Cardiac Physical Diagnosis: a Proctor Harvey Approach
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Essentials of Bedside Cardiology CONTEMPORARY CARDIOLOGY
Essentials of Bedside Cardiology CONTEMPORARY CARDIOLOGY CHRISTOPHER P. CANNON, MD SERIES EDITOR Aging, Heart Disease and Its Management: Facts and Controversies, edited by Niloo M. Edwards, MD, Mathew S. Maurer, MD, and Rachel B. Wellner, MD, 2003 Peripheral Arterial Disease: Diagnosis and Treatment, edited by Jay D. Coffman, MD, and Robert T. Eberhardt, MD, 2003 Essentials ofBedside Cardiology: With a Complete Course in Heart Sounds and Munnurs on CD, Second Edition, by Jules Constant, MD, 2003 Primary Angioplasty in Acute Myocardial Infarction, edited by James E. Tcheng, MD,2002 Cardiogenic Shock: Diagnosis and Treatment, edited by David Hasdai, MD, Peter B. Berger, MD, Alexander Battler, MD, and David R. Holmes, Jr., MD, 2002 Management of Cardiac Arrhythmias, edited by Leonard I. Ganz, MD, 2002 Diabetes and Cardiovascular Disease, edited by Michael T. Johnstone and Aristidis Veves, MD, DSC, 2001 Blood Pressure Monitoring in Cardiovascular Medicine and Therapeutics, edited by William B. White, MD, 2001 Vascular Disease and Injury: Preclinical Research, edited by Daniell. Simon, MD, and Campbell Rogers, MD 2001 Preventive Cardiology: Strategies for the Prevention and Treatment of Coronary Artery Disease, edited by JoAnne Micale Foody, MD, 2001 Nitric Oxide and the Cardiovascular System, edited by Joseph Loscalzo, MD, phD and Joseph A. Vita, MD, 2000 Annotated Atlas of Electrocardiography: A Guide to Confident Interpretation, by Thomas M. Blake, MD, 1999 Platelet Glycoprotein lIb/IlIa Inhibitors in Cardiovascular Disease, edited by A. Michael Lincoff, MD, and Eric J. Topol, MD, 1999 Minimally Invasive Cardiac Surgery, edited by Mehmet C. Oz, MD and Daniel J. Goldstein, MD, 1999 Management ofAcute Coronary Syndromes, edited by Christopher P. -

Viding Diagnostic Insights Into the Pathophysiologic Mechanisms
viding diagnostic insights into the pathophysiologic mechanisms under- lying the acoustic findings heard in clinical practice.162-165 Contemporary physicians should take advantage of the valuable clinical information that can be obtained by such an inexpensive instrument and expedient and reli- able tool as the stethoscope. The following section reviews the funda- mental technique of cardiac auscultation, emphasizing the diagnostic value and practical clinical applications of this time-honored (but endan- gered) art in this time of need.166 The Art and Technique of Cardiac Auscultation. Auscultation of the heart and vascular system is one of the most challenging and rewarding clinical diagnostic skills that can (and should) be learned and applied by every prac- ticing physician. Proficiency in cardiac auscultation requires experience, repeated practice, and a great deal of patience (and patients). Most impor- tantly, it requires a proper state of mind. (“we hear what we listen for”). Although the most vital component of the auscultatory apparatus lies between the earpieces, the proper use of a well-designed, efficient stetho- scope cannot be overemphasized. To ensure optimal sound transmission, the well-crafted stethoscope should be airtight, with snug but comfortably-fit- ting earpieces, properly aligned metal binaurals, and flexible, double-barrel, 1 thick-walled tubing, ⁄8 inch in internal diameter and no more than 12 to 15 inches in length. A high-quality stethoscope should be equipped with both bell and diaphragm chest pieces. The bell, when applied gently to the skin, will “bring out” low frequency sounds and murmurs (eg, faint S4 or S3 gal- lop or diastolic rumble) and the diaphragm, when pressed firmly against the skin, will accentuate high-pitched acoustic events (eg, diastolic blowing murmur of AR). -

