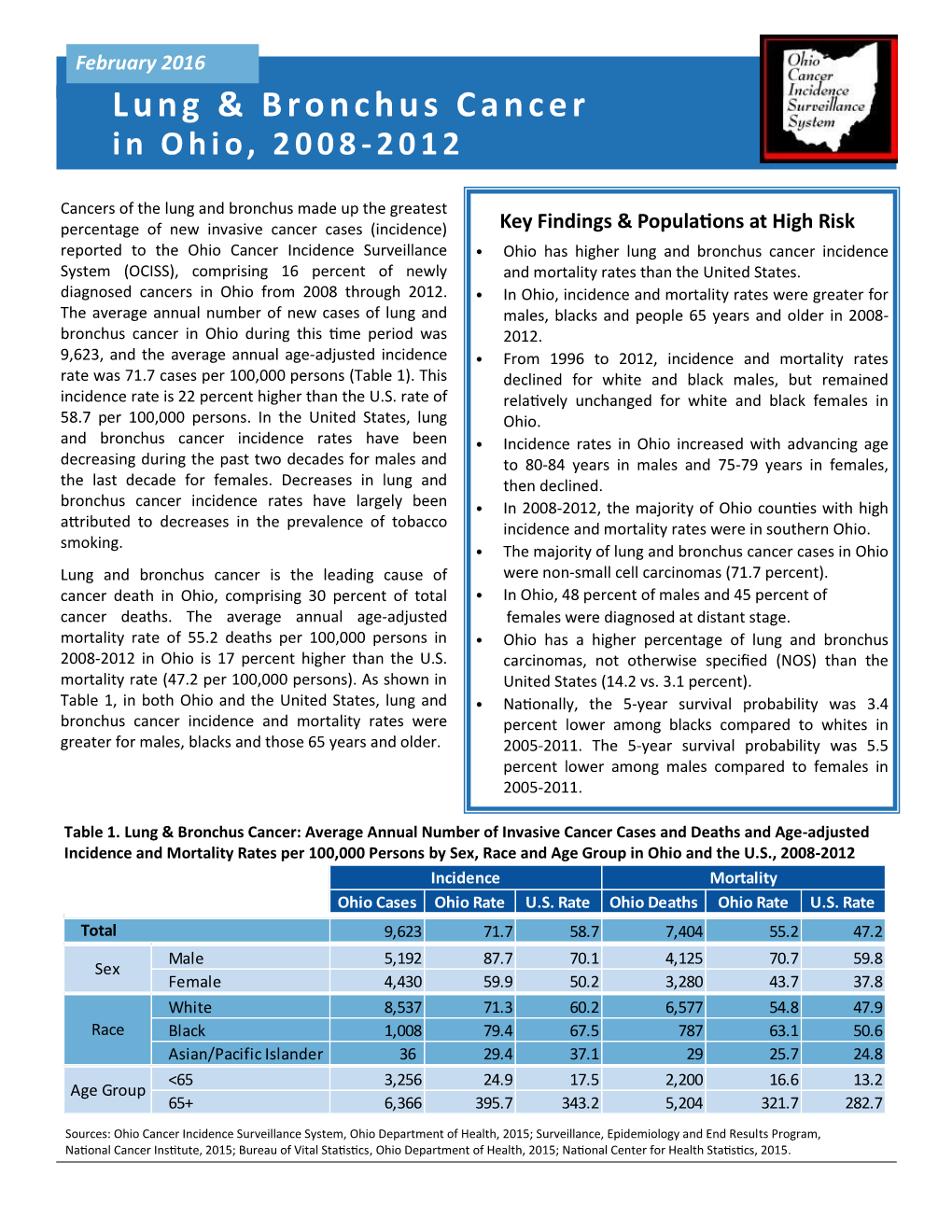
Lung & Bronchus Cancer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Lung Anatomy
Lung anatomy Breathing Breathing is an automatic and usually subconscious process which is controlled by the brain. The brain will determine how much oxygen we require and how fast we need to breathe in order to supply our vital organs (brain, heart, kidneys, liver, stomach and bowel), as well as our muscles and joints, with enough oxygen to carry out our normal daily activities. In order for breathing to be effective we need to use our lungs, breathing muscles and blood system efficiently. This leaflet should help you to better understand the process of breathing and how we get the much needed oxygen into our bodies. The lungs You have two lungs, one in the right side and one in the left side of your chest. The right lung is bigger than the left due to the position of the heart (which is positioned in the left side of the chest). Source: Pulmonary Rehabilitation Reference No: 66354-1 Issue date: 13/2/20 Review date: 13/2/23 Page 1 of 5 Both lungs are covered by 2 thin layers of tissue called the pleura. The pleura stop the surface of the lungs rubbing together as we breathe in and out. The lungs are protected by the ribcage. The airways Within the lungs there is a vast network of airways (tubes) which help to transport the oxygen into the lungs and the carbon dioxide out. These tubes branch into smaller and smaller tubes the further they go into the lungs. Page 2 of 5 Trachea (windpipe): This tube connects your nose and mouth to your lungs. -

1. Launch the View! • Launch Human Anatomy Atlas. • Navigate to Quizzes/Lab Activities, Find the Respiratory Lab Section
Name: __________________________________________________________ Date: ______________________________ Activity 1: Respiratory System Lab 1. Launch the view! • Launch Human Anatomy Atlas. • Navigate to Quizzes/Lab Activities, find the Respiratory Lab section. • Launch Augmented Reality mode and scan the image below. • Don’t have AR? Select view 1. Respiratory System. 2. Fill in the blanks. • Find the structures listed in the word bank. • Read the definitions, then fill in the blank with the correct respiratory system structure from the word bank. © Argosy Publishing, Inc., 2007-2018. All Rights Reserved. 1/2 Name: __________________________________________________________ Date: ______________________________ Word bank: • Alveoli • Nasopharynx • Bronchi • Oropharynx • Laryngopharynx • Primary bronchi • Lungs • Trachea • Nasal cavity The ______________________________ is composed of the chambers of the internal nose that function as a part of the upper respiratory system. The ______________________________ is the most posterior part of the pharynx. It is shared by the respiratory system and the digestive system. The upper respiratory and upper digestive tracts diverge right after this structure. The front of this structure merges with the triangular entrance of the larynx. The ______________________________ conveys air between the upper and lower respiratory structures. The ______________________________ is a portion of the pharynx that begins at the rear of the nasal cavity and functions as an airway in the upper respiratory system. Its cavity always stays open, unlike the other parts of the pharynx. The ______________________________ are two organs that are responsible for gas exchange. The ______________________________ are the major airways of the lower respiratory system. The ______________________________ are the main sites of gas exchange, where oxygen is brought into the bloodstream and carbon dioxide is removed. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Lung Microbiome Participation in Local Immune Response Regulation in Respiratory Diseases
