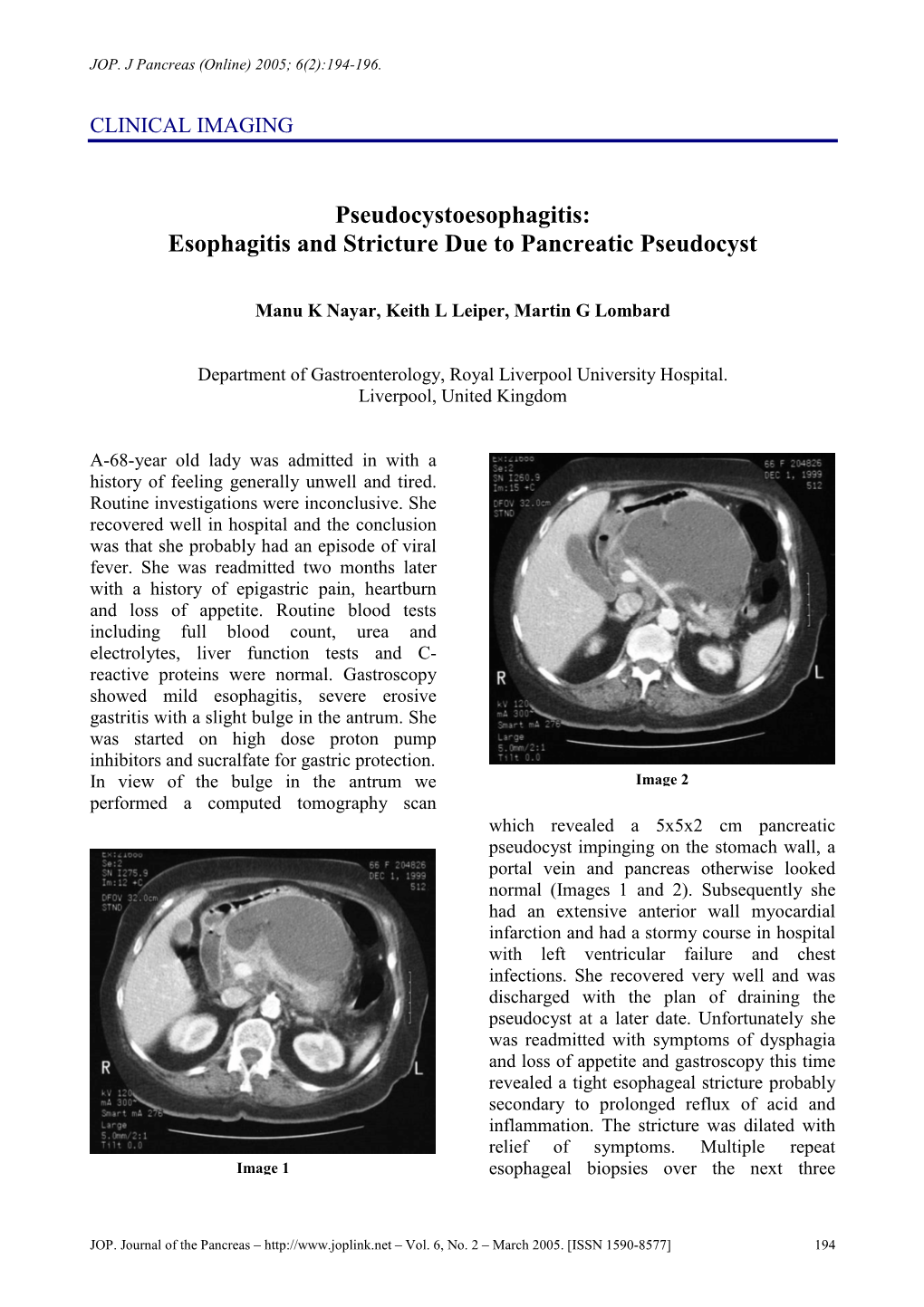
Esophagitis and Stricture Due to Pancreatic Pseudocyst
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dyspepsia (Indigestion)
Indigestion (dydpepsia). Indigestion information - Patient | Patient Page 1 of 5 View this article online at https://patient.info/health/dyspepsia-indigestion Dyspepsia (Indigestion) Dyspepsia (indigestion) is a term which describes pain and sometimes other symptoms which come from your upper gut (the stomach, oesophagus or duodenum). There are various causes (described below). Treatment depends on the likely cause. Understanding digestion Food passes down the gullet (oesophagus) into the stomach. The stomach makes acid which is not essential but helps to digest food. Food then passes gradually into the first part of the small intestine (the duodenum). In the duodenum and the rest of the small intestine, food mixes with chemicals called enzymes. The enzymes come from the pancreas and from cells lining the intestine. The enzymes break down (digest) the food. Digested food is then absorbed into the body from the small intestine. What is dyspepsia? Dyspepsia is a term which includes a group of symptoms that come from a problem in your upper gut. The gut (gastrointestinal tract) is the tube that starts at the mouth and ends at the anus. The upper gut includes the oesophagus, stomach and duodenum. Various conditions cause dyspepsia. The main symptom is usually pain or discomfort in the upper tummy (abdomen). In addition, other symptoms that may develop include: • Bloating. • Belching. • Quickly feeling full after eating. • Feeling sick (nausea). • Being sick (vomiting). Symptoms are often related to eating. Doctors used to include heartburn (a burning sensation felt in the lower chest area) and bitter-tasting liquid coming up into the back of the throat (sometimes called 'waterbrash') as symptoms of dyspepsia. -

Non-Alcoholic Steatohepatitis (NASH) in Non-Obese Children
Tropical Gastroenterology 2016;37(2):133-135 133 collection then follow the path along the lesser omentum References or gastrohepatic ligament toward the liver leading to the formation of left lobe subcapsular collections. Second 1. Mofredj A, Cadranel JF, Dautreaux Met al. Pancreatic mechanism, likely in our second case, is tracking of pseudocyst located in the liver: a case report and literature review. J Clin Gastroenterol. 2000;30:813. pancreatic juice along the hepatoduodenal ligament 2. Okuda K, Sugita S, Tsukada E, Sakuma Yet al. Pancreatic from the head of pancreas to the portahepatis resulting pseudocyst in the left hepatic lobe: a report of two cases. in formation of intrahepatic parenchymal collections. Hepatology. 1991;13:359-63. Pseudocysts, which form as per the first mechanism, 3. Kralik J, Pesula E. A pancreatic pseudocyst in the liver. are mainly subcapsular in location and are biconvex in Rozhl Chir. 1993;72:913. shape. Intra parenchymal pseudocysts formed as a result 4. Bhasin DK, Rana SS, Chandail VS et al. An intrahepatic pancreatic pseudocyst successfully treated endoscopic of the second mechanism are located away from the liver transpapillary drainage alone. JOP. 2005;6:5937. capsule and are located near branches of porta hepatis. 5. Atia A, Kalra S, Rogers M et al. A wayward cyst. JOP. J Intrahepatic pseudocysts pose a diagnostic challenge Pancreas (Online) 2009;10:4214. because they are rarely considered in the differential diagnosis of cystic hepatic lesions. Amylase rich fluid on aspiration and communication of pseudocyst with disrupted pancreatic duct on imaging is indicative of diagnosis. However, neither of pseudocysts in our two Non-alcoholic steatohepatitis cases had communication with pancreatic duct. -

Abdominal Pain - Gastroesophageal Reflux Disease