Systolic Murmurs
Murmurs and the Cardiac Physical Exam Carolyn A. Altman Texas Children’s Hospital Advanced Practice Provider Conference Houston, TX April 6 , 2018 The Cardiac Physical Exam Before applying a stethoscope….. Some pearls on • General appearance • Physical exam beyond the heart 2 Jugular Venous Distention Pallor Cyanosis 3 Work of Breathing Normal infant breathing Quiet Tachypnea Increased Rate, Work of Breathing 4 Beyond the Chest Clubbing Observed in children older than 6 mos with chronic cyanosis Loss of the normal angle of the nail plate with the axis of the finger Abnormal sponginess of the base of the nail bed Increasing convexity of the nail Etiology: ? sludging 5 Chest ❖ Chest wall development and symmetry ❖ Long standing cardiomegaly can lead to hemihypertrophy and flared rib edge: Harrison’s groove or sulcus 6 Ready to Examine the Heart Palpation Auscultation General overview Defects Innocent versus pathologic 7 Cardiac Palpation ❖ Consistent approach: palm of your hand, hypothenar eminence, or finger tips ❖ Precordium, suprasternal notch ❖ PMI? ❖ RV impulse? ❖ Thrills? ❖ Heart Sounds? 8 Cardiac Auscultation Where to listen: ★ 4 main positions ★ Inching ★ Ancillary sites: don’t forget the head in infants 9 Cardiac Auscultation Focus separately on v Heart sounds: • S2 normal splitting and intensity? • Abnormal sounds? Clicks, gallops v Murmurs v Rubs 10 Cardiac Auscultation Etiology of heart sounds: Aortic and pulmonic valves actually close silently Heart sounds reflect vibrations of the cardiac structures after valve closure Sudden -

1. Intermittent Chest Pain: Angina: • Stable: (Caused By
CVS: 1. Intermittent chest pain: Angina: • Stable: (caused by chronic narrowing in one or more coronary arteries), episodes of pain are precipitated by exertion and may occur more readily when walking in cold or windy weather, after a large meal or while carrying a heavy load; the pain is promptly relieved by rest and/or sublingual glyceryl nitrate (GTN) spray, and typically lasts for less than 10 minutes. • unstable angina (caused by a sudden severe narrowing in a coronary artery), there is usually an abrupt onset or worsening of chest pain episodes that may occur on minimal exertion or at rest. • Retrosternal/ Progressive onset/ increase in intensity over 1–2 minutes/ Constricting, heavy/ Sometimes arm(s), neck, epigastrium/ Associated with breathlessness/ Intermittent, with episodes lasting 2–10 minutes/ Triggered by emotion, exertion, especially if cold, windy/ Relieved by rest, nitrates Mild to moderate. • Aggravated by thyroxine or drug-induced anemia, e.g. aspirin or NSAIDs Esophageal: • Retrosternal or epigastric/ Over 1–2 minutes; can be sudden (spasm)/ C: Gripping, tight or burning/ R: Often to back, sometimes to arms/ A: Heartburn, acid reflux/ T: Intermittent, often at night-time; variable duration/ Lying flat/some foods may trigger/ Not relieved by rest; nitrates sometimes relieve/ Usually mild but esophageal spasm can mimic myocardial infarction. 2. Acute chest pain: MI: • SOCRATES: Retrosternal/ Rapid over a few minutes/ Constricting, heavy/ Often to arm(s), neck, jaw, sometimes epigastrium/ Sweating, nausea, vomiting, breathlessness, feeling of impending death (angor animi)/ Acute presentation; prolonged duration/ ’Stress’ and exercise rare triggers, usually spontaneous/ Not relieved by rest or nitrates/ Usually severe. -

Valvular Heart Disease Acute Rheumatic Fever
Valvular heart disease Acute rheumatic fever Rheumatic fever • It typically occurs several weeks after streptococcal pharyngitis. • The most common pathogen is group A beta-hemolytic streptococci (GABHS) • Streptococcus cross-react with proteins in cardiac valves. • Time from acute streptococcal infection to onset of symptomatic rheumatic fever (RF) is usually 3–4 weeks. • RF is thought to complicate up to 3% of untreated streptococcal sore throats. • Previous episodes of RF predispose to recurrences. Diagnostic criteria for rheumatic fever (Jones criteria) • Evidence of group A streptococcal pharyngitis • Either a positive throat culture or rapid streptococcal antigen test, or an elevated or rising streptococcal antibody titer (samples taken 2 weeks apart). • Plus two major or one major and two minor Jones criteria: Major criteria Minor criteria • Polyarthritis • Fever • Carditis • Arthralgia • Chorea • Prolonged PR interval • Erythema marginatum • Elevated ESR and CRP • Subcutaneous nodules Joints • Migratory large-joint polyarthritis starting in the lower limbs in 75% of cases. Duration is <4 weeks at each site. There is severe pain and tenderness in contrast to a mild degree of joint swelling. Heart • Pancarditis occurs in 50% of cases with features of acute heart failure, mitral and aortic regurgitation, and pericarditis. • Endocarditis • affects the mitral valve (65%–70%), aortic valve (25%), and tricuspid valve (10%, never in isolation), causing acute regurgitation and heart failure but chronic stenosis. • Pericarditis • Pain • Friction rub • rarely causes hemodynamic instability/tamponade or constriction. Heart Myocarditis • Acute heart failure • Arrhythmias • Most common reason of death Skin • Erythema marginatum is an evanescent rash with serpiginous outlines and central clearings on the trunk and proximal limbs. -

