P14 Protein Expression Is a Predictor of Both Relapse and Survival In
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

Mitosis Vs. Meiosis
Mitosis vs. Meiosis In order for organisms to continue growing and/or replace cells that are dead or beyond repair, cells must replicate, or make identical copies of themselves. In order to do this and maintain the proper number of chromosomes, the cells of eukaryotes must undergo mitosis to divide up their DNA. The dividing of the DNA ensures that both the “old” cell (parent cell) and the “new” cells (daughter cells) have the same genetic makeup and both will be diploid, or containing the same number of chromosomes as the parent cell. For reproduction of an organism to occur, the original parent cell will undergo Meiosis to create 4 new daughter cells with a slightly different genetic makeup in order to ensure genetic diversity when fertilization occurs. The four daughter cells will be haploid, or containing half the number of chromosomes as the parent cell. The difference between the two processes is that mitosis occurs in non-reproductive cells, or somatic cells, and meiosis occurs in the cells that participate in sexual reproduction, or germ cells. The Somatic Cell Cycle (Mitosis) The somatic cell cycle consists of 3 phases: interphase, m phase, and cytokinesis. 1. Interphase: Interphase is considered the non-dividing phase of the cell cycle. It is not a part of the actual process of mitosis, but it readies the cell for mitosis. It is made up of 3 sub-phases: • G1 Phase: In G1, the cell is growing. In most organisms, the majority of the cell’s life span is spent in G1. • S Phase: In each human somatic cell, there are 23 pairs of chromosomes; one chromosome comes from the mother and one comes from the father. -

Interaction of Cdc2 and Rum1 Regulates Start and S-Phase in Fission Yeast
Journal of Cell Science 108, 3285-3294 (1995) 3285 Printed in Great Britain © The Company of Biologists Limited 1995 JCS8905 Interaction of cdc2 and rum1 regulates Start and S-phase in fission yeast Karim Labib1,2,3, Sergio Moreno3 and Paul Nurse1,2,* 1ICRF Cell Cycle Laboratory, Department of Biochemistry, University of Oxford, Oxford, OX1 1QU, UK 2ICRF, PO Box 123, Lincolns Inn Fields, London WC2A 3PX, UK 3Instituto de Microbiologia-Bioquimica, CSIC/Universidad de Salamanca, Edificio Departamental, Campus Miguel de Unamuno, 37007 Salamanca, Spain *Author for correspondence SUMMARY The p34cdc2 kinase is essential for progression past Start in rum1, can disrupt the dependency of S-phase upon mitosis, the G1 phase of the fission yeast cell cycle, and also acts in resulting in an extra round of S-phase in the absence of G2 to promote mitotic entry. Whilst very little is known mitosis. We show that cdc2 and rum1 interact in this about the G1 function of cdc2, the rum1 gene has recently process, and describe dominant cdc2 mutants causing been shown to encode an important regulator of Start in multiple rounds of S-phase in the absence of mitosis. We fission yeast, and a model for rum1 function suggests that suggest that interaction of rum1 and cdc2 regulates Start, it inhibits p34cdc2 activity. Here we present genetic data and this interaction is important for the regulation of S- cdc2 suggesting that rum1 maintains p34 in a pre-Start G1 phase within the cell cycle. form, inhibiting its activity until the cell achieves the critical mass required for Start, and find that in the absence of rum1 p34cdc2 has increased Start activity in vivo. -

The Cell Cycle & Mitosis
The Cell Cycle & Mitosis Cell Growth The Cell Cycle is G1 phase ___________________________________ _______________________________ During the Cell Cycle, a cell ___________________________________ ___________________________________ Anaphase Cell Division ___________________________________ Mitosis M phase M ___________________________________ S phase replication DNA Interphase Interphase is ___________________________ ___________________________________ G2 phase Interphase is divided into three phases: ___, ___, & ___ G1 Phase S Phase G2 Phase The G1 phase is a period of The S phase replicates During the G2 phase, many of activity in which cells _______ ________________and the organelles and molecules ____________________ synthesizes _______ molecules. required for ____________ __________ Cells will When DNA replication is ___________________ _______________ and completed, _____________ When G2 is completed, the cell is synthesize new ___________ ____________________ ready to enter the ____________________ ____________________ ____________________ ____________________ ____________________ Mitosis are divided into four phases: _____________, ______________, _____________, & _____________ Below are cells in two different phases of the cell cycle, fill in the blanks using the word bank: Chromatin Nuclear Envelope Chromosome Sister Chromatids Nucleolus Spinder Fiber Centrosome Centrioles 5.._________ 1.__________ v 6..__________ 2.__________ 7.__________ 3.__________ 8..__________ 4.__________ v The Cell Cycle & Mitosis Microscope Lab: -