microorganisms Review Lung Microbiome Participation in Local Immune Response Regulation in Respiratory Diseases Juan Alberto Lira-Lucio 1 , Ramcés Falfán-Valencia 1 , Alejandra Ramírez-Venegas 2, Ivette Buendía-Roldán 3 , Jorge Rojas-Serrano 4 , Mayra Mejía 4 and Gloria Pérez-Rubio 1,* 1 HLA Laboratory, Instituto Nacional de Enfermedades Respiratorias Ismael Cosío Villegas, Mexico City 14080, Mexico; [email protected] (J.A.L.-L.); [email protected] (R.F.-V.) 2 Tobacco Smoking and COPD Research Department, Instituto Nacional de Enfermedades Respiratorias Ismael Cosío Villegas, Mexico City 14080, Mexico; [email protected] 3 Translational Research Laboratory on Aging and Pulmonary Fibrosis, Instituto Nacional de Enfermedades Respiratorias Ismael Cosío Villegas, Mexico City 14080, Mexico; [email protected] 4 Interstitial Lung Disease and Rheumatology Unit, Instituto Nacional de Enfermedades Respiratorias Ismael Cosío Villegas, Mexico City 14080, Mexico; [email protected] (J.R.-S.); [email protected] (M.M.) * Correspondence: [email protected]; Tel.: +52-55-5487-1700 (ext. 5152) Received: 11 June 2020; Accepted: 7 July 2020; Published: 16 July 2020 Abstract: The lung microbiome composition has critical implications in the regulation of innate and adaptive immune responses. Next-generation sequencing techniques have revolutionized the understanding of pulmonary physiology and pathology. Currently, it is clear that the lung is not a sterile place; therefore, the investigation of the participation of the pulmonary microbiome in the presentation, severity, and prognosis of multiple pathologies, such as asthma, chronic obstructive pulmonary disease, and interstitial lung diseases, contributes to a better understanding of the pathophysiology. Dysregulation of microbiota components in the microbiome–host interaction is associated with multiple lung pathologies, severity, and prognosis, making microbiome study a useful tool for the identification of potential therapeutic strategies. -

Nasal Cavity Trachea Right Main (Primary) Bronchus Left Main (Primary) Bronchus Nostril Oral Cavity Pharynx Larynx Right Lung
Nasal cavity Oral cavity Nostril Pharynx Larynx Trachea Left main Right main (primary) (primary) bronchus bronchus Left lung Right lung Diaphragm © 2018 Pearson Education, Inc. 1 Cribriform plate of ethmoid bone Sphenoidal sinus Frontal sinus Posterior nasal aperture Nasal cavity • Nasal conchae (superior, Nasopharynx middle, and inferior) • Pharyngeal tonsil • Nasal meatuses (superior, middle, and inferior) • Opening of pharyngotympanic • Nasal vestibule tube • Nostril • Uvula Hard palate Oropharynx • Palatine tonsil Soft palate • Lingual tonsil Tongue Laryngopharynx Hyoid bone Larynx Esophagus • Epiglottis • Thyroid cartilage Trachea • Vocal fold • Cricoid cartilage (b) Detailed anatomy of the upper respiratory tract © 2018 Pearson Education, Inc. 2 Pharynx • Nasopharynx • Oropharynx • Laryngopharynx (a) Regions of the pharynx © 2018 Pearson Education, Inc. 3 Posterior Mucosa Esophagus Submucosa Trachealis Lumen of Seromucous muscle trachea gland