ACS/ASE Medical Student Core Curriculum Abdominal Pain - Gastroesophageal Reflux Disease ABDOMINAL PAIN - GASTROESOPHAGEAL REFLUX DISEASE Epidemiology and Pathophysiology Gastroesophageal reflux disease (GERD) is one of the most commonly encountered benign foregut disorders. Approximately 20-40% of adults in the United States experience chronic GERD symptoms, and these rates are rising rapidly. GERD is the most common gastrointestinal-related disorder that is managed in outpatient primary care clinics. GERD is defined as a condition which develops when stomach contents reflux into the esophagus causing bothersome symptoms and/or complications. Mechanical failure of the antireflux mechanism is considered the cause of GERD. Mechanical failure can be secondary to functional defects of the lower esophageal sphincter or anatomic defects that result from a hiatal or paraesophageal hernia. These defects can include widening of the diaphragmatic hiatus, disturbance of the angle of His, loss of the gastroesophageal flap valve, displacement of lower esophageal sphincter into the chest, and/or failure of the phrenoesophageal membrane. Symptoms, however, can be accentuated by a variety of factors including dietary habits, eating behaviors, obesity, pregnancy, medications, delayed gastric emptying, altered esophageal mucosal resistance, and/or impaired esophageal clearance. Signs and Symptoms Typical GERD symptoms include heartburn, regurgitation, dysphagia, excessive eructation, and epigastric pain. Patients can also present with extra-esophageal symptoms including cough, hoarse voice, sore throat, and/or globus. GERD can present with a wide spectrum of disease severity ranging from mild, intermittent symptoms to severe, daily symptoms with associated esophageal and/or airway damage. For example, severe GERD can contribute to shortness of breath, worsening asthma, and/or recurrent aspiration pneumonia. -
Pancreatic Disorders in Inflammatory Bowel Disease
Submit a Manuscript: http://www.wjgnet.com/esps/ World J Gastrointest Pathophysiol 2016 August 15; 7(3): 276-282 Help Desk: http://www.wjgnet.com/esps/helpdesk.aspx ISSN 2150-5330 (online) DOI: 10.4291/wjgp.v7.i3.276 © 2016 Baishideng Publishing Group Inc. All rights reserved. MINIREVIEWS Pancreatic disorders in inflammatory bowel disease Filippo Antonini, Raffaele Pezzilli, Lucia Angelelli, Giampiero Macarri Filippo Antonini, Giampiero Macarri, Department of Gastro- acute pancreatitis or chronic pancreatitis has been rec enterology, A.Murri Hospital, Polytechnic University of Marche, orded in patients with inflammatory bowel disease (IBD) 63900 Fermo, Italy compared to the general population. Although most of the pancreatitis in patients with IBD seem to be related to Raffaele Pezzilli, Department of Digestive Diseases and Internal biliary lithiasis or drug induced, in some cases pancreatitis Medicine, Sant’Orsola-Malpighi Hospital, 40138 Bologna, Italy were defined as idiopathic, suggesting a direct pancreatic Lucia Angelelli, Medical Oncology, Mazzoni Hospital, 63100 damage in IBD. Pancreatitis and IBD may have similar Ascoli Piceno, Italy presentation therefore a pancreatic disease could not be recognized in patients with Crohn’s disease and ulcerative Author contributions: Antonini F designed the research; Antonini colitis. This review will discuss the most common F and Pezzilli R did the data collection and analyzed the data; pancreatic diseases seen in patients with IBD. Antonini F, Pezzilli R and Angelelli L wrote the paper; Macarri G revised the paper and granted the final approval. Key words: Pancreas; Pancreatitis; Extraintestinal mani festations; Exocrine pancreatic insufficiency; Ulcerative Conflictofinterest statement: The authors declare no conflict colitis; Crohn’s disease; Inflammatory bowel disease of interest. -

