Elective Induction of Labor Protocol for Singleton Pregnancies
Total Page:16
File Type:pdf, Size:1020Kb
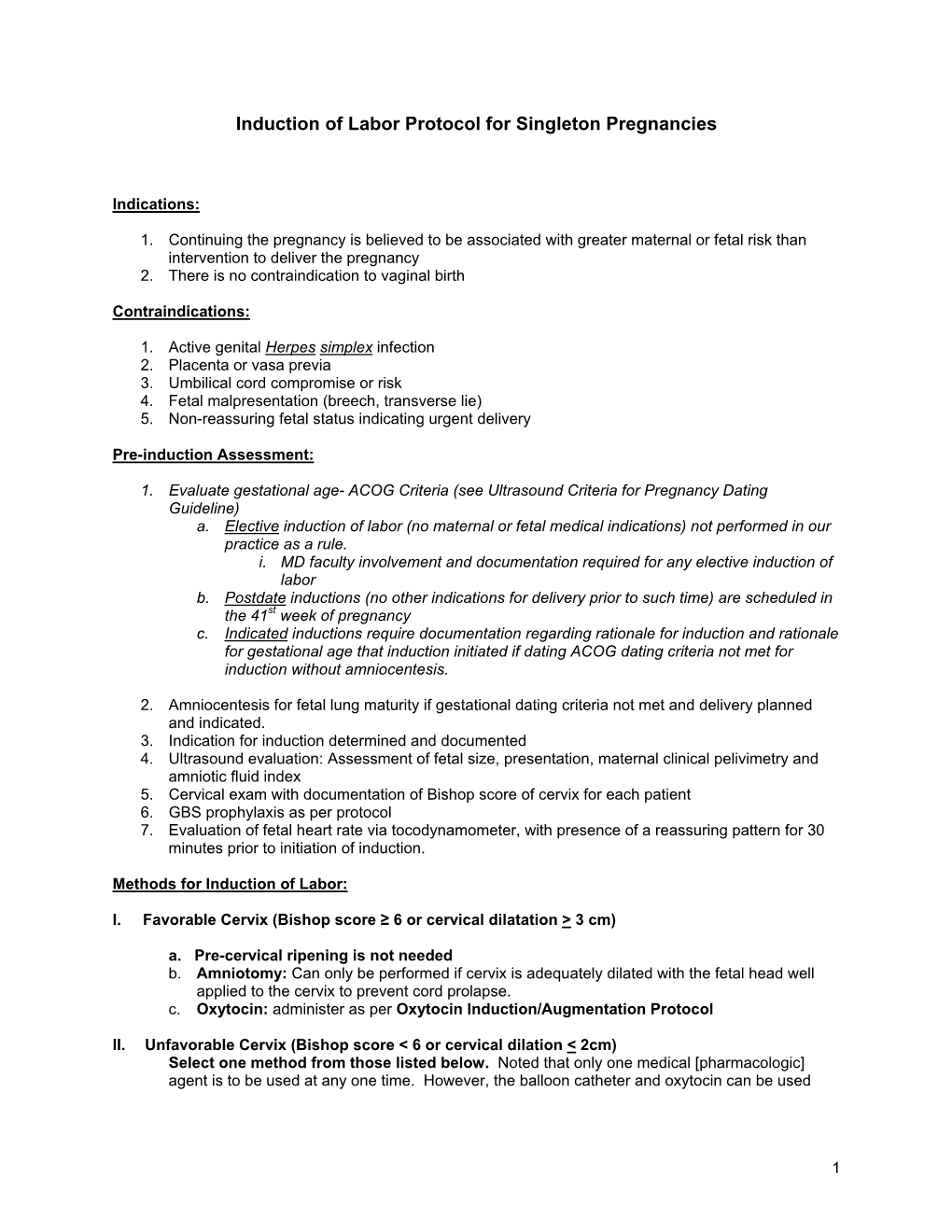
Load more
Recommended publications
-