Label the Parts of the Cell Cycle Diagram and Briefly Describe What Is Happening: a B C D E F G H I J 1) Chromosomes Move To
Label the parts of the cell cycle diagram and briefly describe what is happening: A Interphase - cell is growing and preparing for division. B G1 - growth and normal cell function C S - DNA replication D G2 - growth, preparation for division, duplicate organelles E Prophase - nuclear envelope dissolves, mitotic apparatus set up, DNA condenses. F Metaphase - chromosome line up in center G Anaphase - sister chromatids separate and are pulled to poles of cell. H Telophase - nuclei reform, DNA relaxes into chromatin, cleaveage furrow or cell plate forms I Mitosis - nuclear division J Cytokinesis - the rest of the cell divides 1) Chromosomes move to the middle of the cell during what phase? 2) What are sister chromatids? 3) What holds the chromatids together? 4) When do the sister chromatids separate? 5) During which phase do chromosomes first become visible? 6) During which phase does the cleavage furrow start forming? 7) What is another name for mitosis? 8) What is the structure that breaks the spindle fiber into 2? 9) What makes up the mitotic apparatus? 10) Complete the table by checking the correct column for each statement. Statement Interphase Mitosis Cell growth occurs Nuclear division occurs Chromosomes are finishing moving into separate daughter cells. Normal functions occur Chromosomes are duplicated DNA synthesis occurs Cytoplasm divides immediately after this period Mitochondria and other organelles are made. The Animal Cell Cycle – Phases are out of order 11) Which cell is in metaphase? 12) Cells A and F show an early and late stage of the same phase of mitosis. What phase is it? 13) In cell A, what is the structure labeled X? 14) In cell F, what is the structure labeled Y? 15) Which cell is not in a phase of mitosis? 16) A new membrane is forming in B. -