in submucosa Hyaline cartilage Adventitia (a) Anterior © 2018 Pearson Education, Inc. 4 Intercostal muscle Rib Parietal pleura Lung Pleural cavity Trachea Visceral pleura Thymus Apex of lung Left superior lobe Right superior lobe Oblique Horizontal fissure fissure Right middle lobe Left inferior lobe Oblique fissure Right inferior lobe Heart (in pericardial cavity of mediastinum) Diaphragm Base of lung (a) Anterior view. The lungs flank mediastinal structures laterally. © 2018 Pearson Education, Inc. 5 Posterior Vertebra Esophagus (in posterior mediastinum) Root of lung at hilum Right lung • Left main bronchus Parietal pleura • Left pulmonary artery • Left pulmonary vein Visceral pleura Pleural cavity Left lung Thoracic wall Pulmonary trunk Pericardial membranes Heart (in mediastinum) Sternum Anterior mediastinum Anterior (b) Transverse section through the thorax, viewed from above © 2018 Pearson Education, Inc. 6 Alveolar duct Alveoli Respiratory bronchioles Alveolar duct Terminal bronchiole Alveolar sac (a) Diagrammatic view of respiratory bronchioles, alveolar ducts, and alveoli © 2018 Pearson Education, Inc. -

GLOSSARY of MEDICAL and ANATOMICAL TERMS
GLOSSARY of MEDICAL and ANATOMICAL TERMS Abbreviations: • A. Arabic • abb. = abbreviation • c. circa = about • F. French • adj. adjective • G. Greek • Ge. German • cf. compare • L. Latin • dim. = diminutive • OF. Old French • ( ) plural form in brackets A-band abb. of anisotropic band G. anisos = unequal + tropos = turning; meaning having not equal properties in every direction; transverse bands in living skeletal muscle which rotate the plane of polarised light, cf. I-band. Abbé, Ernst. 1840-1905. German physicist; mathematical analysis of optics as a basis for constructing better microscopes; devised oil immersion lens; Abbé condenser. absorption L. absorbere = to suck up. acervulus L. = sand, gritty; brain sand (cf. psammoma body). acetylcholine an ester of choline found in many tissue, synapses & neuromuscular junctions, where it is a neural transmitter. acetylcholinesterase enzyme at motor end-plate responsible for rapid destruction of acetylcholine, a neurotransmitter. acidophilic adj. L. acidus = sour + G. philein = to love; affinity for an acidic dye, such as eosin staining cytoplasmic proteins. acinus (-i) L. = a juicy berry, a grape; applied to small, rounded terminal secretory units of compound exocrine glands that have a small lumen (adj. acinar). acrosome G. akron = extremity + soma = body; head of spermatozoon. actin polymer protein filament found in the intracellular cytoskeleton, particularly in the thin (I-) bands of striated muscle. adenohypophysis G. ade = an acorn + hypophyses = an undergrowth; anterior lobe of hypophysis (cf. pituitary). adenoid G. " + -oeides = in form of; in the form of a gland, glandular; the pharyngeal tonsil. adipocyte L. adeps = fat (of an animal) + G. kytos = a container; cells responsible for storage and metabolism of lipids, found in white fat and brown fat. -

Manatee Anatomy and Physiology