Preventing the First Cesarean Delivery
Current Commentary Preventing the First Cesarean Delivery Summary of a Joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal- Fetal Medicine, and American College of Obstetricians and Gynecologists Workshop Catherine Y. Spong, MD, Vincenzo Berghella, MD, Katharine D. Wenstrom, MD, Brian M. Mercer, MD, and George R. Saade, MD points were identified to assist with reduction in cesar- With more than one third of pregnancies in the United ean delivery rates including that labor induction should States being delivered by cesarean and the growing be performed primarily for medical indication; if done knowledge of morbidities associated with repeat cesar- for nonmedical indications, the gestational age should be ean deliveries, the Eunice Kennedy Shriver National Insti- at least 39 weeks or more and the cervix should be favor- tute of Child Health and Human Development, the able, especially in the nulliparous patient. Review of the Society for Maternal-Fetal Medicine, and the American current literature demonstrates the importance of adher- College of Obstetricians and Gynecologists convened ing to appropriate definitions for failed induction and a workshop to address the concept of preventing the first arrest of labor progress. The diagnosis of “failed induc- cesarean delivery. The available information on maternal tion” should only be made after an adequate attempt. and fetal factors, labor management and induction, and Adequate time for normal latent and active phases of nonmedical factors leading to the first cesarean delivery the first stage, and for the second stage, should be was reviewed as well as the implications of the first allowed as long as the maternal and fetal conditions per- cesarean delivery on future reproductive health. -

Labor and Vaginal Delivery
VI LABOR, DELIVERY, AND POSTPARTUM LABOR AND VAGINAL DELIVERY Kelly A. Best, MD CHAPTER 61 1. What is the definition of labor? Labor begins when uterine contractions of sufficient frequency, intensity, and duration are attained to bring about effacement and progressive dilation of the cervix. 2. What two steps are theorized to be crucial to the initiation of labor in human pregnancy? 1. Retreat from pregnancy maintenance 2. Uterotonic induction Despite extensive investigation into the associated physiologic and biochemical changes, the physiologic processes in human pregnancy that result in the onset of labor are still not defined. 3. In which patients is induction of labor considered? Awaiting the onset of normal labor may not be an option in certain circumstances. At preterm gestations, indications for labor induction include severe preeclampsia, fetal growth restriction with abnormal antepartum surveillance or other evidence of fetal compromise, and deterioration of maternal disease to the point that continuation of pregnancy is believed to be detrimental. In cases of rupture of membranes without labor (i.e., premature rupture of membranes) at term (37 to 42 weeks) or postterm (≥42 weeks), induction of labor is often performed. 4. What is a Bishop score, and how is it used? A Bishop score is a quantifiable method to assess the likelihood of a successful induction. Elements include dilation, effacement, station, consistency, and position of the cervix (Table 61-1). A score of 6 or less trans- lates into a need to ripen the cervix and is associated with less successful inductions. A score 8 or greater generally means the cervix does not need ripening and induction is more likely to be successful. -

A Guide to Obstetrical Coding Production of This Document Is Made Possible by Financial Contributions from Health Canada and Provincial and Territorial Governments
ICD-10-CA | CCI A Guide to Obstetrical Coding Production of this document is made possible by financial contributions from Health Canada and provincial and territorial governments. The views expressed herein do not necessarily represent the views of Health Canada or any provincial or territorial government. Unless otherwise indicated, this product uses data provided by Canada’s provinces and territories. All rights reserved. The contents of this publication may be reproduced unaltered, in whole or in part and by any means, solely for non-commercial purposes, provided that the Canadian Institute for Health Information is properly and fully acknowledged as the copyright owner. Any reproduction or use of this publication or its contents for any commercial purpose requires the prior written authorization of the Canadian Institute for Health Information. Reproduction or use that suggests endorsement by, or affiliation with, the Canadian Institute for Health Information is prohibited. For permission or information, please contact CIHI: Canadian Institute for Health Information 495 Richmond Road, Suite 600 Ottawa, Ontario K2A 4H6 Phone: 613-241-7860 Fax: 613-241-8120 www.cihi.ca [email protected] © 2018 Canadian Institute for Health Information Cette publication est aussi disponible en français sous le titre Guide de codification des données en obstétrique. Table of contents About CIHI ................................................................................................................................. 6 Chapter 1: Introduction .............................................................................................................. -