ACC/AAP/AHA/ASE/HRS/SCAI/SCCT/SCMR/SOPE 2014 Appropriate Use Criteria for Initial Transthoracic Echocardiography in Outpatient P
JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY VOL. - ,NO.- ,2014 ª 2014 BY THE AMERICAN COLLEGE OF CARDIOLOGY FOUNDATION ISSN 0735-1097/$36.00 PUBLISHED BY ELSEVIER INC. http://dx.doi.org/10.1016/j.jacc.2014.08.003 1 APPROPRIATE USE CRITERIA 55 2 56 3 57 4 ACC/AAP/AHA/ASE/HRS/ 58 5 59 6 SCAI/SCCT/SCMR/SOPE 60 7 61 8 2014 Appropriate Use Criteria for 62 9 63 10 Initial Transthoracic Echocardiography 64 11 65 12 in Outpatient Pediatric Cardiology 66 13 67 14 A Report of the American College of Cardiology Appropriate Use Criteria Task Force, 68 15 American Academy of Pediatrics, American Heart Association, American Society of 69 16 Echocardiography, Heart Rhythm Society, Society for Cardiovascular Angiography and 70 17 Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular 71 18 Magnetic Resonance, and Society of Pediatric Echocardiography 72 19 73 20 74 21 75 22 76 Q1 Writing Group for Robert M. Campbell, MD, FACC, FAHA, FAAP, FHRS, Wyman W. Lai, MD, MPH, FACC, FASE 23 77 Echocardiography Chair Leo Lopez, MD, FACC, FAAP, FASE 24 78 in Outpatient Ritu Sachdeva, MD, FACC, FAAP, FASE 25 79 Pediatric Pamela S. Douglas, MD, MACC, FAHA, FASE 26 80 Cardiology Benjamin W. Eidem, MD, FACC, FASE 27 81 28 82 29 83 30 Rating Panel Robert M. Campbell, MD, FACC, FAHA, FAAP, FHRS, Richard Lockwood, MD** 84 yy 31 Chair* G. Paul Matherne, MD, MBA, FACC, FAHA 85 zz 32 Pamela S. Douglas, MD, MACC, FAHA, FASE, Moderator* David Nykanen, MD, FACC 86 yy 33 Catherine L. -

Pregnancy and Cardiovascular Disease
Pregnancy and Cardiovascular Disease Cindy M. Martin, M.D. Co-Director, Adult Congenital and Cardiovascular Genetics Center No Disclosures Objectives • Discuss the hemodynamic changes during pregnancy • Define the low, medium and high risk cardiac lesions as related to pregnancy • Review use of cardiovascular drugs in pregnancy Pregnancy and the Heart • 2-4% of pregnancies in women without preexisting cardiac abnormalities are complicated by maternal CV disease • In 2000, there were an estimated 1 million adult patients in the US with congenital heart disease (CHD), with the number increasing by 5% yearly • In 2005, the number of adult patients with CHD surpassed the number of children with CHD in the United States • CV and CHD disease does not always preclude pregnancy but may pose increase risk to mother and fetus Hemodynamic Changes during Pregnancy • Blood Volume – increases 40-50% • Heart rate – increases 10-15 bpm • SVR and PVR – decreases • Blood Pressure – decreases 10mmHg • Cardiac Output – increases 30-50% – Peaks at end of second trimester and plateaus until delivery • These changes are usually well tolerated Physiologic Changes in Pregnancy Hemodynamic Changes in Labor and Delivery • CO increases an additional 50% with each contraction – Uterine contraction displaces 300-500ml blood into the general circulation – Possible for the cardiac output to be 70-80% above baseline during labor and delivery • Mean arterial pressure also usually rises • Volume changes – Increased blood volume with uterine contraction – Increase venous -

