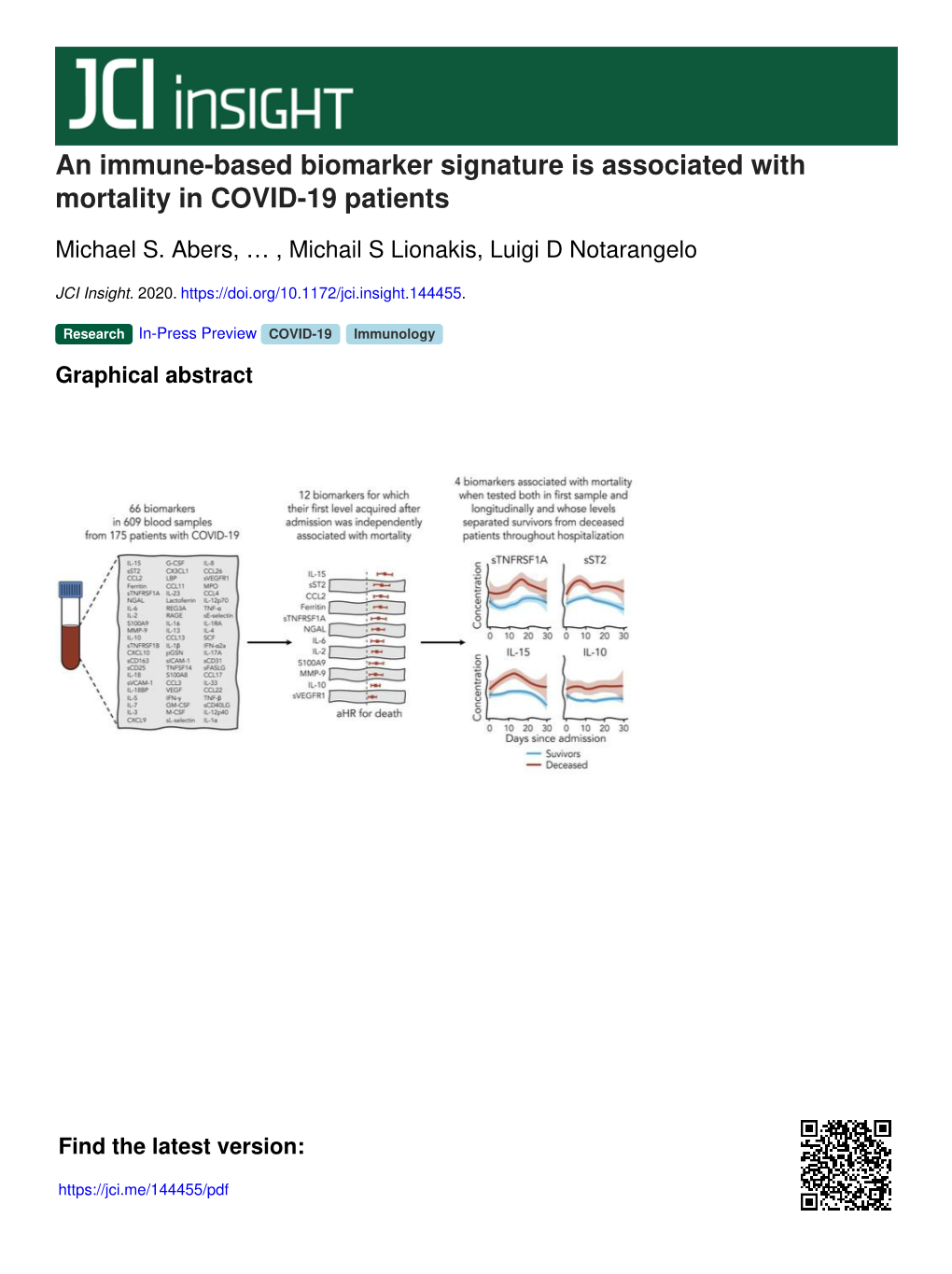
An Immune-Based Biomarker Signature Is Associated with Mortality in COVID-19 Patients
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

