Interstitial Incisional Hernia Following Appendectomy: a Case Report
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

Utility of the Digital Rectal Examination in the Emergency Department: a Review
The Journal of Emergency Medicine, Vol. 43, No. 6, pp. 1196–1204, 2012 Published by Elsevier Inc. Printed in the USA 0736-4679/$ - see front matter http://dx.doi.org/10.1016/j.jemermed.2012.06.015 Clinical Reviews UTILITY OF THE DIGITAL RECTAL EXAMINATION IN THE EMERGENCY DEPARTMENT: A REVIEW Chad Kessler, MD, MHPE*† and Stephen J. Bauer, MD† *Department of Emergency Medicine, Jesse Brown VA Medical Center and †University of Illinois-Chicago College of Medicine, Chicago, Illinois Reprint Address: Chad Kessler, MD, MHPE, Department of Emergency Medicine, Jesse Brown Veterans Hospital, 820 S Damen Ave., M/C 111, Chicago, IL 60612 , Abstract—Background: The digital rectal examination abdominal pain and acute appendicitis. Stool obtained by (DRE) has been reflexively performed to evaluate common DRE doesn’t seem to increase the false-positive rate of chief complaints in the Emergency Department without FOBTs, and the DRE correlated moderately well with anal knowing its true utility in diagnosis. Objective: Medical lit- manometric measurements in determining anal sphincter erature databases were searched for the most relevant arti- tone. Published by Elsevier Inc. cles pertaining to: the utility of the DRE in evaluating abdominal pain and acute appendicitis, the false-positive , Keywords—digital rectal; utility; review; Emergency rate of fecal occult blood tests (FOBT) from stool obtained Department; evidence-based medicine by DRE or spontaneous passage, and the correlation be- tween DRE and anal manometry in determining anal tone. Discussion: Sixteen articles met our inclusion criteria; there INTRODUCTION were two for abdominal pain, five for appendicitis, six for anal tone, and three for fecal occult blood. -

The Differences Between ICD-9 and ICD-10
Preparing for the ICD-10 Code Set: Fact Sheet 2 October 1, 2015 Compliance Date Get the Facts to be Compliant Alert: The new ICD-10 compliance date is October 1, 2015. The Differences Between ICD-9 and ICD-10 This is the second fact sheet in a series and is focused on the differences between the ICD-9 and ICD-10 code sets. Collectively, the fact sheets will provide information, guidance, and checklists to assist you with understanding what you need to do to implement the ICD-10 code set. The ICD-10 code sets are not a simple update of the ICD-9 code set. The ICD-10 code sets have fundamental changes in structure and concepts that make them very different from ICD-9. Because of these differences, it is important to develop a preliminary understanding of the changes from ICD-9 to ICD-10. This basic understanding of the differences will then identify more detailed training that will be needed to appropriately use the ICD-10 code sets. In addition, seeing the differences between the code sets will raise awareness of the complexities of converting to the ICD-10 codes. Overall Comparisons of ICD-9 to ICD-10 Issues today with the ICD-9 diagnosis and procedure code sets are addressed in ICD-10. One concern today with ICD-9 is the lack of specificity of the information conveyed in the codes. For example, if a patient is seen for treatment of a burn on the right arm, the ICD-9 diagnosis code does not distinguish that the burn is on the right arm. -
Appendectomy: Simple Appendicitis
Appendectomy: Simple Appendicitis Your child has had an appendectomy (ap pen DECK toe mee). This is the surgical removal of the appendix. The appendix is a small, narrow sac at the beginning of the large intestine (Picture 1). The appendix has no known function. What to Expect After Surgery . Your child will awaken in the Post Anesthesia Care Unit (PACU) near the surgery area. He or she may be in the PACU for 1 to 2 hours. After your child wakes up in the PACU, he or she will return to a hospital room or be Esophagus transferred to the Surgery Unit. Discharge will be directly from the Surgery Unit. Liver Stomach . Your child will have 3 to 4 small incision Large sites (see Helping Hand HH-I-283, Intestines Laparoscopic Surgery (colon) ). Small . Your child will receive fluids and pain intestines medicine through an intravenous line (IV). Rectum When your child can take liquids by mouth, pain medicine will also be given by mouth. Appendix . Your child will need to cough and deep-breathe often to help keep the lungs clear. He or she may use a plastic device called an incentive Picture 1 The appendix inside the body. spirometer to help with this. Your child will need to get up and walk soon after surgery. Walking will help "wake up" the bowels; it will also help with breathing and blood flow. Your child will be able to go home on the same day of the surgery if he or she is: o able to drink clear liquids like water, clear soft drinks, broth, and fruit punch o taking pain medicine by mouth and his or her pain is controlled, and o able to walk. -