Necrotizing Pancreatitis and Gas Forming Organisms
JOP. J Pancreas (Online) 2016 Nov 08; 17(6):649-652. CASE REPORT Necrotizing Pancreatitis and Gas Forming Organisms Theadore Hufford, Terrence Lerner Metropolitan Group Hospitals Residency in General Surgery, University of Illinois, United States ABSTRACT Context Acute Pancreatitis is a common disease of the gastrointestinal tract that accounts for thousands of hospital admissions in the United States every year. Severe acute necrotic pancreatitis has a high mortality rate if left untreated, and always requires surgical intervention. The timing of surgical intervention is of importance. Here we present a case of a patient with severe necrotizing pancreatitis with possible gas producing bacteria in the retroperitoneum shown on imaging and cultures. Case Report The patient is a Seventy- two-year old male presenting to the emergency department with complaining of severe epigastric pain for the past 48 hours. The labs and clinical symptoms were consistent with pancreatitis. However, the imaging showed necrotic pancreatitis that required immediate intervention. During the course of six weeks, the patient underwent numerous surgical procedures to debride the necrotic pancreas. The patient was ultimately clinically stable to be discharged and transferred to a skilled-nursing facility, but returned 3 days later with a post- surgical wound infection vs. Conclusion The patient ultimately expired 7 days after his second admission to the hospital due to multi-organ failure secondary to sepsis. anastomotic leak with enterocutaneous fistula. INTRODUCTION has proven to decrease mortality by about 40% in most cases [6]. Finding the cause of the infection is of the Acute Pancreatitis (AP) is a common disease of the utmost importance in necrotizing pancreatitis cases. -

Gastritis - Symptoms and Causes - Mayo Clinic Visited 11/22/2019
Gastritis - Symptoms and causes - Mayo Clinic Visited 11/22/2019 Request an Appointment Find a Doctor MENU Find a Job Give Now Log in to Patient Account English Patient Care & Health Information Diseases & Conditions Request an Gastritis Appointment Symptoms & causes Diagnosis & treatment Doctors & departments Overview Print Advertisement Gastritis is a general term for a group Mayo Clinic does not endorse companies or of conditions with one thing in common: products. Advertising revenue supports our not- inflammation of the lining of the for-profit mission. stomach. The inflammation of gastritis Advertising & Sponsorship is most often the result of infection with Policy Opportunities Ad Choices the same bacterium that causes most stomach ulcers. Regular use of certain Stomach and pain relievers and drinking too much pyloric valve Mayo Clinic Marketplace alcohol also can contribute to gastritis. Check out these best-sellers and special offers on books and newsletters from Mayo Clinic. Gastritis may occur suddenly (acute gastritis), or appear slowly over time (chronic gastritis). In some cases, gastritis NEW – Guide to Fibromyalgia can lead to ulcers and an increased risk of stomach cancer. Instant access – Mayo Clinic Health Letter For most people, however, gastritis isn't serious and improves quickly with treatment. Diabetes? This diet works … Stop osteoporosis in its tracks The Mayo Clinic Diet Online Products & Services Book: Mayo Clinic on Digestive Health https://www.mayoclinic.org/diseases-conditions/gastritis/symptoms-causes/syc-20355807[11/22/2019 4:16:25 PM] Gastritis - Symptoms and causes - Mayo Clinic Visited 11/22/2019 Symptoms The signs and symptoms of gastritis include: Gnawing or burning ache or pain (indigestion) in your upper abdomen that may become either worse or better with eating Nausea Vomiting A feeling of fullness in your upper abdomen after eating Gastritis doesn't always cause signs and symptoms. -