THE PRACTICE of EPISIOTOMY: a QUALITATIVE DESCRIPTIVE STUDY on PERCEPTIONS of a GROUP of WOMEN Online Brazilian Journal of Nursing, Vol
Online Brazilian Journal of Nursing E-ISSN: 1676-4285 [email protected] Universidade Federal Fluminense Brasil Yi Wey, Chang; Rejane Salim, Natália; Pires de Oliveira Santos Junior, Hudson; Gualda, Dulce Maria Rosa THE PRACTICE OF EPISIOTOMY: A QUALITATIVE DESCRIPTIVE STUDY ON PERCEPTIONS OF A GROUP OF WOMEN Online Brazilian Journal of Nursing, vol. 10, núm. 2, abril-agosto, 2011, pp. 1-11 Universidade Federal Fluminense Rio de Janeiro, Brasil Available in: http://www.redalyc.org/articulo.oa?id=361441674008 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative THE PRACTICE OF EPISIOTOMY: A QUALITATIVE DESCRIPTIVE STUDY ON PERCEPTIONS OF A GROUP OF WOMEN Chang Yi Wey1, Natália Rejane Salim2, Hudson Pires de Oliveira Santos Junior3, Dulce Maria Rosa Gualda4 1. Hospital Universitário, Universidade de São Paulo 2,3,4. Escola de Enfermagem, Universidade de São Paulo ABSTRACT: This study set out to understand the experiences and perceptions of women from the practices of episiotomy during labor. This is a qualitative descriptive approach, performed in a school hospital in São Paulo, which data were collected through interviews with the participation of 35 women, who experienced and not episiotomy in labor. The thematic analysis shows these categories: Depends the size of the baby facilitates the childbirth; Depends each woman; The woman is not open; and Episiotomy is not necessary. The results allowed that there is lack of clarification and knowledge regarding this practice, which makes the role of decision ends up in the professionals’ hands. -

2020 CDA Paper Abstraction Forms
2020 OBI DATA ABSTRACTION FORMS DEMOGRAPHICS Hospital Name: Patient Last Name: Patient First Name: Medical Record Number (MRN): Maternal Birthdate (MM/DD/YY): Postal Zip Hispanic Ethnicity: Code: Hispanic or Latino Not Hispanic or Latino Race (select all that apply): Unknown American Indian or Alaskan Native Asian Patient's Insurance Type: Black or African American Medicaid Self Pay/None Native Hawaiian or Other Pacific Islander Private Other: __________ White Unknown LABOR MANAGEMENT: Admission L&D Admission Date: L&D Admission Time: Provider admitting patient to Labor & Delivery (Last Name, First Name): Service/Practice patient admitted to: Admitting Nurse (Last name, First name): Certified Nurse Midwife Family Practice / Family Medicine Gravidity on admission: Parity on admission: Maternal Fetal Medicine Obstetrics Physician Maternal Height at admission: Maternal Weight at admission: Pre-pregnancy Weight: IN LBS LBS CM K G KG Did the patient receive prenatal care? If yes, date prenatal care Transfer of care from an intended home birth? started: Yes No Unable to determine Yes No LABOR MANAGEMENT: Maternal Comorbidities Present On Admission Pre-pregnancy diabetes (Type I or Type II Yes Was the patient using opioids during this Yes diabetes diagnosed prior to this pregnancy) No pregnancy? No Gestational diabetes (diagnosis in this pregnancy Yes What was the status of the patient's opioid use during this with or without medication tx) No pregnancy? (select all that apply): In treatment for opioid use disorder during pregnancy Pre-pregnancy -