An Audio Guide to Pediatric and Adult Heart Murmurs
Listen Up! An Audio Guide to Pediatric and Adult Heart Murmurs May 9, 2018 Dr. Michael Grattan Dr. Andrew Thain https://pollev.com/michaelgratt679 Case • You are working at an urgent care centre when a 40 year old recent immigrant from Syria presents with breathlessness. • You hear the following on cardiac auscultation: • What do you hear? • How can you describe what you hear so another practitioner will understand exactly what you mean? • What other important information will help you determine the significance of your auscultation? Objectives • In pediatric and adult patients: – To provide a general approach to cardiac auscultation – To review the most common pathologic and innocent heart murmurs • To emphasize the importance of a thorough history and physical exam (in addition to murmur description) in determining underlying etiology for heart problems Outline • A little bit of physiology and hemodynamics (we promise not too much) • Interactive pediatric and adult cases – https://pollev.com/michaelgratt679 – Get your listening ears ready! • Systolic murmurs (pathologic and innocent) • Diastolic murmurs • Continuous murmurs • Some other stuff Normal Heart Sounds Normal First & Second Sounds Splitting of 2nd heart sound Physiological : • Venous return to right is increased in inspiration – causes delayed closure of the pulmonary valve. • Simultaneously, return to left heart is reduced - premature closure of the aortic valve. • Heart sounds are unsplit when the patient holds breath at end expiration. Fixed: • No alteration in splitting with respiration. • In a patient with ASD – In expiration there is reduced pressure in the right atrium and increased pressure in the left atrium. • Blood is shunted to the right and this delays closure of the pulmonary valve in the same way as would occur in inspiration. -

Cardiology 1
Cardiology 1 SINGLE BEST ANSWER (SBA) a. Sick sinus syndrome b. First-degree AV block QUESTIONS c. Mobitz type 1 block d. Mobitz type 2 block 1. A 19-year-old university rower presents for the pre- e. Complete heart block Oxford–Cambridge boat race medical evaluation. He is healthy and has no significant medical history. 5. A 28-year-old man with no past medical history However, his brother died suddenly during football and not on medications presents to the emergency practice at age 15. Which one of the following is the department with palpitations for several hours and most likely cause of the brother’s death? was found to have supraventricular tachycardia. a. Aortic stenosis Carotid massage was attempted without success. b. Congenital long QT syndrome What is the treatment of choice to stop the attack? c. Congenital short QT syndrome a. Intravenous (IV) lignocaine d. Hypertrophic cardiomyopathy (HCM) b. IV digoxin e. Wolff–Parkinson–White syndrome c. IV amiodarone d. IV adenosine 2. A 65-year-old man presents to the heart failure e. IV quinidine outpatient clinic with increased shortness of breath and swollen ankles. On examination his pulse was 6. A 75-year-old cigarette smoker with known ischaemic 100 beats/min, blood pressure 100/60 mmHg heart disease and a history of cardiac failure presents and jugular venous pressure (JVP) 10 cm water. + to the emergency department with a 6-hour history of The patient currently takes furosemide 40 mg BD, increasing dyspnoea. His ECG shows a narrow complex spironolactone 12.5 mg, bisoprolol 2.5 mg OD and regular tachycardia with a rate of 160 beats/min. -
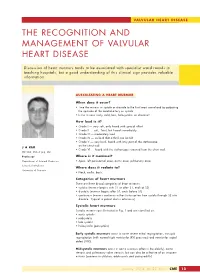
The Recognition and Management of Valvular Heart Disease
VALVULAR HEART DISEASE THE RECOGNITION AND MANAGEMENT OF VALVULAR HEART DISEASE Discussion of heart murmurs tends to be associated with specialist ward rounds in teaching hospitals, but a good understanding of this clinical sign provides valuable information. AUSCULTATING A HEART MURMUR When does it occur? •Time the murmur in systole or diastole to the first heart sound and by palpating the upstroke of the carotid artery as systole. • Is the murmur early, mild, late, holosystolic, or diastolic? How loud is it? •Grade I — very soft, only heard with special effort • Grade II — soft, faint, but heard immediately • Grade III — moderately loud • Grade IV — so loud that a thrill can be felt •Grade V — very loud, heard with only part of the stethoscope on the chest wall J A KER • Grade VI — heard with the stethoscope removed from the chest wall. MB ChB, MMed (Int), MD Professor Where is it maximal? Department of Internal Medicine • Apex, left parasternal area, aortic area, pulmonary area. School of Medicine Where does it radiate to? University of Pretoria • Neck, axilla, back. Categories of heart murmurs There are three broad categories of heart murmurs: • systolic (murmur begins with S1 or after S1, ends at S2) • diastolic (murmur begins after S2, ends before S1) • continuous (murmur continues without interruption from systole through S2 into diastole. Typical in patent ductus arteriosus). Systolic heart murmurs Systolic murmurs are illustrated in Fig. 1 and are classified as: • early systolic • midsystolic •late systolic • holosystolic (pansystolic) Early systolic murmurs occur in acute severe mitral regurgitation, tricuspid regurgitation (with normal right ventricular (RV) pressures) and ventricular septal defect (VSD). -