Manatee Anatomy and Physiology Grade level: Elementary 5 Subject Area: Biology, Anatomy and Physiology, Marine Biology Duration: Teach: 15 minutes, Activity: 20 minutes, Discussion: 20 minutes. Setting: Classroom Next Generation Sunshine State Standards: Reading: LAFS.5.RI Reading standards for Information text Cluster 3 LAFS.5.RI.3 Writing: LA.B.2.1, LA.B.1.2 Speaking and Listening: Cluster 2 LAFS.5.SL.Z Presentation of Knowledge and Ideas Science: Body of Knowledge Life Science: SC.5.L.14, SC.5.L.15, SC.5.L.17, Body of Knowledge Nature of Science Supporting Idea 1: SC.5.N.1 Practice of Science, Supporting Idea 2:SC.5.N.2 Characteristics of Scientific Knowledge Earth Systems and Patterns: 7SC.E.E.7 Statewide Science Assessment Prompt: How might humans help manatees survive? Objectives: Students will learn about manatee bodies and explain some anatomical and physiological differences between manatees, humans and other animals. Materials: Handouts of basic manatee anatomy, dolphin anatomy & human anatomy, crayons or markers, coloring direction sheet, question worksheet, Quiz sheet Vocabulary: Mammal, endangered species, habitat, conservation, vibrissae, nares, blowhole, flipper, herbivore, omnivore, carnivore. Background/Preparation: Handouts of manatee, dolphin, and human anatomy. Fact sheets comparing and contrasting specific and unique anatomical aspects of each species. Basic manatee fact sheet highlighting personality, limited habitat, endangered status and conservation efforts. Teachers can review the manatee fact sheets, and select points of interest they would most like to incorporate into a lesson. This activity may fit best into the week where the human anatomy lessons are addressed. Teachers can present the information via traditional lecture, group discussion, question and answer session, or doing the coloring activity as the lesson points are addressed, etc. -

The Fifth Pulmonary Vein
CASE REPORT Anatomy Journal of Africa. 2016. Vol 5 (2): 704 - 706 The Fifth Pulmonary vein Hilkiah Kinfemichael, Asrat Dawit Correspondence to Hilkiah Kinfemichael, Myungsung Medical College, Addis Ababa, Ethiopia PO Box 14972 Email : [email protected]. ABSTRACT A cadaver in Myungsung Medical College (MMC) had a 3rd pulmonary vein originating from the middle lobe of the right lung. Such anatomical variations are very rare. People with this variation have a total of five pulmonary veins entering left atrium. It has clinical implications especially for thoracic surgeons and radiologists during radiofrequency ablations, lobectomies, valve replacements, pulmonary vein catheterizations, video-assisted thoracic surgery (VATS) and others. Key Words: Anatomy, Variations, Pulmonary veins. INTRODUCTION Two pulmonary veins usually drain oxygenated upper lobe, is formed by the union of blood from each lung to left atrium of the apicoposterior, anterior and lingular veins. The heart. The lobular tributaries lie mainly in the inferior left pulmonary vein, which drains the interlobular septa and two pulmonary veins lower lobe, is formed by the hilar union of two from each lung enter left atrium through two veins, superior and common basal veins. The separate pulmonary ostia on either side. On the right and left pulmonary veins perforate the right lung veins from the apical, anterior and fibrous pericardium and open separately in the posterior part of upper lobe unite with a middle posterosuperior aspect of the left atrium lobar vein, which is formed by lateral and (Standring et al., 2008). This anatomy could medial tributaries, and form the superior right show variations, with more veins draining pulmonary vein (Standring, 2008). -
The Respiratory System