T Cell Binding to Activated Dendritic Cells Cutting Edge
Cutting Edge: CCR4 Mediates Antigen-Primed T Cell Binding to Activated Dendritic Cells Meng-tse Wu, Hui Fang and Sam T. Hwang This information is current as J Immunol 2001; 167:4791-4795; ; of September 27, 2021. doi: 10.4049/jimmunol.167.9.4791 http://www.jimmunol.org/content/167/9/4791 Supplementary http://www.jimmunol.org/content/suppl/2001/10/11/167.9.4791.DC1 Downloaded from Material References This article cites 32 articles, 13 of which you can access for free at: http://www.jimmunol.org/content/167/9/4791.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 27, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2001 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. ● Cutting Edge: CCR4 Mediates Antigen-Primed T Cell Binding to Activated Dendritic Cells Meng-tse Wu, Hui Fang, and Sam T. Hwang1 DC. In the periphery, activated, Ag-bearing DC may bind to cog- The binding of a T cell to an Ag-laden dendritic cell (DC) is a nate effector memory T cells (mTC). -

Genetics of Interleukin 1 Receptor-Like 1 in Immune and Inflammatory Diseases
Current Genomics, 2010, 11, 591-606 591 Genetics of Interleukin 1 Receptor-Like 1 in Immune and Inflammatory Diseases Loubna Akhabir and Andrew Sandford* Department of Medicine, University of British Columbia, UBC James Hogg Research Centre, Providence Heart + Lung Institute, Room 166, St. Paul's Hospital, 1081 Burrard Street, Vancouver, BC V6Z 1Y6, Canada Abstract: Interleukin 1 receptor-like 1 (IL1RL1) is gaining in recognition due to its involvement in immune/inflamma- tory disorders. Well-designed animal studies have shown its critical role in experimental allergic inflammation and human in vitro studies have consistently demonstrated its up-regulation in several conditions such as asthma and rheumatoid ar- thritis. The ligand for IL1RL1 is IL33 which emerged as playing an important role in initiating eosinophilic inflammation and activating other immune cells resulting in an allergic phenotype. An IL1RL1 single nucleotide polymorphism (SNP) was among the most significant results of a genome-wide scan inves- tigating eosinophil counts; in the same study, this SNP associated with asthma in 10 populations. The IL1RL1 gene resides in a region of high linkage disequilibrium containing interleukin 1 receptor genes as well as in- terleukin 18 receptor and accessory genes. This poses a challenge to researchers interested in deciphering genetic associa- tion signals in the region as all of the genes represent interesting candidates for asthma and allergic disease. The IL1RL1 gene and its resulting soluble and receptor proteins have emerged as key regulators of the inflammatory proc- ess implicated in a large variety of human pathologies We review the function and expression of the IL1RL1 gene. -

From IL-15 to IL-33: the Never-Ending List of New Players in Inflammation
From IL-15 to IL-33: the never-ending list of new players in inflammation. Is it time to forget the humble Aspirin and move ahead? Fulvio d’Acquisto, Francesco Maione, Magali Pederzoli-Ribeil To cite this version: Fulvio d’Acquisto, Francesco Maione, Magali Pederzoli-Ribeil. From IL-15 to IL-33: the never-ending list of new players in inflammation. Is it time to forget the humble Aspirin and move ahead?. Bio- chemical Pharmacology, Elsevier, 2009, 79 (4), pp.525. 10.1016/j.bcp.2009.09.015. hal-00544816 HAL Id: hal-00544816 https://hal.archives-ouvertes.fr/hal-00544816 Submitted on 9 Dec 2010 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Accepted Manuscript Title: From IL-15 to IL-33: the never-ending list of new players in inflammation. Is it time to forget the humble Aspirin and move ahead? Authors: Fulvio D’Acquisto, Francesco Maione, Magali Pederzoli-Ribeil PII: S0006-2952(09)00769-2 DOI: doi:10.1016/j.bcp.2009.09.015 Reference: BCP 10329 To appear in: BCP Received date: 30-7-2009 Revised date: 9-9-2009 Accepted date: 10-9-2009 Please cite this article as: D’Acquisto F, Maione F, Pederzoli-Ribeil M, From IL- 15 to IL-33: the never-ending list of new players in inflammation. -