Small Bowel Diseases Requiring Emergency Surgical Intervention
GÜSBD 2017; 6(2): 83 -89 Gümüşhane Üniversitesi Sağlık Bilimleri Dergisi Derleme GUSBD 2017; 6(2): 83 -89 Gümüşhane University Journal Of Health Sciences Review SMALL BOWEL DISEASES REQUIRING EMERGENCY SURGICAL INTERVENTION ACİL CERRAHİ GİRİŞİM GEREKTİREN İNCE BARSAK HASTALIKLARI Erdal UYSAL1, Hasan BAKIR1, Ahmet GÜRER2, Başar AKSOY1 ABSTRACT ÖZET In our study, it was aimed to determine the main Çalışmamızda cerrahların günlük pratiklerinde, ince indications requiring emergency surgical interventions in barsakta acil cerrahi girişim gerektiren ana endikasyonları small intestines in daily practices of surgeons, and to belirlemek, literatür desteğinde verileri analiz etmek analyze the data in parallel with the literature. 127 patients, amaçlanmıştır. Merkezimizde ince barsak hastalığı who underwent emergency surgical intervention in our nedeniyle acil cerrahi girişim uygulanan 127 hasta center due to small intestinal disease, were involved in this çalışmaya alınmıştır. Hastaların dosya ve bilgisayar kayıtları study. The data were obtained by retrospectively examining retrospektif olarak incelenerek veriler elde edilmiştir. the files and computer records of the patients. Of the Hastaların demografik özellikleri, tanıları, yapılan cerrahi patients, demographical characteristics, diagnoses, girişimler ve mortalite parametreleri kayıt altına alındı. performed emergency surgical interventions, and mortality Elektif opere edilen hastalar ve izole incebarsak hastalığı parameters were recorded. The electively operated patients olmayan hastalar çalışma dışı bırakıldı Rakamsal and those having no insulated small intestinal disease were değişkenler ise ortalama±standart sapma olarak verildi. excluded. The numeric variables are expressed as mean ±standard deviation.The mean age of patients was 50.3±19.2 Hastaların ortalama yaşları 50.3±19.2 idi. Kadın erkek years. The portion of females to males was 0.58. -

Nia Repair - the Role of Mesh Hernia Forms
Frezza EE, et al., J Gastroenterol Hepatology Res 2017, 2: 008 DOI: 10.24966/GHR-2566/100008 HSOA Journal of Gastroenterology & Hepatology Research Research Article tients were reoperated for removal of midline skin changes, two for Component Separation or severe seromas requiring wash up of the subcutaneous and fascia area and placement of a wound vacuum on top of the mesh. Mesh Repair for Ventral Her- Conclusion: This study supports the notion that a ventral hernia reflects a defect in the abdominal wall not just the point at which the nia Repair - The Role of Mesh hernia forms. To avoid a point of rupture, we support highly the CSR technique, since hernia is an abdominal disease not just a hole. in Covering all the Abdominal Keywords: Abdominal wall physiology; Biological mesh; Compo- nent separation; Cross sectional area; Elastic force; Phasix mesh; Wall in the Component Repair Polypropylene mesh; Tensile force; Ventral hernia; Ventral hernia Eldo E Frezza1*, Cory Cogdill2, Mitchell Wacthell3 and Edoar- repair do GP Frezza4 1Eastern New Mexico University, Health Science Center, Roswell NM, USA Introduction 2Mathematics, Physics and Science Department, Eastern New Mexico The correction of abdominal wall hernias has presented a surgical University, Roswell NM, USA challenge for decades. Simple repair of the hernia opening, Ventral 3Texas Tech University, Lubbock TX, USA Hernia Repair (VHR), has been confronted by a more definitive goal 4University of Delaware, Newark DE, USA of restoration of abdominal muscular strength and wall function, ac- complished by mobilizing abdominal wall muscles and closing with inlay mesh, Component Separation Repair (CSR) [1]. CSR mobilizes fresh muscle medially to reinforce the region of herniation, while pre- serving fascia associated muscle, and fascia of the rectus muscle, with closure at the line a alba [1]. -