Hospital Maternity Care Report Card, 2018
New Jersey Hospital Maternity Care Report Card, 2018 Revised on 06/16/2020 1 | P a g e HEALTHCARE QUALITY AND INFORMATICS Prepared by: Erin Mayo, DVM, MPH Genevieve Lalanne-Raymond, RN, MPH Mehnaz Mustafa, MPH, MSc Yannai Kranzler, PhD Technical Support Andreea A. Creanga, MD, PhD Debra Bingham, DrPH, RN, FAAN Jennifer Fearon, MPH Marcela Maziarz, MPA Hospital Partners Diana Contreras, MD-Atlantic Health System Lisa Gittens-Williams, MD Obstetrics & Gynecology– University Hospital Thomas Westover, MD, FACOG- Cooper University Health Care Perry L. Robin, MD, MSEd, FACOG- Cooper University Health Care Hewlett Guy, MD, FACOG- Cooper University Health Care Suzanne Spernal, DNP, APN-BC, RNC-OB, CBC- RWJBarnabas Health 2 | P a g e Table of Contents Statute ........................................................................................................................................................... 5 Summary of the Statute ............................................................................................................................. 5 Summary of Findings ................................................................................................................................ 6 Variation in Delivery Outcomes by Hospital .................................................................................... 6 Complication Rates by Race/Ethnicity: ............................................................................................ 6 General Observations ........................................................................................................................ -

OBGYN-Study-Guide-1.Pdf
OBSTETRICS PREGNANCY Physiology of Pregnancy: • CO input increases 30-50% (max 20-24 weeks) (mostly due to increase in stroke volume) • SVR anD arterial bp Decreases (likely due to increase in progesterone) o decrease in systolic blood pressure of 5 to 10 mm Hg and in diastolic blood pressure of 10 to 15 mm Hg that nadirs at week 24. • Increase tiDal volume 30-40% and total lung capacity decrease by 5% due to diaphragm • IncreaseD reD blooD cell mass • GI: nausea – due to elevations in estrogen, progesterone, hCG (resolve by 14-16 weeks) • Stomach – prolonged gastric emptying times and decreased GE sphincter tone à reflux • Kidneys increase in size anD ureters dilate during pregnancy à increaseD pyelonephritis • GFR increases by 50% in early pregnancy anD is maintaineD, RAAS increases = increase alDosterone, but no increaseD soDium bc GFR is also increaseD • RBC volume increases by 20-30%, plasma volume increases by 50% à decreased crit (dilutional anemia) • Labor can cause WBC to rise over 20 million • Pregnancy = hypercoagulable state (increase in fibrinogen anD factors VII-X); clotting and bleeding times do not change • Pregnancy = hyperestrogenic state • hCG double 48 hours during early pregnancy and reach peak at 10-12 weeks, decline to reach stead stage after week 15 • placenta produces hCG which maintains corpus luteum in early pregnancy • corpus luteum produces progesterone which maintains enDometrium • increaseD prolactin during pregnancy • elevation in T3 and T4, slight Decrease in TSH early on, but overall euthyroiD state • linea nigra, perineum, anD face skin (melasma) changes • increase carpal tunnel (median nerve compression) • increased caloric need 300cal/day during pregnancy and 500 during breastfeeding • shoulD gain 20-30 lb • increaseD caloric requirements: protein, iron, folate, calcium, other vitamins anD minerals Testing: In a patient with irregular menstrual cycles or unknown date of last menstruation, the last Date of intercourse shoulD be useD as the marker for repeating a urine pregnancy test. -