Gastroesophageal Reflux Disease (GERD)
Guidelines for Clinical Care Quality Department Ambulatory GERD Gastroesophageal Reflux Disease (GERD) Guideline Team Team Leader Patient population: Adults Joel J Heidelbaugh, MD Objective: To implement a cost-effective and evidence-based strategy for the diagnosis and Family Medicine treatment of gastroesophageal reflux disease (GERD). Team Members Key Points: R Van Harrison, PhD Diagnosis Learning Health Sciences Mark A McQuillan, MD History. If classic symptoms of heartburn and acid regurgitation dominate a patient’s history, then General Medicine they can help establish the diagnosis of GERD with sufficiently high specificity, although sensitivity Timothy T Nostrant, MD remains low compared to 24-hour pH monitoring. The presence of atypical symptoms (Table 1), Gastroenterology although common, cannot sufficiently support the clinical diagnosis of GERD [B*]. Testing. No gold standard exists for the diagnosis of GERD [A*]. Although 24-hour pH monitoring Initial Release is accepted as the standard with a sensitivity of 85% and specificity of 95%, false positives and false March 2002 negatives still exist [II B*]. Endoscopy lacks sensitivity in determining pathologic reflux but can Most Recent Major Update identify complications (eg, strictures, erosive esophagitis, Barrett’s esophagus) [I A]. Barium May 2012 radiography has limited usefulness in the diagnosis of GERD and is not recommended [III B*]. Content Reviewed Therapeutic trial. An empiric trial of anti-secretory therapy can identify patients with GERD who March 2018 lack alarm or warning symptoms (Table 2) [I A*] and may be helpful in the evaluation of those with atypical manifestations of GERD, specifically non-cardiac chest pain [II B*]. Treatment Ambulatory Clinical Lifestyle modifications. -

The Clinical Analysis of Acute Pancreatitis in Colorectal Cancer Patients Undergoing Chemotherapy After Operation
Journal name: OncoTargets and Therapy Article Designation: Original Research Year: 2015 Volume: 8 OncoTargets and Therapy Dovepress Running head verso: Ji et al Running head recto: Analysis of acute pancreatitis in colorectal cancer patients open access to scientific and medical research DOI: http://dx.doi.org/10.2147/OTT.S88857 Open Access Full Text Article ORIGINAL RESEARCH The clinical analysis of acute pancreatitis in colorectal cancer patients undergoing chemotherapy after operation Yanlei Ji1 Abstract: Acute pancreatitis is a rare complication in postoperative colorectal cancer patients Zhen Han2 after FOLFOX6 (oxaliplatin + calcium folinate +5-FU [5-fluorouracil]) chemotherapy. In this Limei Shao1 paper, a total of 62 patients with gastrointestinal cancer were observed after the burst of acute Yunling Li1 pancreatitis. Surgery of the 62 cases of colorectal cancer patients was completed successfully. Long Zhao1 But when they underwent FOLFOX6 chemotherapy, five patients got acute pancreatitis (8.06%), Yuehuan Zhao1 four (6.45%) had mild acute pancreatitis, and one (1.61%) had severe acute pancreatitis, of which two were males (3.23%) and three females (4.84%). No patients (0.00%) had acute pancreatitis 1 Department of Special Diagnosis, on the 1st day after chemotherapy; one patient (1.61%) got it in the first 2 and 3 days after Shandong Cancer Hospital and Institute, Jinan, People’s Republic chemotherapy; and three others (4.83%) got it in the first 4 days after chemotherapy. In the 2 For personal use only. of China; Department of Internal 62 patients with malignant tumors, the body mass index (BMI) was less than 18 (underweight) in Medicine, Jinan Second People’s six of them, with two cases of acute pancreatitis (33.33%); the BMI was 18–25 (normal weight) Hospital, Jinan, People’s Republic of China in 34 cases, with one case (2.94%) of acute pancreatitis; the BMI was 25–30 (overweight) in 13 cases, with 0 cases (0.00%) of acute pancreatitis; and the BMI was $30 (obese) in nine patients, with two cases of acute pancreatitis (22.22%). -

