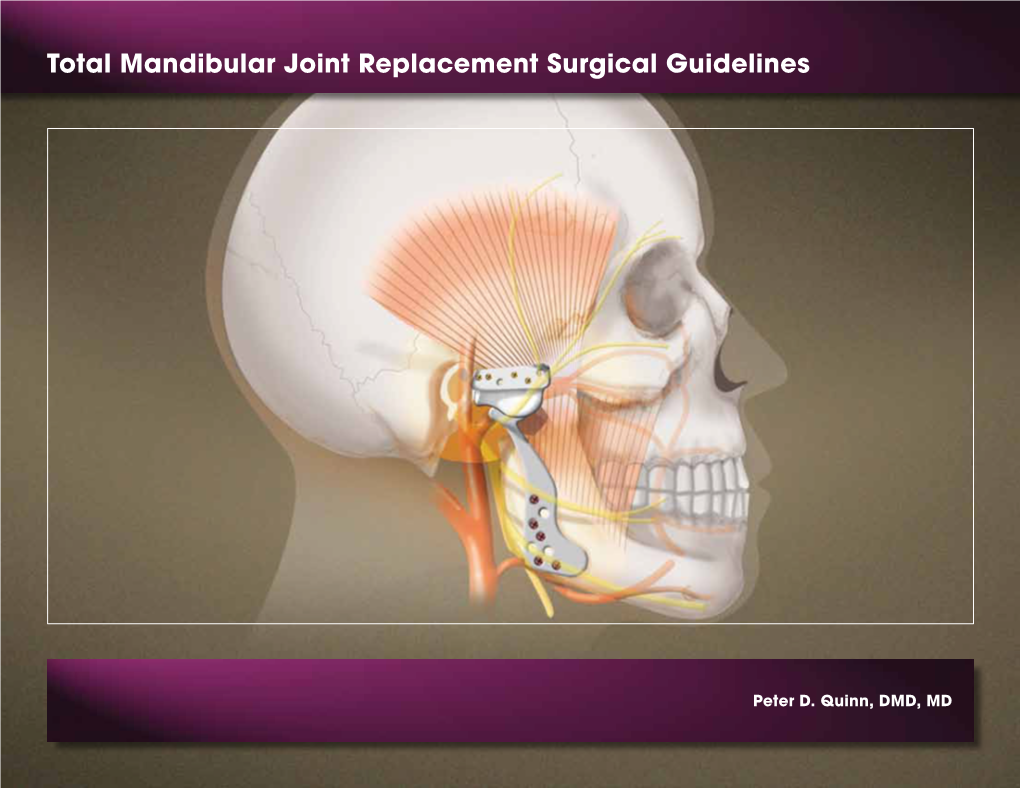
Total Mandibular Joint Replacement Surgical Guidelines
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Volume 15, Issue 1, January-April
Volume 15, Issue 1, January-April Osteochondral lesions of the talus in adults J. Batista, G. Joannas, L. Casola, L. Logioco, G. Arrondo 1A Traumatic lesion with isolated cartilage injury (flap) Tx: arthroscopy, curettage, and microfractures. 1B Traumatic lesion (cartilage and subchondral bone injury) 1B.1 Lesion <10mm in diameter and <5mm of depth (superficial lesion) Tx: arthroscopy, curettage, and microfractures. 1B.2 Lesion >10mm in diameter and >5mm in depth Tx: fragment fixation with osteosynthesis, open surgery, osteochondral graft, or mosaicoplasty. 2A Non-traumatic isolated bone injury, subchondral cyst. Tx: retrograde drilling. 2B Non-traumatic open subchondral bone cyst with articular connection (progression of type 2A). 2B.1 Lesion measuring <10mm in diameter and <5mm in depth (superficial lesion). Tx: arthroscopy, curettage, and microfractures. 2B.2 Lesion measuring >10mm in diameter and >5mm in depth. Tx: open surgery, osteochondral graft, or mosaicoplasty. 3 Type 1 or 2 lesions associated with lateral instability of the ankle Tx: ligament repair. 4 With limb deformities 4A Types 1 or 2 lesions with hindfoot deformity = varus or valgus calcaneus Tx: varus or valgus calcaneal osteotomy. 4B Type 1 or 2 lesion with supramalleolar deformity of distal tibia (varus or valgus) Tx: varus or valgus supramalleolar osteotomy. Tx: treatment. Volume 15, Issue 1, January-April The Journal of the Foot & Ankle (eISSN 2675-2980) is published quarterly in April, August, and December, with the purpose of disseminating papers on themes of Foot and Ankle Medicine and Surgery and related areas. The Journal offers free and open access to your content on our website. All papers are already published with active DOIs. -