Mechanism of Macrophage-Derived Chemokine/CCL22 Production by Hacat Keratinocytes
C Yano, et al Ann Dermatol Vol. 27, No. 2, 2015 http://dx.doi.org/10.5021/ad.2015.27.2.152 ORIGINAL ARTICLE Mechanism of Macrophage-Derived Chemokine/CCL22 Production by HaCaT Keratinocytes Chizuko Yano, Hidehisa Saeki1, Mayumi Komine2, Shinji Kagami3, Yuichiro Tsunemi4, Mamitaro Ohtsuki2, Hidemi Nakagawa Department of Dermatology, The Jikei University School of Medicine, 1Department of Dermatology, Nippon Medical School, Tokyo, 2Department of Dermatology, Jichi Medical University, Shimotsuke, 3Department of Dermatology, Kanto Central Hospital, 4Department of Dermatology, Tokyo Women’s Medical University, Tokyo, Japan Background: CC chemokine ligand 17 (CCL17) and CCL22 27(2) 152∼156, 2015) are the functional ligands for CCR4. We previously reported that inhibitors of nuclear factor-kappa B and p38 mi- -Keywords- togen-activated protein kinase (p38 MAPK), but not of ex- Chemokine CCL22, Chemokine CCL17, Epidermal growth tracellular signal-related kinase (ERK), inhibited tumor ne- factor receptor, HaCaT keratinocytes crosis factor (TNF)-α- and interferon (IFN)-γ-induced pro- duction of CCL17 by the human keratinocyte cell line, HaCaT. Further, an inhibitor of epidermal growth factor re- INTRODUCTION ceptor (EGFR) enhanced the CCL17 production by these keratinocytes. Objective: To identify the mechanism under- The macrophage-derived chemokine (MDC)/CC chemo- lying CCL22 production by HaCaT cells. Methods: We inves- kine ligand 22 (CCL22) is one of the functional ligands for tigated the signal transduction pathways by which TNF-α CC chemokine receptor 4 (CCR4) and is a chemoattractant and IFN-γ stimulate HaCaT cells to produce CCL22 by add- for the CCR4-expressing cells such as Th2 cells. We and ing various inhibitors. -

Differential Expression of Interferon-Γ and Chemokine Genes
Differential expression of interferon-γ and chemokine genes distinguishes Rasmussen encephalitis from cortical dysplasia and provides evidence for an early Th1 immune response Owens et al. Owens et al. Journal of Neuroinflammation 2013, 10:56 http://www.jneuroinflammation.com/content/10/1/56 Owens et al. Journal of Neuroinflammation 2013, 10:56 JOURNAL OF http://www.jneuroinflammation.com/content/10/1/56 NEUROINFLAMMATION RESEARCH Open Access Differential expression of interferon-γ and chemokine genes distinguishes Rasmussen encephalitis from cortical dysplasia and provides evidence for an early Th1 immune response Geoffrey C Owens1,7*, My N Huynh1, Julia W Chang1, David L McArthur1, Michelle J Hickey2, Harry V Vinters2,3, Gary W Mathern1,4,5,6† and Carol A Kruse1,6† Abstract Background: Rasmussen encephalitis (RE) is a rare complex inflammatory disease, primarily seen in young children, that is characterized by severe partial seizures and brain atrophy. Surgery is currently the only effective treatment option. To identify genes specifically associated with the immunopathology in RE, RNA transcripts of genes involved in inflammation and autoimmunity were measured in brain tissue from RE surgeries and compared with those in surgical specimens of cortical dysplasia (CD), a major cause of intractable pediatric epilepsy. Methods: Quantitative polymerase chain reactions measured the relative expression of 84 genes related to inflammation and autoimmunity in 12 RE specimens and in the reference group of 12 CD surgical specimens. Data were analyzed by consensus clustering using the entire dataset, and by pairwise comparison of gene expression levels between the RE and CD cohorts using the Harrell-Davis distribution-free quantile estimator method. -