Ventral Hernia Repair
AMERICAN COLLEGE OF SURGEONS • DIVISION OF EDUCATION Ventral Hernia Repair Benefits and Risks of Your Operation Patient Education B e n e fi t s — An operation is the only This educational information is way to repair a hernia. You can return to help you be better informed to your normal activities and, in most about your operation and cases, will not have further discomfort. empower you with the skills and Risks of not having an operation— knowledge needed to actively The size of your hernia and the pain it participate in your care. causes can increase. If your intestine becomes trapped in the hernia pouch, you will have sudden pain and vomiting Keeping You Common Sites for Ventral Hernia and require an immediate operation. Informed If you decide to have the operation, Information that will help you possible risks include return of the further understand your operation The Condition hernia; infection; injury to the bladder, and your role in healing. A ventral hernia is a bulge through blood vessels, or intestines; and an opening in the muscles on the continued pain at the hernia site. Education is provided on: abdomen. The hernia can occur at a Hernia Repair Overview .................1 past incision site (incisional), above the navel (epigastric), or other weak Condition, Symptoms, Tests .........2 Expectations muscle sites (primary abdominal). Treatment Options….. ....................3 Before your operation—Evaluation may include blood work, urinalysis, Risks and Common Symptoms Possible Complications ..................4 ultrasound, or a CT scan. Your surgeon ● Visible bulge on the abdomen, and anesthesia provider will review Preparation especially with coughing or straining your health history, home medications, and Expectations .............................5 ● Pain or pressure at the hernia site and pain control options. -
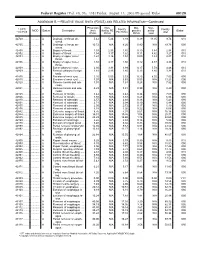
RELATIVE VALUE UNITS (RVUS) and RELATED INFORMATION—Continued
Federal Register / Vol. 68, No. 158 / Friday, August 15, 2003 / Proposed Rules 49129 ADDENDUM B.—RELATIVE VALUE UNITS (RVUS) AND RELATED INFORMATION—Continued Physician Non- Mal- Non- 1 CPT/ Facility Facility 2 MOD Status Description work facility PE practice acility Global HCPCS RVUs RVUs PE RVUs RVUs total total 42720 ....... ........... A Drainage of throat ab- 5.42 5.24 3.93 0.39 11.05 9.74 010 scess. 42725 ....... ........... A Drainage of throat ab- 10.72 N/A 8.26 0.80 N/A 19.78 090 scess. 42800 ....... ........... A Biopsy of throat ................ 1.39 2.35 1.45 0.10 3.84 2.94 010 42802 ....... ........... A Biopsy of throat ................ 1.54 3.17 1.62 0.11 4.82 3.27 010 42804 ....... ........... A Biopsy of upper nose/ 1.24 3.16 1.54 0.09 4.49 2.87 010 throat. 42806 ....... ........... A Biopsy of upper nose/ 1.58 3.17 1.66 0.12 4.87 3.36 010 throat. 42808 ....... ........... A Excise pharynx lesion ...... 2.30 3.31 1.99 0.17 5.78 4.46 010 42809 ....... ........... A Remove pharynx foreign 1.81 2.46 1.40 0.13 4.40 3.34 010 body. 42810 ....... ........... A Excision of neck cyst ........ 3.25 5.05 3.53 0.25 8.55 7.03 090 42815 ....... ........... A Excision of neck cyst ........ 7.07 N/A 5.63 0.53 N/A 13.23 090 42820 ....... ........... A Remove tonsils and ade- 3.91 N/A 3.63 0.28 N/A 7.82 090 noids. -