Anterior Reconstruction Techniques for Cervical Spine Deformity
Neurospine 2020;17(3):534-542. Neurospine https://doi.org/10.14245/ns.2040380.190 pISSN 2586-6583 eISSN 2586-6591 Review Article Anterior Reconstruction Techniques Corresponding Author for Cervical Spine Deformity Samuel K. Cho 1,2 1 1 1 https://orcid.org/0000-0001-7511-2486 Murray Echt , Christopher Mikhail , Steven J. Girdler , Samuel K. Cho 1Department of Orthopedics, Icahn School of Medicine at Mount Sinai, New York, NY, USA Department of Orthopaedics, Icahn 2 Department of Neurological Surgery, Montefiore Medical Center/Albert Einstein College of Medicine, Bronx, School of Medicine at Mount Sinai, 425 NY, USA West 59th Street, 5th Floor, New York, NY, USA E-mail: [email protected] Cervical spine deformity is an uncommon yet severely debilitating condition marked by its heterogeneity. Anterior reconstruction techniques represent a familiar approach with a range Received: June 24, 2020 of invasiveness and correction potential—including global or focal realignment in the sagit- Revised: August 5, 2020 tal and coronal planes. Meticulous preoperative planning is required to improve or prevent Accepted: August 17, 2020 neurologic deterioration and obtain satisfactory global spinal harmony. The ability to per- form anterior only reconstruction requires mobility of the opposite column to achieve cor- rection, unless a combined approach is planned. Anterior cervical discectomy and fusion has limited focal correction, but when applied over multiple levels there is a cumulative ef- fect with a correction of approximately 6° per level. Partial or complete corpectomy has the ability to correct sagittal deformity as well as decompress the spinal canal when there is an- terior compression behind the vertebral body. -

ERAS for Hip and Knee (THA and TKA) Arthroplasty – a Need to Look Beyond LOS
ASERalert November 2016 | Volume 1, Issue 1 ERAS for Hip and Knee (THA and TKA) Arthroplasty – A Need to Look Beyond LOS OFFICIAL also in this issue PUBLICATION OF ERAS for Total Enhanced ERAS for Spine Joint Arthroplasty: Recovery for Surgery: A New Past, Present and Orthopedic Frontier ASER ALERT • VOLUME 1, ISSUE 1 • aserhq.org Future Surgery 1 ANNUAL CONGRESS OF ENHANCED RECOVERY AND 2017 PERIOPERATIVE MEDICINE APRIL 27TH-29TH, 2017 HYATT REGENCY WASHINGTON ON CAPITOL HILL 400 NEW JERSEY AVE NW, WASHINGTON, D.C. 20001 For more information please visit www.aserhq.org 2 ASER ALERT • VOLUME 1, ISSUE 1 • aserhq.org Board of Directors President’s Message Officers By Tong J (TJ) Gan, MD, MHS, FRCA, President President Tong J (TJ) Gan, MD, MHS, FRCA President-Elect Julie Thacker, MD t is my great pleasure to announce Vice-President the inaugural issue of the ASER Timothy Miller MB, ChB, FRCA Newsletter. Founded in 2014, Treasurer ASER is a multi-specialty nonprofit Roy Soto, MD Iorganization with an international Secretary membership and is dedicated to the Stefan D. Holubar MD, MS, FACS, FASCRS practice of enhanced recovery in the perioperative patient through education Directors and research. We are experiencing a period of tremendous expansion and Keith A. (Tony) Jones, MD growth, as is evidenced by the great Anthony Senagore, MD interest to implement the enhanced Maxime Cannesson, MD, PhD recovery pathway in hospitals around Terrence Loftus, MD, MBA, FACS the country. Andrew Shaw MB, FRCA, FFICM, FCCM Desiree Chappel, CRNA The ASER Mission is to advance the practice of perioperative enhanced recovery and to contribute to its pathways. -