The IL-1-Like Cytokine IL-33 Is Inactivated After Maturation by Caspase-1
The IL-1-like cytokine IL-33 is inactivated after maturation by caspase-1 Corinne Cayrola,b and Jean-Philippe Girarda,b,1 aCentre National de la Recherche Scientifique, Institut de Pharmacologie et de Biologie Structurale, F-31077 Toulouse, France; and bUniversite´de Toulouse, Universite´Paul Sabatier, Institut de Pharmacologie et de Biologie Structurale, F-31077 Toulouse, France Edited by Charles A. Dinarello, University of Colorado Health Sciences Center, Denver, CO, and approved April 10, 2009 (received for review December 13, 2008) IL-33 is a chromatin-associated cytokine of the IL-1 family that has that nuclear IL-33 possesses transcriptional regulatory proper- recently been linked to many diseases, including asthma, rheuma- ties and associates with chromatin in vivo (5). Recently, we found toid arthritis, atherosclerosis, and cardiovascular diseases. IL-33 that IL-33 mimics Kaposi sarcoma herpesvirus for attachment to signals through the IL-1 receptor-related protein ST2 and drives chromatin, and docks, through a short chromatin-binding pep- production of pro-inflammatory and T helper type 2-associated tide, into the acidic pocket formed by the histone H2A-H2B cytokines in mast cells, T helper type 2 lymphocytes, basophils, dimer at the surface of the nucleosome (22). Together, our eosinophils, invariant natural killer T cells, and natural killer cells. findings suggested IL-33 is a dual-function protein that may play It is currently believed that IL-33, like IL-1 and IL-18, requires important roles as both a cytokine and an intracellular nuclear processing by caspase-1 to a mature form (IL-33112–270) for biolog- factor (5, 22). -

Interleukin-18 As a Therapeutic Target in Acute Myocardial Infarction and Heart Failure
Interleukin-18 as a Therapeutic Target in Acute Myocardial Infarction and Heart Failure Laura C O’Brien,1 Eleonora Mezzaroma,2,3,4 Benjamin W Van Tassell,2,3,4 Carlo Marchetti,2,3 Salvatore Carbone,2,3 Antonio Abbate,1,2,3 and Stefano Toldo2,3 1Department of Physiology and Biophysics, 2Victoria Johnson Research Laboratories, and 3Virginia Commonwealth University Pauley Heart Center, School of Medicine, and 4Pharmacotherapy and Outcome Sciences, School of Pharmacy, Virginia Commonwealth University, Richmond, Virginia, United States of America Interleukin 18 (IL-18) is a proinflammatory cytokine in the IL-1 family that has been implicated in a number of disease states. In animal models of acute myocardial infarction (AMI), pressure overload, and LPS-induced dysfunction, IL-18 regulates cardiomy- ocyte hypertrophy and induces cardiac contractile dysfunction and extracellular matrix remodeling. In patients, high IL-18 levels correlate with increased risk of developing cardiovascular disease (CVD) and with a worse prognosis in patients with established CVD. Two strategies have been used to counter the effects of IL-18:IL-18 binding protein (IL-18BP), a naturally occurring protein, and a neutralizing IL-18 antibody. Recombinant human IL-18BP (r-hIL-18BP) has been investigated in animal studies and in phase I/II clinical trials for psoriasis and rheumatoid arthritis. A phase II clinical trial using a humanized monoclonal IL-18 antibody for type 2 diabetes is ongoing. Here we review the literature regarding the role of IL-18 in AMI and heart failure and the evidence and challenges of using IL-18BP and blocking IL-18 antibodies as a therapeutic strategy in patients with heart disease. -

