Managing the Side Effects of Chemotherapy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Quiet Talks on Prayer
Quiet Talks on Prayer Author(s): Gordon, Samuel Dickey (1859-1936) Publisher: Grand Rapids, MI: Christian Classics Ethereal Library Description: Never has a discussion on prayer been as open and honest as it is in S.D. Gordon's Quiet Talks on Prayer. Quiet Talks brings fresh thought and insight to a topic that Christians are familiar with, but may not always understand. Gordon delves into the power, importance, and difficulties of prayerÐand uses Christ's prayer habits as a guide for our own improve- ment.This book is perfect for those yearning to improve their understanding of prayer as a spiritual discipline while strengthening their relationship with God. Luke Getz CCEL Staff Writer i Contents Title Page 1 I. The Meaning and Mission of Prayer 2 Prayer the Greatest Outlet of Power 3 Prayer the Deciding Factor in a Spirit Conflict 12 The Earth, the Battle-Field in Prayer 16 Does Prayer Influence God? 22 II. Hindrances to Prayer 30 Why the Results Fail 31 Why the Results are Delayed 37 The Great Outside Hindrance 48 III. How to Pray 57 The "How" of Relationship 58 The "How" of Method 65 The Listening Side of Prayer 73 Something about God's Will in Connection With Prayer 82 May we Pray With Assurance for the Conversion of Our Loved Ones 88 IV. Jesus' Habits of Prayer 95 Jesus' Habits of Prayer 96 Dissolving Views. 98 Deepening Shadows. 102 Under the Olive Trees. 106 A Composite Picture. 109 ii This PDF file is from the Christian Classics Ethereal Library, www.ccel.org. -

Singer Songwriter Musician Entrepreneur
enya K K Singer Songwriter Musician Entrepreneur WWW.KENYAMJMUSIC.COM Kenya's BIOGRAPHY Singer/songwriter Kenya delivers smooth, soulful vocals with a jazz influence that creates a contemporary groove. Kenya's music has charted in the US Top 30 Billboard Urban Adult Contemporary charts, Top 50 Smooth Jazz independent charts and top 10 on the independent UK Soul Chart in which her previous album My Own Skin (2015) reached the #1 spot for four consecutive weeks. Similarly, she reached the #1 spot in Chicago's R&B/Soul ReverbNation chart (August 2018) and was the 2014 recipient of the Black Women in Jazz "Best Black Female 'Rising Star' Jazz Artist" award. Opening for such recording artists as Lalah Hathaway, Rachelle Ferrell, Raul Midon, Mint Condition's Stokley Williams and Algebra Blessett, Kenya delights diverse crowds with her melodic tone and engaging stage presence. A graduate of Howard University and former member of the university's Howard Gospel Choir, Kenya is now based in Chicago and has performed internationally at noteworthy venues and festivals including Essence Festival, Capital Jazz Super Cruise, Magic CIty Smooth Jazz in the Park Series in Alabama, Washington D.C.'s Blues Alley, Denver's Dazzle Jazz Club, The Biltmore in LA, Groove NYC, Atlanta's St. James Live, The Promontory in Chicago in addition to a variety of other Chicago area venues and showcases, London's Jazz Cafe, Manchester, UK's Band on the Wall and a variety of other international settings. Kenya's most recent collaboration with legendary smooth jazz saxophonist, Gerald Albright is a rearrangement of the classic song "My Favorite Things" and is a stellar example of her progressive musical ideas and talent. -