Total Joint Replacement Hip and Knee Pain Pinnacle Orthopedics Pinnacle Medical Network Total Joint Replacement
Total Joint Replacement Hip and Knee Pain Pinnacle Orthopedics Pinnacle Medical Network Total Joint Replacement About Pinnacle Orthopedics and Pinnacle Medical Network South Louisiana’s Premier System for the Delivery of Musculoskeletal Health Care. Our talented team and professional staff offer a fully- equipped facility for the comprehensive care of your bones, joints, ligaments and muscles. Our team is dedicated to your complete care, from assessment to full recovery. Our primary goal is your safe return to work, sports, play and the activities of daily living. Allow our medical professionals to advance your orthopedic care. Total Joint Replacement “It would be embarrassing to get out of a car because everybody had to help me. Somebody would have to pull me up. I felt like this old woman.” “My life got progressively less active, less fun, and less participative.” “Just a day on my feet was exhausting and the pain became greater and greater until Advil and ibuprofen and all of those kinds of drugs couldn't numb it out. It just got worse and worse.” Total Joint Replacement Does this sound familiar? Total Joint Replacement You’re Not Alone More than 43 million people have some form of arthritis. It is estimated that the number of people affected by arthritis will increase to 60 million by 2020. Source: CDC Total Joint Replacement This information will touch upon the following topics: Understanding the Causes of Joint Pain Treatment Options What Joint Replacement Surgery Involves Realistic Expectations After Joint Replacement Total Joint Replacement Total Joint Replacement Total Joint Replacement Did you know? Nearly 21 million Americans suffer from osteoarthritis, a degenerative joint disease that is a leading cause of joint replacement surgery. -
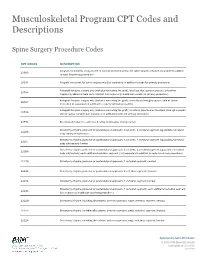
Musculoskeletal Program CPT Codes and Descriptions
Musculoskeletal Program CPT Codes and Descriptions Spine Surgery Procedure Codes CPT CODES DESCRIPTION Allograft, morselized, or placement of osteopromotive material, for spine surgery only (List separately in addition 20930 to code for primary procedure) 20931 Allograft, structural, for spine surgery only (List separately in addition to code for primary procedure) Autograft for spine surgery only (includes harvesting the graft); local (eg, ribs, spinous process, or laminar 20936 fragments) obtained from same incision (List separately in addition to code for primary procedure) Autograft for spine surgery only (includes harvesting the graft); morselized (through separate skin or fascial 20937 incision) (List separately in addition to code for primary procedure) Autograft for spine surgery only (includes harvesting the graft); structural, bicortical or tricortical (through separate 20938 skin or fascial incision) (List separately in addition to code for primary procedure) 20974 Electrical stimulation to aid bone healing; noninvasive (nonoperative) Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral segment (eg, pedicle/vertebral 22206 body subtraction); thoracic Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral segment (eg, pedicle/vertebral 22207 body subtraction); lumbar Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral segment (eg, pedicle/vertebral 22208 body subtraction); each additional vertebral segment (List separately in addition to code for -

Osteotomy Around the Knee: Evolution, Principles and Results
Knee Surg Sports Traumatol Arthrosc DOI 10.1007/s00167-012-2206-0 KNEE Osteotomy around the knee: evolution, principles and results J. O. Smith • A. J. Wilson • N. P. Thomas Received: 8 June 2012 / Accepted: 3 September 2012 Ó Springer-Verlag 2012 Abstract to other complex joint surface and meniscal cartilage Purpose This article summarises the history and evolu- surgery. tion of osteotomy around the knee, examining the changes Level of evidence V. in principles, operative technique and results over three distinct periods: Historical (pre 1940), Modern Early Years Keywords Tibia Osteotomy Knee Evolution Á Á Á Á (1940–2000) and Modern Later Years (2000–Present). We History Results Principles Á Á aim to place the technique in historical context and to demonstrate its evolution into a validated procedure with beneficial outcomes whose use can be justified for specific Introduction indications. Materials and methods A thorough literature review was The concept of osteotomy for the treatment of limb defor- performed to identify the important steps in the develop- mity has been in existence for more than 2,000 years, and ment of osteotomy around the knee. more recently pain has become an additional indication. Results The indications and surgical technique for knee The basic principle of osteotomy (osteo = bone, tomy = osteotomy have never been standardised, and historically, cut) is to induce a surgical transection of a bone to allow the results were unpredictable and at times poor. These realignment and a consequent transfer of weight bearing factors, combined with the success of knee arthroplasty from a damaged area to an undamaged area of joint surface. -