Incidental Drainage of a Periappendicular Abscess During Colonoscopy
UCTN – Unusual cases and technical notes E175 Incidental drainage of a periappendicular abscess during colonoscopy A 50-year-old man was referred to the of oral metronidazole and ciprofloxacin. A P. Figueiredo, V. Fernandes, J. Freitas outpatient colonoscopy clinic after a posi- computed tomography (CT) scan 1 week Department of Gastroenterology, tive fecal occult blood test during screen- after the procedure revealed no abnormal Hospital Garcia de Orta, Almada, Portugal ing for colorectal cancer. Colonoscopy, findings and the patient remained asymp- which was performed with the patient tomatic. sedated, revealed a 12-mm tumor covered Acute appendicitis is the most frequent References by normal, smooth mucosa at the site of acute abdominal emergency seen in de- 1 Oliak D, Yamini D, Udani VM et al. Can per- forated appendicitis be diagnosed preopera- the appendicular orifice. A biopsy was veloped countries. Its most common com- tively based on admission factors? J Gastro- taken, but this led to an immediate puru- plication is perforation and this may be intest Surg 2000; 4: 470–474 lent discharge occurring from the lesion followed by abscess formation [1]. Colo- 2 Ohtaka M, Asakawa A, Kashiwagi A et al. (●" Video 1). Therefore, a diagnosis of a noscopic diagnosis and treatment of a Pericecal appendiceal abscess with drainage periappendicular abscess was incidentally periappendicular abscess is rare [2]. In during colonoscopy. Gastrointest Endosc 1999; 49: 107–109 established. this case a periappendicular abscess was 3 Antevil J, Brown C. Percutaneous drainage After the patient had recovered from the incidentally discovered and drained dur- and interval appendectomy. In: Scott-Turner sedation, he was specifically questioned ing a colonoscopy. -

Immune Functions of the Vermiform Appendix
The Proceedings of the International Conference on Creationism Volume 3 Print Reference: Pages 335-342 Article 30 1994 Immune Functions of the Vermiform Appendix Frank Maas Follow this and additional works at: https://digitalcommons.cedarville.edu/icc_proceedings DigitalCommons@Cedarville provides a publication platform for fully open access journals, which means that all articles are available on the Internet to all users immediately upon publication. However, the opinions and sentiments expressed by the authors of articles published in our journals do not necessarily indicate the endorsement or reflect the views of DigitalCommons@Cedarville, the Centennial Library, or Cedarville University and its employees. The authors are solely responsible for the content of their work. Please address questions to [email protected]. Browse the contents of this volume of The Proceedings of the International Conference on Creationism. Recommended Citation Maas, Frank (1994) "Immune Functions of the Vermiform Appendix," The Proceedings of the International Conference on Creationism: Vol. 3 , Article 30. Available at: https://digitalcommons.cedarville.edu/icc_proceedings/vol3/iss1/30 IMMUNE FUNCTIONS OF THE VERMIFORM APPENDIX FRANK MAAS, M.S. 320 7TH STREET GERVAIS, OR 97026 KEYWORDS Mucosal immunology, gut-associated lymphoid tissues. immunocompetence, appendix (human and rabbit), appendectomy, neoplasm, vestigial organs. ABSTRACT The vermiform appendix Is purported to be the classic example of a vestigial organ, yet for nearly a century it has been known to be a specialized organ highly infiltrated with lymphoid tissue. This lymphoid tissue may help protect against local gut infections. As the vertebrate taxonomic scale increases, the lymphoid tissue of the large bowel tends to be concentrated In a specific region of the gut: the cecal apex or vermiform appendix. -
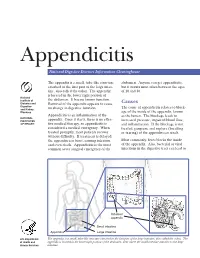
Appendicitis
Appendicitis National Digestive Diseases Information Clearinghouse The appendix is a small, tube-like structure abdomen. Anyone can get appendicitis, attached to the first part of the large intes- but it occurs most often between the ages tine, also called the colon. The appendix of 10 and 30. is located in the lower right portion of National Institute of the abdomen. It has no known function. Diabetes and Removal of the appendix appears to cause Causes Digestive The cause of appendicitis relates to block- and Kidney no change in digestive function. Diseases age of the inside of the appendix, known Appendicitis is an inflammation of the as the lumen. The blockage leads to NATIONAL INSTITUTES appendix. Once it starts, there is no effec- increased pressure, impaired blood flow, OF HEALTH tive medical therapy, so appendicitis is and inflammation. If the blockage is not considered a medical emergency. When treated, gangrene and rupture (breaking treated promptly, most patients recover or tearing) of the appendix can result. without difficulty. If treatment is delayed, the appendix can burst, causing infection Most commonly, feces blocks the inside and even death. Appendicitis is the most of the appendix. Also, bacterial or viral common acute surgical emergency of the infections in the digestive tract can lead to Inflamed appendix Small intestine Appendix Large intestine U.S. Department The appendix is a small, tube-like structure attached to the first part of the large intestine, also called the colon. The of Health and appendix is located in the lower right portion of the abdomen, near where the small intestine attaches to the large Human Services intestine. -

