recommended by any major medical professional estimated 1 million deaths in the year 2000.5 organization. The U.S. Preventive Services Task Although there are other important risk factors Force (USPSTF) gave lung cancer screening a “D” for lung cancer,3,6–10 cigarette smoking is the major recommendation in both 1985 and 1996, meaning risk factor; approximately 87% of all lung, that there were fair-quality data to recommend bronchial, and tracheal cancer are attributed to against screening for lung cancer1 based largely on 3 smoking.3 Consequently, the most important public negative trials conducted in the United States in the health intervention that could reduce lung cancer 1970s. Since the last Task Force review, several new incidence and deaths is changing smoking habits. studies of lung cancer screening have been reported, Unfortunately, although overall prevalence rates of and greater attention has been directed toward the smoking in the United States have decreased over limitations of existing literature. This review was the past 2 decades, the prevalence of current adult conducted to aid the current USPSTF in updating smokers remains high at 24%.10,11 In the clinical its lung cancer screening recommendation. setting,