Intrahepatic Pancreatic Pseudocyst: Case Series
JOP. J Pancreas (Online) 2016 Jul 08; 17(4):410-413. CASE SERIES Intrahepatic Pancreatic Pseudocyst: Case Series Dhaval Gupta, Nirav Pipaliya, Nilesh Pandav, Kaivan Shah, Meghraj Ingle, Prabha Sawant Department of Gastroenterology, Lokmanya Tilak Municipal Medical College &Hospital, Sion, Mumbai, India ABSTRACT Intrahepatic pseudocyst is a very rare complication of pancreatitis. Lack of experience and literature makes diagnosis and management of intrahepatic pseudocyst very difficult. Majority of published cases were managed by either percutaneous or surgical drainage. Less than 30 cases of intrahepatic pseudocysts have been reported in the literature and there is not a single report of endoscopic ultrasound guided management of intrahepatic pseudocysts. Here we report a case series of 2 patients who presented with intrahepatic pseudocysts and out of which first case was successfully managed by EUS guided drainage. Our second case is also the youngest patient presented with intrahepatic pseudocyst till now. INTRODUCTION abdominal distention since last 1 month. However he did located in or around t not have significant weight loss, gastrointestinal bleeding, A pancreatic pseudocyst is a collection of pancreatic fluid pedal edema, jaundice, fever. His past medical history and he pancreas. Pancreatic pseudocysts family history was not significant. He was chronic alcoholic are encased by a non-epithelial lining of fibrous, necrotic since last 15 years with intake of approximately 90 gram and granulation tissue secondary to pancreatic injury. -

Clinical Biliary Tract and Pancreatic Disease
Clinical Upper Gastrointestinal Disorders in Urgent Care, Part 2: Biliary Tract and Pancreatic Disease Urgent message: Upper abdominal pain is a common presentation in urgent care practice. Narrowing the differential diagnosis is sometimes difficult. Understanding the pathophysiology of each disease is the key to making the correct diagnosis and providing the proper treatment. TRACEY Q. DAVIDOFF, MD art 1 of this series focused on disorders of the stom- Pach—gastritis and peptic ulcer disease—on the left side of the upper abdomen. This article focuses on the right side and center of the upper abdomen: biliary tract dis- ease and pancreatitis (Figure 1). Because these diseases are regularly encountered in the urgent care center, the urgent care provider must have a thorough understand- ing of them. Biliary Tract Disease The gallbladder’s main function is to concentrate bile by the absorption of water and sodium. Fasting retains and concentrates bile, and it is secreted into the duodenum by eating. Impaired gallbladder contraction is seen in pregnancy, obesity, rapid weight loss, diabetes mellitus, and patients receiving total parenteral nutrition (TPN). About 10% to 15% of residents of developed nations will form gallstones in their lifetime.1 In the United States, approximately 6% of men and 9% of women 2 have gallstones. Stones form when there is an imbal- ©Phototake.com ance in the chemical constituents of bile, resulting in precipitation of one or more of the components. It is unclear why this occurs in some patients and not others, Tracey Q. Davidoff, MD, is an urgent care physician at Accelcare Medical Urgent Care in Rochester, New York, is on the Board of Directors of the although risk factors do exist. -