Periacetabular Osteotomy (PAO) of the Hip
UW HEALTH SPORTS REHABILITATION Rehabilitation Guidelines For Periacetabular Osteotomy (PAO) Of The Hip The hip joint is composed of the femur (the thigh bone) and the Lunate surface of acetabulum acetabulum (the socket formed Articular cartilage by the three pelvic bones). The Anterior superior iliac spine hip joint is a ball and socket joint Head of femur Anterior inferior iliac spine that not only allows flexion and extension, but also rotation of the Iliopubic eminence Acetabular labrum thigh and leg (Fig 1). The head of Greater trochanter (fibrocartilainous) the femur is encased by the bony Fat in acetabular fossa socket in addition to a strong, (covered by synovial) Neck of femur non-compliant joint capsule, Obturator artery making the hip an extremely Anterior branch of stable joint. Because the hip is Intertrochanteric line obturator artery responsible for transmitting the Posterior branch of weight of the upper body to the obturator artery lower extremities and the forces of Obturator membrane Ischial tuberosity weight bearing from the foot back Round ligament Acetabular artery up through the pelvis, the joint (ligamentum capitis) Lesser trochanter Transverse is subjected to substantial forces acetabular ligament (Fig 2). Walking transmits 1.3 to Figure 1 Hip joint (opened) lateral view 5.8 times body weight through the joint and running and jumping can generate forces across the joint fully form, the result can be hip that is shared by the whole hip, equal to 6 to 8 times body weight. dysplasia. This causes the hip joint including joint surfaces and the to experience load that is poorly previously-mentioned acetabular The labrum is a circular, tolerated over time, resulting in labrum. -

What Is the Impact of a Previous Femoral Osteotomy on THA?
Clin Orthop Relat Res (2019) 477:1176-1187 DOI 10.1097/CORR.0000000000000659 2018 Bernese Hip Symposium What Is the Impact of a Previous Femoral Osteotomy on THA? A Systematic Review Enrico Gallazzi MD, Ilaria Morelli MD, Giuseppe Peretti MD, Luigi Zagra MD 02/11/2020 on BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD30p/TQ0kcqx8yGZO9yTf1dd5lN9ZPVa7AUCC2fdK0Vq4= by https://journals.lww.com/clinorthop from Downloaded Downloaded from Received: 10 August 2018 / Accepted: 8 January 2019 / Published online: 17 April 2019 https://journals.lww.com/clinorthop Copyright © 2019 by the Association of Bone and Joint Surgeons Abstract by Background Femoral osteotomies have been widely used Questions/purposes In this systematic review, we asked: BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD30p/TQ0kcqx8yGZO9yTf1dd5lN9ZPVa7AUCC2fdK0Vq4= to treat a wide range of developmental and degenerative hip (1) What are the most common complications after THA in diseases. For this purpose, different types of proximal fe- patients who have undergone femoral osteotomy, and how mur osteotomies were developed: at the neck as well as at frequently do those complications occur? (2) What is the the trochanteric, intertrochanteric, or subtrochanteric lev- survival of THA after previous femoral osteotomy? (3) Is els. Few studies have evaluated the impact of a previous the timing of hardware removal associated with THA femoral osteotomy on a THA; thus, whether and how a complications and survivorship? previous femoral osteotomy affects the -

Surgical Considerations of the TMJ
Surgical Considerations of the TMJ Peter B. Franco DMD, FACS Diplomate, American Board of Oral and Maxillofacial Surgery Fellow, American College of Surgeons Carolinas Center for Oral and Facial Surgery Surgical Options of the TMJ • Arthroscopy • Open Arthroplasty – Disk preservation – Diskectomy Surgical Options of TMJ • General Indications – Significant TMJ pain or dysfunction – Non-surgical therapy has failed – Radiographic evidence of disease Failure to manage associated myofascial pain and dysfunction lowers the rate of surgical success. Arthroscopic Arthroplasty • Biopsy of suspected lesions or disease • Confirmation of other diagnostic findings that may warrant surgical treatment • Unexplained persistent joint pain that is non-responsive to medical treatment Arthroscopic Arthroplasty Indications • Closed, locked articular disc • Painful popping joint • Adhesions • Perforated disc • Hypermobile joints • Inflammatory joint disease • Hypermobility • Degenerative Joint Disease • Traumatic Injuries • Suspected Infection Arthroscopic Arthroplasty Equipment • Video/monitoring equipment • Arthroscopic cannula, scissors, forceps, probes, shavers • Laser Arthroscopic Arthroplasty Equipment • Scope • Arthroscopic cannula, scissors, forceps, probes, shavers • Laser Arthroscopic Arthroplasty Equipment • Scope • Video/monitoring equipment • Laser Arthroscopic Arthroplasty Equipment • Scope • Video/monitoring equipment • Arthroscopic cannula, scissors, forceps, probes, shavers Arthroscopic Arthroplasty Equipment Arthroscopic Arthroplasty Arthroscopic -