List, Describe, Diagram, and Identify the Stages of Meiosis
Meiosis and Sexual Life Cycles Objective # 1 In this topic we will examine a second type of cell division used by eukaryotic List, describe, diagram, and cells: meiosis. identify the stages of meiosis. In addition, we will see how the 2 types of eukaryotic cell division, mitosis and meiosis, are involved in transmitting genetic information from one generation to the next during eukaryotic life cycles. 1 2 Objective 1 Objective 1 Overview of meiosis in a cell where 2N = 6 Only diploid cells can divide by meiosis. We will examine the stages of meiosis in DNA duplication a diploid cell where 2N = 6 during interphase Meiosis involves 2 consecutive cell divisions. Since the DNA is duplicated Meiosis II only prior to the first division, the final result is 4 haploid cells: Meiosis I 3 After meiosis I the cells are haploid. 4 Objective 1, Stages of Meiosis Objective 1, Stages of Meiosis Prophase I: ¾ Chromosomes condense. Because of replication during interphase, each chromosome consists of 2 sister chromatids joined by a centromere. ¾ Synapsis – the 2 members of each homologous pair of chromosomes line up side-by-side to form a tetrad consisting of 4 chromatids: 5 6 1 Objective 1, Stages of Meiosis Objective 1, Stages of Meiosis Prophase I: ¾ During synapsis, sometimes there is an exchange of homologous parts between non-sister chromatids. This exchange is called crossing over. 7 8 Objective 1, Stages of Meiosis Objective 1, Stages of Meiosis (2N=6) Prophase I: ¾ the spindle apparatus begins to form. ¾ the nuclear membrane breaks down: Prophase I 9 10 Objective 1, Stages of Meiosis Objective 1, 4 Possible Metaphase I Arrangements: Metaphase I: ¾ chromosomes line up along the equatorial plate in pairs, i.e. -
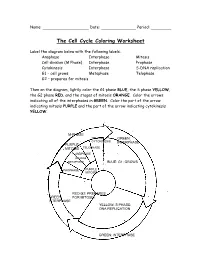
The Cell Cycle Coloring Worksheet
Name: Date: Period: The Cell Cycle Coloring Worksheet Label the diagram below with the following labels: Anaphase Interphase Mitosis Cell division (M Phase) Interphase Prophase Cytokinesis Interphase S-DNA replication G1 – cell grows Metaphase Telophase G2 – prepares for mitosis Then on the diagram, lightly color the G1 phase BLUE, the S phase YELLOW, the G2 phase RED, and the stages of mitosis ORANGE. Color the arrows indicating all of the interphases in GREEN. Color the part of the arrow indicating mitosis PURPLE and the part of the arrow indicating cytokinesis YELLOW. M-PHASE YELLOW: GREEN: CYTOKINESIS INTERPHASE PURPLE: TELOPHASE MITOSIS ANAPHASE ORANGE METAPHASE BLUE: G1: GROWS PROPHASE PURPLE MITOSIS RED:G2: PREPARES GREEN: FOR MITOSIS INTERPHASE YELLOW: S PHASE: DNA REPLICATION GREEN: INTERPHASE Use the diagram and your notes to answer the following questions. 1. What is a series of events that cells go through as they grow and divide? CELL CYCLE 2. What is the longest stage of the cell cycle called? INTERPHASE 3. During what stage does the G1, S, and G2 phases happen? INTERPHASE 4. During what phase of the cell cycle does mitosis and cytokinesis occur? M-PHASE 5. During what phase of the cell cycle does cell division occur? MITOSIS 6. During what phase of the cell cycle is DNA replicated? S-PHASE 7. During what phase of the cell cycle does the cell grow? G1,G2 8. During what phase of the cell cycle does the cell prepare for mitosis? G2 9. How many stages are there in mitosis? 4 10. Put the following stages of mitosis in order: anaphase, prophase, metaphase, and telophase. -

Working on Genomic Stability: from the S-Phase to Mitosis
G C A T T A C G G C A T genes Review Working on Genomic Stability: From the S-Phase to Mitosis Sara Ovejero 1,2,3,* , Avelino Bueno 1,4 and María P. Sacristán 1,4,* 1 Instituto de Biología Molecular y Celular del Cáncer (IBMCC), Universidad de Salamanca-CSIC, Campus Miguel de Unamuno, 37007 Salamanca, Spain; [email protected] 2 Institute of Human Genetics, CNRS, University of Montpellier, 34000 Montpellier, France 3 Department of Biological Hematology, CHU Montpellier, 34295 Montpellier, France 4 Departamento de Microbiología y Genética, Universidad de Salamanca, Campus Miguel de Unamuno, 37007 Salamanca, Spain * Correspondence: [email protected] (S.O.); [email protected] (M.P.S.); Tel.: +34-923-294808 (M.P.S.) Received: 31 January 2020; Accepted: 18 February 2020; Published: 20 February 2020 Abstract: Fidelity in chromosome duplication and segregation is indispensable for maintaining genomic stability and the perpetuation of life. Challenges to genome integrity jeopardize cell survival and are at the root of different types of pathologies, such as cancer. The following three main sources of genomic instability exist: DNA damage, replicative stress, and chromosome segregation defects. In response to these challenges, eukaryotic cells have evolved control mechanisms, also known as checkpoint systems, which sense under-replicated or damaged DNA and activate specialized DNA repair machineries. Cells make use of these checkpoints throughout interphase to shield genome integrity before mitosis. Later on, when the cells enter into mitosis, the spindle assembly checkpoint (SAC) is activated and remains active until the chromosomes are properly attached to the spindle apparatus to ensure an equal segregation among daughter cells. -