In Patients with Crohn's Disease Gut: First Published As 10.1136/Gut.38.3.379 on 1 March 1996
Gut 1996; 38: 379-383 379 High frequency of helicobacter negative gastritis in patients with Crohn's disease Gut: first published as 10.1136/gut.38.3.379 on 1 March 1996. Downloaded from L Halme, P Karkkainen, H Rautelin, T U Kosunen, P Sipponen Abstract In a previous study we described upper gastro- The frequency of gastric Crohn's disease intestinal lesions characteristic of CD in 17% has been considered low. This study was of patients with ileocolonic manifestations of undertaken to determine the prevalence of the disease.10 Furthermore, 40% of these chronic gastritis and Helicobacter pylori patients had chronic, non-specific gastritis. infection in patients with Crohn's disease. This study aimed to determine the prevalence Oesophagogastroduodenoscopy was per- of chronic gastritis and that of H pylori infec- formed on 62 consecutive patients suffer- tion in patients with CD who had undergone ing from ileocolonic Crohn's disease. oesophagogastroduodenoscopy (OGDS) at the Biopsy specimens from the antrum and Fourth Department of Surgery, Helsinki corpus were processed for both histological University Hospital between 1989 and 1994. and bacteriological examinations. Hpylori antibodies of IgG and IgA classes were measured in serum samples by enzyme Patients and methods immunoassay. Six patients (9.70/o) were During a five year period from September 1989 infected with H pylorn, as shown by histo- to August 1994, OGDS was performed on 62 logy, and in five of them the infection consecutive patients with CD to establish the was also verified by serology. Twenty one distribution of their disease. During the study patients (32%) had chronic H pyloni period, the OGDS was repeated (one to seven negative gastritis (negative by both times) - on three patients because of anaemia histology and serology) and one of them and on five patients because of upper gastroin- also had atrophy in the antrum and corpus. -

Abdominal Pain
10 Abdominal Pain Adrian Miranda Acute abdominal pain is usually a self-limiting, benign condition that irritation, and lateralizes to one of four quadrants. Because of the is commonly caused by gastroenteritis, constipation, or a viral illness. relative localization of the noxious stimulation to the underlying The challenge is to identify children who require immediate evaluation peritoneum and the more anatomically specific and unilateral inner- for potentially life-threatening conditions. Chronic abdominal pain is vation (peripheral-nonautonomic nerves) of the peritoneum, it is also a common complaint in pediatric practices, as it comprises 2-4% usually easier to identify the precise anatomic location that is produc- of pediatric visits. At least 20% of children seek attention for chronic ing parietal pain (Fig. 10.2). abdominal pain by the age of 15 years. Up to 28% of children complain of abdominal pain at least once per week and only 2% seek medical ACUTE ABDOMINAL PAIN attention. The primary care physician, pediatrician, emergency physi- cian, and surgeon must be able to distinguish serious and potentially The clinician evaluating the child with abdominal pain of acute onset life-threatening diseases from more benign problems (Table 10.1). must decide quickly whether the child has a “surgical abdomen” (a Abdominal pain may be a single acute event (Tables 10.2 and 10.3), a serious medical problem necessitating treatment and admission to the recurring acute problem (as in abdominal migraine), or a chronic hospital) or a process that can be managed on an outpatient basis. problem (Table 10.4). The differential diagnosis is lengthy, differs from Even though surgical diagnoses are fewer than 10% of all causes of that in adults, and varies by age group.