Indications for Unicompartmental Knee Arthroplasty and Rationale for Robotic Arm–Assisted Technology
A Review Paper Indications for Unicompartmental Knee Arthroplasty and Rationale for Robotic Arm–Assisted Technology Jess H. Lonner, MD results not dissimilar from those of total knee arthroplasty Abstract (TKA), leading to a gradual change in attitude toward UKA. Unicompartmental knee arthroplasty (UKA) is an effec- As long-term data become available, UKA is being more tive surgical treatment for focal arthritis when appropri- universally embraced as a clear and definable treatment ate selection criteria are followed. Although results can option for unicompartmental arthritis. be optimized with careful patient selection and use of a Superb clinical data and desirable kinematic perfor- sound implant design, two of the most important deter- mance support the role of UKA. Berger and colleagues3 minants of UKA performance and durability are how well the bone is prepared and components aligned. Study found that the implant survival rate for 62 consecutive results have shown that component malalignment by as UKAs performed by a skilled surgeon with a design still in little as 2° may predispose to implant failure after UKA. use today was 98% after 10 years and 96% after 13 years, Conventional cutting guides have been relatively inac- using revision and radiographic loosening as the respective curate in determining alignment and preparing the bone endpoints. Emerson and Higgins,4 reporting their personal surfaces for unicompartmental implants. Computer navi- experience with 55 mobile-bearing UKAs, noted a 90% gation has improved component alignment to an extent, rate of 10-year implant survival with progression of lateral but outliers still exist. compartment arthritis as the endpoint and 96% with com- The introduction of robotics capitalizes on the virtues of ponent loosening as the endpoint. -

A Regional Resource for Joint Replacement, Trauma, Orthopedics, Sports Medicine and Spine Problems
3688 Veterans Memorial Dr. Hattiesburg, MS 39401 appointments, referrals & 2nd opinions: 601-554-7400 Online encyclopedia about orthopedics and spine care at: SouthernBoneandJoint.com A regional resource for joint replacement, trauma, orthopedics, sports medicine and spine problems Decades ago an orthopedic provide patients the most hip and knee replacement. The advanced FDA-approved artificial surgeon would treat all types advanced technology and care technology enables the joint discs that preserve motion in the of joint problems. With ever- specific to their orthopedic injury replacement surgeon to map out spine. increasing new technology and or pain symptom. in advance of surgery the optimal Consquently, these clinical care treatment advances specific to One example is the use of new cuts in the bone for the best centers are referred patients from different joints and bones, that’s Robotic Surgery Technology. The surgical outcome and to spare as across the region. changed dramatically. Over hip and knee surgeons make use much bone as possible. Appointments, referrals and the past 15 years, orthopedics of Mako Robotic Surgery that Similarly, the spine surgeons in second opinions can be set up by has become super-specialized improves the outcomes from The Spine Center provide the most calling 601-554-7400. with surgeons now becoming fellowship-trained in a specific body part, such as foot/ankle or ORTHOPEDIC SPECIALTY CENTERS LOCATIONS hand/arm or spine. The best care comes from a specialized approach. Consequently, MAIN CLINIC LOCATION: Because of this super 3688 Veterans Memorial Drive Southern Bone and Joint Specialists is organized into CLINICAL CARE specialization in orthopedics, Hattiesburg, MS 39401 CENTERS that provides the most advanced treatment options. -

Utilization Management Policy Title: Lumbar Spine Surgeries
Medica Policy No. III-SUR.34 UTILIZATION MANAGEMENT POLICY TITLE: LUMBAR SPINE SURGERIES EFFECTIVE DATE: January 18, 2021 This policy was developed with input from specialists in orthopedic spine surgery and endorsed by the Medical Policy Committee. IMPORTANT INFORMATION – PLEASE READ BEFORE USING THIS POLICY These services may or may not be covered by all Medica plans. Please refer to the member’s plan document for specific coverage information. If there is a difference between this general information and the member’s plan document, the member’s plan document will be used to determine coverage. With respect to Medicare and Minnesota Health Care Programs, this policy will apply unless these programs require different coverage. Members may contact Medica Customer Service at the phone number listed on their member identification card to discuss their benefits more specifically. Providers with questions about this Medica utilization management policy may call the Medica Provider Service Center toll-free at 1-800-458-5512. Medica utilization management policies are not medical advice. Members should consult with appropriate health care providers to obtain needed medical advice, care and treatment. PURPOSE To promote consistency between Utilization Management reviewers by providing the criteria that determine medical necessity. BACKGROUND I. Prevalence / Incidence A. It is reported that the lifetime incidence of low back pain (LBP) in the general population within the United States is between 60% and 90%, with an annual incidence of 5%. According to a National Center for Health Statistics study (Patel, 2007), 14.3% of new patient visits to primary care physicians per year are for LBP.