Respiratory Rehabilitation Program The Respiratory System Every cell in the body needs oxygen to survive. The respiratory system provides a way for oxygen to enter the body. It also provides a way for carbon dioxide, the waste product of cells, to leave the body. The respiratory system is made up of 2 sections: the upper respiratory tract and the lower respiratory tract mouth and nose larynx or voice box trachea The Upper Respiratory Tract Mouth and Nose Air enters the body through your mouth and nose. The air is warmed, moistened and filtered by mucous secretions and hairs in the nose. Larynx or Voice Box The larynx sits at the top of the trachea. It contains your vocal cords. Each time you breathe in or inhale, the air passes through the larynx, down the trachea and into the lungs. When you breathe out or exhale, the air moves from your lungs, up your trachea and out through your nose and mouth. When you speak, the vocal cords tighten up and move closer together. Air from the lungs is forced between them and causes them to vibrate. This produces sound. Your tongue, lips and teeth form words out of these sounds. Trachea The trachea is the tube that connects the mouth and nose to your lungs. It is also called the windpipe. The Lower Respiratory Tract Inside Lungs Outside Lungs bronchial tubes alveoli diaphragm (muscle) Bronchial Tubes The trachea splits into 2 bronchial tubes in your lungs. These are called the left bronchus and right bronchus. The bronchus tubes keep branching off into smaller and smaller tubes called bronchi. -

Lung Lobe Segmentation Based on Lung Fissure Surface Classification
algorithms Article Lung Lobe Segmentation Based on Lung Fissure Surface Classification Using a Point Cloud Region Growing Approach Xin Chen 1, Hong Zhao 2 and Ping Zhou 3,* 1 College of Electrical and Information Engineering, Hunan University, Changsha 410082, China; [email protected] 2 College of Aerospace Science and Engineering, National University of Defense Technology, Changsha 410003, China; [email protected] 3 College of Biology, Hunan University, Changsha 410082, China * Correspondence: [email protected] Received: 2 September 2020; Accepted: 13 October 2020; Published: 15 October 2020 Abstract: In anatomy, the lung can be divided by lung fissures into several pulmonary lobe units with specific functions. Identifying the lung lobes and the distribution of various diseases among different lung lobes from CT images is important for disease diagnosis and tracking after recovery. In order to solve the problems of low tubular structure segmentation accuracy and long algorithm time in segmenting lung lobes based on lung anatomical structure information, we propose a segmentation algorithm based on lung fissure surface classification using a point cloud region growing approach. We cluster the pulmonary fissures, transformed into point cloud data, according to the differences in the pulmonary fissure surface normal vector and curvature estimated by principal component analysis. Then, a multistage spline surface fitting method is used to fill and expand the lung fissure surface to realize the lung lobe segmentation. The proposed approach was qualitatively and quantitatively evaluated on a public dataset from Lobe and Lung Analysis 2011 (LOLA11), and obtained an overall score of 0.84. Although our approach achieved a slightly lower overall score compared to the deep learning based methods (LobeNet_V2 and V-net), the inter-lobe boundaries from our approach were more accurate for the CT images with visible lung fissures. -

Clay Adams Anatomical Model