Cell Life Cycle and Reproduction the Cell Cycle (Cell-Division Cycle), Is a Series of Events That Take Place in a Cell Leading to Its Division and Duplication
Cell Life Cycle and Reproduction The cell cycle (cell-division cycle), is a series of events that take place in a cell leading to its division and duplication. The main phases of the cell cycle are interphase, nuclear division, and cytokinesis. Cell division produces two daughter cells. In cells without a nucleus (prokaryotic), the cell cycle occurs via binary fission. Interphase Gap1(G1)- Cells increase in size. The G1checkpointcontrol mechanism ensures that everything is ready for DNA synthesis. Synthesis(S)- DNA replication occurs during this phase. DNA Replication The process in which DNA makes a duplicate copy of itself. Semiconservative Replication The process in which the DNA molecule uncoils and separates into two strands. Each original strand becomes a template on which a new strand is constructed, resulting in two DNA molecules identical to the original DNA molecule. Gap 2(G2)- The cell continues to grow. The G2checkpointcontrol mechanism ensures that everything is ready to enter the M (mitosis) phase and divide. Mitotic(M) refers to the division of the nucleus. Cell growth stops at this stage and cellular energy is focused on the orderly division into daughter cells. A checkpoint in the middle of mitosis (Metaphase Checkpoint) ensures that the cell is ready to complete cell division. The final event is cytokinesis, in which the cytoplasm divides and the single parent cell splits into two daughter cells. Reproduction Cellular reproduction is a process by which cells duplicate their contents and then divide to yield multiple cells with similar, if not duplicate, contents. Mitosis Mitosis- nuclear division resulting in the production of two somatic cells having the same genetic complement (genetically identical) as the original cell. -
Cell Division for Growth of Eukaryotic Organisms and Replacement of Some Eukaryotic Cells
Mitosis CELL DIVISION FOR GROWTH OF EUKARYOTIC ORGANISMS AND REPLACEMENT OF SOME EUKARYOTIC CELLS T H I S WORK IS LICENSED UNDER A CREATIVE COMMONS ATTRIBUTION - NONCOMMERCIAL - SHAREALIKE 4 . 0 INTERNATIONAL LICENSE . History of Understanding Cancer Rudolf Virchow (1821-1902) – First to recognize leukemia in mid-1800s, believing that diseased tissue was caused by a breakdown within the cell and not from an invasion of foreign organisms. Louis Pasteur (1822-1895) – Proved Virchow to be correct in late 1800s. Virchow’s understanding that cancer cells start out normal and then become abnormal is still used today. If cancer is the study of abnormal cell division, let’s look at normal cell division. Types of Normal Cell Division There are two types of normal cell division – mitosis and meiosis. Mitosis is cell division which begins in the fertilized egg (or zygote) stage and continues during the life of the organism in one way or another. Each diploid (2n) daughter cell is genetically identical to the diploid (2n) parent cell. Meiosis is cell division in the ovaries of the female and testes of the male and involves the formation of egg and sperm cells, respectively. Each diploid (2n) parent cell produces haploid (n) daughter cells. Meiosis will be discussed more fully in Chapter 5 of the Oncofertility Curriculum. Walther Flemming (1843 – 1905) • Described the process of cell division in 1882 and coined the word ‘mitosis’ • Also responsible for the word “chromosome’ which he first referred to as stained strands • Co-worker Eduard Strasburger -

Cell Cycle the Cell Cycle Is the Period of Time from the Beginning of One
7/22/2009 As you grow from an infant to an adult, you pass through different stages of your life cycle. • Similarly, a cell passes Cell Cycle through different stages of its life. • The life cycle of a cell is Cells divide to increase their numbers called the cell cycle. through a process of mitosis, which results in two daughter cells with identical sets of chromosomes. The cell cycle is the period of time from The longest stage of the cell cycle is the beginning of one cell division to the called interphase. beginning of the next. • Interphase is the stage It consists of three stages: that occurs in between cell 1. interphase divisions. 2. mitosis • During interphase, the cell 3. cytokinesis grows and develops and performs its functions. Toward the end of interphase (just The second stage of the cell cycle is before the cell begins to divide), the called mitosis (splitting of the nucleus). amount of DNA doubles. • Mitosis is the process in cell division where • Organelles of the cytoplasm (like the nucleus divides mitochondria) also double in number. into two nuclei, each with an identical set of chromosomes. • Mitosis is divided into four phases: prophase, metaphase, anaphase, and telophase. 1 7/22/2009 The shortest stage of the cell cycle is called Mitosis cytokinesis (division of the cytoplasm). • In cytokinesis, the cytoplasm and its organelles divide into two daughter cells. – Each daughter cell contains a nucleus with an identical set of chromosomes. • The two daughter cells then start their own cycles, beginning again with the interphase stage. -