• Chapter 8 • Nursing Care of Women with Complications During Labor and Birth • Obstetric Procedures • Amnioinfusion –
• Chapter 8 • Nursing Care of Women with Complications During Labor and Birth • Obstetric Procedures • Amnioinfusion – Oligohydramnios – Umbilical cord compression – Reduction of recurrent variable decelerations – Dilution of meconium-stained amniotic fluid – Replaces the “cushion ” for the umbilical cord and relieves the variable decelerations • Obstetric Procedures (cont.) • Amniotomy – The artificial rupture of membranes – Done to stimulate or enhance contractions – Commits the woman to delivery – Stimulates prostaglandin secretion – Complications • Prolapse of the umbilical cord • Infection • Abruptio placentae • Obstetric Procedures (cont.) • Observe for complications post-amniotomy – Fetal heart rate outside normal range (110-160 beats/min) suggests umbilical cord prolapse – Observe color, odor, amount, and character of amniotic fluid – Woman ’s temperature 38 ° C (100.4 ° F) or higher is suggestive of infection – Green fluid may indicate that the fetus has passed a meconium stool • Nursing Tip • Observe for wet underpads and linens after the membranes rupture. Change them as often as needed to keep the woman relatively dry and to reduce the risk for infection or skin breakdown. • Induction or Augmentation of Labor • Induction is the initiation of labor before it begins naturally • Augmentation is the stimulation of contractions after they have begun naturally • Indications for Labor Induction • Gestational hypertension • Ruptured membranes without spontaneous onset of labor • Infection within the uterus • Medical problems in the -

Pretest Obstetrics and Gynecology
Obstetrics and Gynecology PreTestTM Self-Assessment and Review Notice Medicine is an ever-changing science. As new research and clinical experience broaden our knowledge, changes in treatment and drug therapy are required. The authors and the publisher of this work have checked with sources believed to be reliable in their efforts to provide information that is complete and generally in accord with the standards accepted at the time of publication. However, in view of the possibility of human error or changes in medical sciences, neither the authors nor the publisher nor any other party who has been involved in the preparation or publication of this work warrants that the information contained herein is in every respect accurate or complete, and they disclaim all responsibility for any errors or omissions or for the results obtained from use of the information contained in this work. Readers are encouraged to confirm the information contained herein with other sources. For example and in particular, readers are advised to check the prod- uct information sheet included in the package of each drug they plan to administer to be certain that the information contained in this work is accurate and that changes have not been made in the recommended dose or in the contraindications for administration. This recommendation is of particular importance in connection with new or infrequently used drugs. Obstetrics and Gynecology PreTestTM Self-Assessment and Review Twelfth Edition Karen M. Schneider, MD Associate Professor Department of Obstetrics, Gynecology, and Reproductive Sciences University of Texas Houston Medical School Houston, Texas Stephen K. Patrick, MD Residency Program Director Obstetrics and Gynecology The Methodist Health System Dallas Dallas, Texas New York Chicago San Francisco Lisbon London Madrid Mexico City Milan New Delhi San Juan Seoul Singapore Sydney Toronto Copyright © 2009 by The McGraw-Hill Companies, Inc. -

Bain Birthing Center Statistics
THE BAIN BIRTHING CENTER Our 2019 Statistics We are pleased to make available to you the following information about Mount Auburn Hospital's obstetrics program. We hope you will find this fact sheet interesting and informative, and we strongly encourage you to discuss any questions you might have with your health care provider or childbirth educator. MOUNT AUBURN HOSPITAL Mount Auburn Hospital is a Harvard Medical School community teaching hospital. Our goal is to provide personal, individualized care in a setting of clinical excellence. There are 22 obstetricians and 26 midwives on the staff. Last year, midwives attended 39% of the births at Mount Auburn Hospital. Labor/Delivery/Recovery Rooms (LDR's) The Bain Birthing Center at Mount Auburn Hospital welcomed 2481 birth parents and 2513 babies in 2019 (32 sets of twins!). All labor rooms are private Labor/Delivery/Recovery rooms (LDRs) with their own bathrooms and showers. Two of the rooms also have Jacuzzis. The Bain Birthing Center has expanded to include eight LDR rooms (one with a free standing birthing tub), a dedicated triage and evaluation area, and a four bed antepartum observation unit. Following the birth, families are transferred to a room in the maternity suite for their postpartum stay. Most parents and babies room-in together. There is a Level IIa Nursery for those babies who need special care. CESAREAN BIRTHS Although there are some babies who must be delivered by cesarean birth, we are strongly committed to keeping our rates as low as safely possible. The most common reasons for cesarean sections include fetal intolerance of labor (when the baby is dangerously stressed by uterine contractions), cephalopelvic disproportion or CPD (when the baby's head is larger than the mother's pelvis) and breech presentation (when the baby's buttocks are coming first instead of the head). -