3D Educational Resources LEARN ABOUT THE HUMAN BODY! The human body is an amazing living machine. It contains complex organs that perform all sorts of functions that work together to keep us alive. Find out more about how they do this in a series of fun mini-activities and demonstrations. ONTARIO CURRICULUM LINKS Through this activity, you and your students will use an anatomical model to go through a series of mini-activities and demonstrations about our body’s organs. This activity can be connected to multiple aspects of the school curriculum, our suggested link is: Grade 5: Science (Human Organ Systems) MATERIALS Grades 1 measuring cup 1 3D printout of the anatomical 5 – 9 1 tablespoon (15 mL) model or 3D files of the anatomical 2 bowls (around 1 L model and each) software* to view the files Ag e Range 1 ruler 1.65 m yarn 8 – 14 years 1 measuring tape 900 mL water 750 mL vinegar * Note: There are many free programs available to view the 3D files. Some examples include Sketchup Make (https://www.sketchup.com/download/all) and 3D Builder, which is included with Windows 10. IngeniumCanada.org INSTRUCTIONS These activities can be done either with a 3D printed anatomical model or through viewing the 3D model with a computer program. Feel free to add your own contributions and explore parts of the model not covered in this document. Assembling the Anatomical Model If you are having trouble putting together the anatomical model, you can find below a series of diagrams that should help you out. -

Patient and Physician Guide: National Lung Screening Trial (NLST)
Patient and Physician Guide: National Lung Screening Trial (NLST) What is the purpose of this guide? To explain the benefits and harms of low-dose computed tomography (CT) screening for lung cancer in people at high risk for the disease. The NLST showed a reduction in deaths from CT screening compared to chest X-ray screening. The Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial recently showed that chest X-ray screening (compared to no screening) did NOT reduce the chance of dying from lung cancer. Who participated in the NLST? Current or former cigarette smokers within the past 15 years, 55 to 74 years of age, with at least 30 pack-years of smoking [Pack-years = packs per day x number of years smoking]. Participants must have had no symptoms or signs of lung cancer or other serious medical conditions, and be medically fit for surgery. Study Findings: Low-dose CT versus Chest X-ray screening 53,454 current and former smokers were randomly assigned to be screened once a year for 3 years with low-dose CT or chest X-ray. Here’s what happened after an average of 6.5 years: Low-dose CT Chest X-ray 26,722 people 26,732 people Benefit: How did CT scans help compared to chest X-ray, an ineffective screening test? 3 in 1,000 fewer died from lung cancer 18 in 1,000 versus 21 in 1,000 5 in 1,000 fewer died from all causes 70 in 1,000 versus 75 in 1,000 Harm: What problems did CT scans cause compared to chest X-ray? 223 in 1,000 more had at least one false alarm 365 in 1,000 versus 142 in 1,000 18 in 1,000 more had a false alarm leading to an invasive such as bronchoscopy, biopsy, or surgery procedure, 25 in 1,000 versus 7 in 1,000 2 in 1,000 more had a major complication from 3 in 1,000 versus 1 in 1,000 Invasive procedures “Take home” messages Lung cancer screening with CT scans is the only screening test shown to lower the chance of dying from lung cancer.