12 ACE (Angiotensin-Converting Enzyme)
Index Ablation, radiofrequency, 58–59 Antihypertensive and Lipid Ablative therapy, 65–66 Lowering Treatment to Accupril (quinapril), 12 Prevent Heart Attack Trial ACE (angiotensin-converting (ALLHAT), 18 enzyme) inhibitors, 7 Antihypertensive drug classes, Acebutolol (Sectral), 13, 61 7–18 Aceon (perindopril), 13 Antihypertensive drug selection, Adalat Procardia (nifedipine), 14 19–20 Adenocard (adenosine), 64 Antihypertensive drugs, 12–16 Adenosine (Adenocard), 64 Antiplatelet therapy, 40 Adolescents Aortic insufficiency, 98–99 sudden cardiac death in, 218–219 Aortic stenosis, 105–107 syncope in, 213 Aspirin Alcohol, 158 angina pectoris and, 36 Aldactone (spironolactone), 16 low-dose, 188 Aldomet (methyldopa), 15 Atenolol (Tenormin), 13, 61 ab-blockers, 15 Atherosclerosis, 186–187 a1-blockers, 14, 17 premature, 148–149 Altace (ramipril), 13 Athletes Amiloride (Midamor), 15 murmurs in, 111–112 Amiodarone (Cordarone), 63 sudden cardiac death in, 219–220 Amlodipine (Norvasc), 14 Atorvastatin (Lipitor), 163 Aneurysm, 196–197 Atrial fibrillation, 191–192, 76–80 Angina pectoris, 27–28, 32–41 Atrial flutter, 80–81 aspirin and, 36 Atrial premature beats, 70 unstable, 36–41 Atrial tachycardia, 73 Angiotensin-converting enzyme Atrioventricular (AV) nodal (ACE) inhibitors, 7 reentrant tachycardias, 74–75 Angiotensin receptor antagonists, Atrioventricular node, 53 9 Atrioventricular reciprocating Ankle-brachial index, 282 tachycardias, 75–76 Antiadrenergic agents, 11–18 Austin Flint murmur, 104 Antiarrhythmic drugs, 59–65 AV, see Atrioventricular -

Ministry of Health of Ukraine Kharkiv National Medical University
Ministry of Health of Ukraine Kharkiv National Medical University AUSCULTATION OF THE HEART. NORMAL HEART SOUNDS, REDUPLICATION OF THE SOUNDS, ADDITIONAL SOUNDS (TRIPLE RHYTHM, GALLOP RHYTHM), ORGANIC AND FUNCTIONAL HEART MURMURS Methodical instructions for students Рекомендовано Ученым советом ХНМУ Протокол №__от_______2017 г. Kharkiv KhNMU 2017 Auscultation of the heart. normal heart sounds, reduplication of the sounds, additional sounds (triple rhythm, gallop rhythm), organic and functional heart murmurs / Authors: Т.V. Ashcheulova, O.M. Kovalyova, O.V. Honchar. – Kharkiv: KhNMU, 2017. – 20 с. Authors: Т.V. Ashcheulova O.M. Kovalyova O.V. Honchar AUSCULTATION OF THE HEART To understand the underlying mechanisms contributing to the cardiac tones formation, it is necessary to remember the sequence of myocardial and valvular action during the cardiac cycle. During ventricular systole: 1. Asynchronous contraction, when separate areas of myocardial wall start to contract and intraventricular pressure rises. 2. Isometric contraction, when the main part of the ventricular myocardium contracts, atrioventricular valves close, and intraventricular pressure significantly increases. 3. The ejection phase, when the intraventricular pressure reaches the pressure in the main vessels, and the semilunar valves open. During diastole (ventricular relaxation): 1. Closure of semilunar valves. 2. Isometric relaxation – initial relaxation of ventricular myocardium, with atrioventricular and semilunar valves closed, until the pressure in the ventricles becomes lower than in the atria. 3. Phases of fast and slow ventricular filling - atrioventricular valves open and blood flows from the atria to the ventricles. 4. Atrial systole, after which cardiac cycle repeats again. The noise produced By a working heart is called heart sounds. In auscultation two sounds can be well heard in healthy subjects: the first sound (S1), which is produced during systole, and the second sound (S2), which occurs during diastole.