Biomarker Quantitation Assay Guide
Biomarker quantitation assay guide Quantitate protein: ELISA l Antibody pairs l ProQuantum HS immunoassays l ProcartaPlex immunoassays Quantitate mRNA: QuantiGene multiplexed gene expression assays Our Invitrogen™ portfolio offers a variety of assays for quantitation of single proteins and mRNA, as well as mix-and-match and ready-to-use panels for correlated multiplexing using the Luminex® platform. Our extensive portfolio of assays includes: • ELISA and antibody pair kits • ProQuantum™ high-sensitivity immunoassay kits • ProcartaPlex™ multiplex immunoassay kits • QuantiGene™ Plex gene expression assays Additionally, Thermo Fisher Scientific supports your quantitation assay needs with accessory reagents and instruments for a comprehensive offering. Use this guide to help identify your needs, and then contact your sales representative if you have questions or go to thermofisher.com/quantitatebiomarkers Contents Biomarker background 4 Biomarker quantitation assay platforms 7 Single-analyte quantitation ELISA kits 9 Antibody pair kits 11 ProQuantum high-sensitivity immunoassay kits 12 Accessory reagents and equipment 14 Multianalyte quantitation Luminex xMAP technology 17 ProcartaPlex multiplex immunoassay kits 19 ProcartaPlex high-sensitivity immunoassay kits 27 ProcartaPlex Platinum immunoassay kits 28 Custom assay development service 30 Multiplexed gene expression assays 32 QuantiGene Plex assays 32 Additional gene expression solutions 38 Comprehensive immunoassay product listing 40 Biomarker background Highly referenced kits you can -

Interleukin-33 Signaling Exacerbates Experimental Infectious Colitis by Enhancing Gut Permeability and Inhibiting Protective Th17 Immunity
www.nature.com/mi ARTICLE OPEN Interleukin-33 signaling exacerbates experimental infectious colitis by enhancing gut permeability and inhibiting protective Th17 immunity Vittoria Palmieri1, Jana-Fabienne Ebel1, Nhi Ngo Thi Phuong1, Robert Klopfleisch2, Vivian Pham Vu3,4, Alexandra Adamczyk1, Julia Zöller1, Christian Riedel5, Jan Buer1, Philippe Krebs3, Wiebke Hansen1, Eva Pastille1 and Astrid M. Westendorf 1 A wide range of microbial pathogens is capable of entering the gastrointestinal tract, causing infectious diarrhea and colitis. A finely tuned balance between different cytokines is necessary to eradicate the microbial threat and to avoid infection complications. The current study identified IL-33 as a critical regulator of the immune response to the enteric pathogen Citrobacter rodentium.We observed that deficiency of the IL-33 signaling pathway attenuates bacterial-induced colitis. Conversely, boosting this pathway strongly aggravates the inflammatory response and makes the mice prone to systemic infection. Mechanistically, IL-33 mediates its detrimental effect by enhancing gut permeability and by limiting the induction of protective T helper 17 cells at the site of infection, thus impairing host defense mechanisms against the enteric pathogen. Importantly, IL-33-treated infected mice supplemented with IL-17A are able to resist the otherwise strong systemic spreading of the pathogen. These findings reveal a novel IL-33/IL-17A crosstalk that controls the pathogenesis of Citrobacter rodentium-driven infectious colitis. Manipulating the dynamics of cytokines may offer new therapeutic strategies to treat specific intestinal infections. 1234567890();,: Mucosal Immunology (2021) 14:923–936; https://doi.org/10.1038/s41385-021-00386-7 INTRODUCTION epithelial cells, and endothelial cells in response to injury6. -

The Relevance of Clinical, Genetic and Serological Markers
AUTREV-01901; No of Pages 18 Autoimmunity Reviews xxx (2016) xxx–xxx Contents lists available at ScienceDirect Autoimmunity Reviews journal homepage: www.elsevier.com/locate/autrev Review Cardiovascular risk assessment in patients with rheumatoid arthritis: The relevance of clinical, genetic and serological markers Raquel López-Mejías a, Santos Castañeda b, Carlos González-Juanatey c,AlfonsoCorralesa, Iván Ferraz-Amaro d, Fernanda Genre a, Sara Remuzgo-Martínez a, Luis Rodriguez-Rodriguez e, Ricardo Blanco a,JavierLlorcaf, Javier Martín g, Miguel A. González-Gay a,h,i,⁎ a Epidemiology, Genetics and Atherosclerosis Research Group on Systemic Inflammatory Diseases, Rheumatology Division, IDIVAL, Santander, Spain b Division of Rheumatology, Hospital Universitario la Princesa, IIS-IPrincesa, Madrid, Spain c Division of Cardiology, Hospital Lucus Augusti, Lugo, Spain d Rheumatology Division, Hospital Universitario de Canarias, Santa Cruz de Tenerife, Spain e Division of Rheumatology, Hospital Clínico San Carlos, Madrid, Spain f Division of Epidemiology and Computational Biology, School of Medicine, University of Cantabria, and CIBER Epidemiología y Salud Pública (CIBERESP), IDIVAL, Santander, Spain g Institute of Parasitology and Biomedicine López-Neyra, IPBLN-CSIC, Granada, Spain h School of Medicine, University of Cantabria, Santander, Spain i Cardiovascular Pathophysiology and Genomics Research Unit, School of Physiology, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa article info abstract Article history: Cardiovascular disease (CV) is the most common cause of premature mortality in patients with rheumatoid ar- Received 7 July 2016 thritis (RA). This is the result of an accelerated atherosclerotic process. Adequate CV risk stratification has special Accepted 9 July 2016 relevance in RA to identify patients at risk of CV disease. -