Targeting Cyclin-Dependent Kinases in Human Cancers: from Small Molecules to Peptide Inhibitors
Cancers 2015, 7, 179-237; doi:10.3390/cancers7010179 OPEN ACCESS cancers ISSN 2072-6694 www.mdpi.com/journal/cancers Review Targeting Cyclin-Dependent Kinases in Human Cancers: From Small Molecules to Peptide Inhibitors Marion Peyressatre †, Camille Prével †, Morgan Pellerano and May C. Morris * Institut des Biomolécules Max Mousseron, IBMM-CNRS-UMR5247, 15 Av. Charles Flahault, 34093 Montpellier, France; E-Mails: [email protected] (M.P.); [email protected] (C.P.); [email protected] (M.P.) † These authors contributed equally to this work. * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +33-04-1175-9624; Fax: +33-04-1175-9641. Academic Editor: Jonas Cicenas Received: 17 December 2014 / Accepted: 12 January 2015 / Published: 23 January 2015 Abstract: Cyclin-dependent kinases (CDK/Cyclins) form a family of heterodimeric kinases that play central roles in regulation of cell cycle progression, transcription and other major biological processes including neuronal differentiation and metabolism. Constitutive or deregulated hyperactivity of these kinases due to amplification, overexpression or mutation of cyclins or CDK, contributes to proliferation of cancer cells, and aberrant activity of these kinases has been reported in a wide variety of human cancers. These kinases therefore constitute biomarkers of proliferation and attractive pharmacological targets for development of anticancer therapeutics. The structural features of several of these kinases have been elucidated and their molecular mechanisms of regulation characterized in depth, providing clues for development of drugs and inhibitors to disrupt their function. However, like most other kinases, they constitute a challenging class of therapeutic targets due to their highly conserved structural features and ATP-binding pocket. -

Utimmunohistochemical Detection of the Alternate Ink4a-Encoded
utImmunohistochemical Detection of the Alternate INK4a-Encoded Tumor Suppressor Protein p14ARF in Archival Human Cancers and Cell Lines Using Commercial Antibodies: Correlation with p16INK4a Expression Joseph Geradts, M.D., Robb E. Wilentz, M.D., Helen Roberts, B.Sc. Nuffield Department of Clinical Laboratory Sciences (JG, HR), University of Oxford, John Radcliffe Hospital, Oxford, UK; and Department of Pathology (REW), The Johns Hopkins University School of Medicine, Baltimore, Maryland KEY WORDS: Antibodies, Immunohistochemistry, The INK4a locus encodes two structurally unrelated INK4a, p14ARF, p16INK4a. tumor suppressor proteins, p16INK4a and p14ARF. Mod Pathol 2001;14(11):1162–1168 Although the former is one of the most common targets for inactivation in human neoplasia, the fre- The INK4a gene on chromosome 9p21 is one of the quency of p14ARF abrogation is not established. We most common targets for inactivation in human have developed an immunohistochemical assay neoplasia. The gene is unusual in that it encodes that allows the evaluation of p14ARF expression in two structurally unrelated proteins, p16INK4a and formalin-fixed, paraffin-embedded tissues, using p14ARF, the human homologue of murine p19ARF. commercially available antibodies. p14ARF positive Two different first exons are spliced in different cells showed nuclear/nucleolar staining, which was reading frames to common exon 2 (1). p16INK4a acts absent in all cell lines and tumors with homozygous as a retinoblastoma protein (pRB) agonist by inhib- deletions of the INK4a gene. The assay was applied iting the phosphorylation of pRB by activated to 34 paraffin-embedded cell buttons, 30 non-small cyclin-dependent kinases 4 and 6 (2). The principal INK4a cell lung cancers and 28 pancreatic carcinomas, and methods of p16 inactivation are homozygous the staining results were correlated with p16INK4a deletion of the gene, promoter methylation of exon ARF 1␣, and intragenic mutation (3).