Obi Data Abstraction Forms Demographics
OBI DATA ABSTRACTION FORMS DEMOGRAPHICS Last Name: First Name: Patient MRN: Maternal Birthdate: Ethnicity: Hispanic or Latino / / Not Hispanic or Latino Race (select all that apply): Postal Zip Code: American Indian or Alaskan Native Asian Patient's Insurance Type: Black Medicaid Self Pay/None Native Hawaiian or Other Pacific Islander Private Other White ADMISSION Admission Date: Admission Time: Provider admitting patient to Labor & Delivery: / / Service/Practice patient admitted to: Admitting nurse: Certified Nurse Midwife Family Practice Gravidity on admission: Parity on admission: Maternal Fetal Medicine Obstetrics Physician Height at admission: Weight at admission: Pre-pregnancy weight: IN LBS LBS CM KG KG Did patient receive prenatal care? Date prenatal care started: Transfer of care from an intended home birth? Yes No Unable to determine / / Yes No MATERNAL COMORBIDITIES PRESENT ON ADMISSION Pre-pregnancy diabetes (Type I or Type II Yes Was the patient using opioids during this Yes diabetes diagnosed prior to this pregnancy) No pregnancy? No Gestational diabetes (diagnosis in this Yes What was the status of the patient's opioid use during this pregnancy with or without medication tx) No pregnancy? Select all that apply: Yes In treatment for opioid use disorder during pregnancy Pre-pregnancy hypertension (chronic) No Ongoing opioid/heroin use disorder (without current tx) Gestational hypertension (PIH, preeclampsia, Yes Opioid use for acute pain eclampsia, HELLP syndrome) No Opioid use for chronic pain Alcohol Use During Pregnancy? -

Intrauterine Pressure Catheter Insertion External Cardiotogography
Appendix 4 Fetal Surveillance – Intrauterine Pressure Catheter Insertion External Cardiotogography (CTG) provides an objective record of the frequency and duration of contractions however the tracing can be interrupted by maternal movement or difficult to capture due to maternal habitus. An intrauterine pressure catheter (IUPC) provides a quantifiable measure of uterine activity where clinically indicated. Indications for use For direct measurement of uterine contractions including: inability to monitor contractions well enough to assess timing of decelerations inability to monitor frequency of contractions as in the obese patient evaluation of contraction strength if patient’s labor process fails to progress. Requirements include the following: confirmed rupture of membranes (spontaneous or artificial) engaged vertex presenting part cervical dilatation of at least 1-2cm patient’s consent and ability to cooperate with sterile vaginal examination Contraindications Contraindications for use include the following: diagnosed or suspected placenta praevia undiagnosed vaginal bleeding non-rupture of amniotic membranes maternal infection (chorioamnionitis, active genital herpes, HIV) non-vertex fetal presentation any condition that precludes vaginal delivery Issues to Consider Potential complications for consideration infection postpartum endomyometritis uterine perforation umbilical core perforation CPP0487-Fetal Surveillance May 2019 cord entanglement extra-membranous catheter placement leading to complications (e.g. placental abruption, fetal distress, disseminated intravascular coagulation, and rarely anaphylactoid syndrome) Considerations To be discussed with the consultant on call and only inserted by senior registrar or consultant who is experienced in the procedure The intrauterine pressure catheter (IUPC) should not be left in situ for longer than 24 hours. Prior to attempting insertion the manufacturer’s product instructions should be read - different companies may have product insertion variations.