Interleukin-18 in Health and Disease
International Journal of Molecular Sciences Review Interleukin-18 in Health and Disease Koubun Yasuda 1 , Kenji Nakanishi 1,* and Hiroko Tsutsui 2 1 Department of Immunology, Hyogo College of Medicine, 1-1 Mukogawa-cho, Nishinomiya, Hyogo 663-8501, Japan; [email protected] 2 Department of Surgery, Hyogo College of Medicine, 1-1 Mukogawa-cho, Nishinomiya, Hyogo 663-8501, Japan; [email protected] * Correspondence: [email protected]; Tel.: +81-798-45-6573 Received: 21 December 2018; Accepted: 29 January 2019; Published: 2 February 2019 Abstract: Interleukin (IL)-18 was originally discovered as a factor that enhanced IFN-γ production from anti-CD3-stimulated Th1 cells, especially in the presence of IL-12. Upon stimulation with Ag plus IL-12, naïve T cells develop into IL-18 receptor (IL-18R) expressing Th1 cells, which increase IFN-γ production in response to IL-18 stimulation. Therefore, IL-12 is a commitment factor that induces the development of Th1 cells. In contrast, IL-18 is a proinflammatory cytokine that facilitates type 1 responses. However, IL-18 without IL-12 but with IL-2, stimulates NK cells, CD4+ NKT cells, and established Th1 cells, to produce IL-3, IL-9, and IL-13. Furthermore, together with IL-3, IL-18 stimulates mast cells and basophils to produce IL-4, IL-13, and chemical mediators such as histamine. Therefore, IL-18 is a cytokine that stimulates various cell types and has pleiotropic functions. IL-18 is a member of the IL-1 family of cytokines. IL-18 demonstrates a unique function by binding to a specific receptor expressed on various types of cells. -
Ccl17-Dependent Release of Ccl3 Restrains Regulatory T Cells Thereby Aggravating Atherosclerosis
From the Institute for Cardiovascular Prevention (IPEK) of the Ludwig-Maximilians-Universität München Director: Univ.-Prof. Dr. med. Christian Weber Ccl17-dependent release of Ccl3 restrains regulatory T cells thereby aggravating atherosclerosis Dissertation zum Erwerb des Doctor of Philosophy (Ph.D.) an der Medizinischen Fakultät der Ludwig-Maximilians-Universität München Submitted by M.Sc. Carlos Neideck from Taió in Santa Catarina, Brazil on 21.03.2018 Supervisor: Prof. Dr. med. Christian Weber Second evaluator: Prof. Dr. rer. nat. Jürgen Bernhagen Dean: Prof. Dr. Reinhard Hickel Date of oral defense: 23.07.2018 Affidavit Neideck, Carlos ______________________________________________________________________ Name, Surname ______________________________________________________________________ Street ______________________________________________________________________ Zip Code, Town ______________________________________________________________________ Country I hereby declare, that the submitted thesis entitled: “Ccl17-dependent release of Ccl3 restrains regulatory T cells thereby aggravating atherosclerosis.” is my own work. I have only used the sources indicated and have not made unauthorized use of services of a third party. Where the work of others has been quoted or reproduced, the source is always given. I further declare that the submitted thesis or parts thereof have not been presented as part of an examination degree to any other university. Munich, 25.07.2018 Carlos Neideck Place, date Signature doctoral candidate Confirmation