The Modern Management of Incisional Hernias
CLINICAL REVIEW The modern management of Follow the link from the online version of this article to obtain certi ed continuing medical education credits incisional hernias David L Sanders,1 Andrew N Kingsnorth2 1Upper Gastrointestinal Surgery, Before the introduction of general anaesthesia by Morton of different tissue properties in constant motion has to be Royal Cornwall Hospital, Truro TR1 in 1846, incisional hernias were rare. As survival after sutured; positive abdominal pressure has to be dealt with; 3LJ, UK 2 abdominal surgery became more common so did the and tissues with impaired healing properties, reduced Peninsula College of Medicine and 1 Dentistry, Plymouth, UK incidence of incisional hernias. Since then, more than perfusion, and connective tissue deficiencies have to be Correspondence to: D L Sanders 4000 peer reviewed articles have been published on the joined. [email protected] topic, many of which have introduced a new or modified This review, which is targeted at the general medical Cite this as: BMJ 2012;344:e2843 surgical technique for prevention and repair. Despite audience, aims to update the reader on the definition, doi: 10.1136/bmj.e2843 considerable improvements in prosthetics used for her- incidence, risk factors, diagnosis, and management of nia surgery, the incidence of incisional hernias and the incisional hernias. recurrence rates after repair remain high. Arguably, no other benign disease has seen so little improvement in Unravelling the terminology terms of surgical outcome. Despite the size of the problem, the terminology used to Unlike other abdominal wall hernias, which occur describe incisional hernias still varies greatly. An inter- through anatomical points of weakness, incisional her- nationally acceptable and uniform definition is needed to nias occur through a weakness at the site of abdominal improve the clarity of communication within the medical wall closure. -

Incisional Hernia After Peritoneal Dialysis Catheter Placement in a Patient Simratdeep Sandhu,1 Richard Dickerman,2 Bruce Smith,3 Anupkumar Shetty1,2 on Sirolimus
Advances in Peritoneal Dialysis, Vol. 33, 2017 Incisional Hernia After Peritoneal Dialysis Catheter Placement in a Patient Simratdeep Sandhu,1 Richard Dickerman,2 Bruce Smith,3 Anupkumar Shetty1,2 on Sirolimus Hernias and peritoneal dialysis (PD) catheter leaks stopped the mycophenolate sodium on his own, and we are frequent complications in patients on PD. Trans- did not resume it. He is still on low-dose prednisone. plant recipients have multiple risk factors for delayed In end-stage renal disease resulting from failing wound healing, such as use of corticosteroids and renal transplantation or from calcineurin inhibitor sirolimus, and the presence of uremia and diabetes nephropathy in solid-organ transplantation, sirolimus mellitus. We report a rare occurrence of incisional is a risk factor for wound dehiscence, development of hernia attributable to internal wound dehiscence incisional hernia, and peritoneal dialysate leak. after PD catheter placement in a patient on sirolimus. Practical tips: Sirolimus should be stopped several A 34-year-old Latino American man was started on days before PD catheter placement. Sirolimus should PD training 4 weeks after placement of a PD catheter. also be stopped if a PD catheter leak is detected or Soon after completing training, he developed a large if incisional hernia develops soon after initiation of soft bulge close to the PD catheter, with expansile PD. Sirolimus should be held till surgical repair of the cough impulse suggestive of an incisional hernia filled hernia and removal and replacement of the catheter. with peritoneal dialysate. The size of the bulge would decrease after the dialysate was drained. No external Key words leak of dialysate was evident along the exit site.