Songs by Artist
Songs by Artist Title Title (Hed) Planet Earth 2 Live Crew Bartender We Want Some Pussy Blackout 2 Pistols Other Side She Got It +44 You Know Me When Your Heart Stops Beating 20 Fingers 10 Years Short Dick Man Beautiful 21 Demands Through The Iris Give Me A Minute Wasteland 3 Doors Down 10,000 Maniacs Away From The Sun Because The Night Be Like That Candy Everybody Wants Behind Those Eyes More Than This Better Life, The These Are The Days Citizen Soldier Trouble Me Duck & Run 100 Proof Aged In Soul Every Time You Go Somebody's Been Sleeping Here By Me 10CC Here Without You I'm Not In Love It's Not My Time Things We Do For Love, The Kryptonite 112 Landing In London Come See Me Let Me Be Myself Cupid Let Me Go Dance With Me Live For Today Hot & Wet Loser It's Over Now Road I'm On, The Na Na Na So I Need You Peaches & Cream Train Right Here For You When I'm Gone U Already Know When You're Young 12 Gauge 3 Of Hearts Dunkie Butt Arizona Rain 12 Stones Love Is Enough Far Away 30 Seconds To Mars Way I Fell, The Closer To The Edge We Are One Kill, The 1910 Fruitgum Co. Kings And Queens 1, 2, 3 Red Light This Is War Simon Says Up In The Air (Explicit) 2 Chainz Yesterday Birthday Song (Explicit) 311 I'm Different (Explicit) All Mixed Up Spend It Amber 2 Live Crew Beyond The Grey Sky Doo Wah Diddy Creatures (For A While) Me So Horny Don't Tread On Me Song List Generator® Printed 5/12/2021 Page 1 of 334 Licensed to Chris Avis Songs by Artist Title Title 311 4Him First Straw Sacred Hideaway Hey You Where There Is Faith I'll Be Here Awhile Who You Are Love Song 5 Stairsteps, The You Wouldn't Believe O-O-H Child 38 Special 50 Cent Back Where You Belong 21 Questions Caught Up In You Baby By Me Hold On Loosely Best Friend If I'd Been The One Candy Shop Rockin' Into The Night Disco Inferno Second Chance Hustler's Ambition Teacher, Teacher If I Can't Wild-Eyed Southern Boys In Da Club 3LW Just A Lil' Bit I Do (Wanna Get Close To You) Outlaw No More (Baby I'ma Do Right) Outta Control Playas Gon' Play Outta Control (Remix Version) 3OH!3 P.I.M.P. -
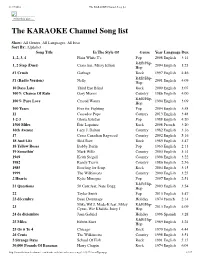
The KARAOKE Channel Song List
11/17/2016 The KARAOKE Channel Song list Print this List ... The KARAOKE Channel Song list Show: All Genres, All Languages, All Eras Sort By: Alphabet Song Title In The Style Of Genre Year Language Dur. 1, 2, 3, 4 Plain White T's Pop 2008 English 3:14 R&B/Hip- 1, 2 Step (Duet) Ciara feat. Missy Elliott 2004 English 3:23 Hop #1 Crush Garbage Rock 1997 English 4:46 R&B/Hip- #1 (Radio Version) Nelly 2001 English 4:09 Hop 10 Days Late Third Eye Blind Rock 2000 English 3:07 100% Chance Of Rain Gary Morris Country 1986 English 4:00 R&B/Hip- 100% Pure Love Crystal Waters 1994 English 3:09 Hop 100 Years Five for Fighting Pop 2004 English 3:58 11 Cassadee Pope Country 2013 English 3:48 1-2-3 Gloria Estefan Pop 1988 English 4:20 1500 Miles Éric Lapointe Rock 2008 French 3:20 16th Avenue Lacy J. Dalton Country 1982 English 3:16 17 Cross Canadian Ragweed Country 2002 English 5:16 18 And Life Skid Row Rock 1989 English 3:47 18 Yellow Roses Bobby Darin Pop 1963 English 2:13 19 Somethin' Mark Wills Country 2003 English 3:14 1969 Keith Stegall Country 1996 English 3:22 1982 Randy Travis Country 1986 English 2:56 1985 Bowling for Soup Rock 2004 English 3:15 1999 The Wilkinsons Country 2000 English 3:25 2 Hearts Kylie Minogue Pop 2007 English 2:51 R&B/Hip- 21 Questions 50 Cent feat. Nate Dogg 2003 English 3:54 Hop 22 Taylor Swift Pop 2013 English 3:47 23 décembre Beau Dommage Holiday 1974 French 2:14 Mike WiLL Made-It feat. -

SONGS to SING!!! 72 1 out of This World! NOTES Song Book
Turn the page for SONGS TO SING!!! 72 1 Out of this World! NOTES Song Book THE AARDVARK SONG………………………………………..………4 APPLES AND BANANAS………………………………………….…5 ARUSTASHA………………………………………………….…....…….5 BABY JAWS………………………………………………………….… 5 BAZOOKA BUBBLE GUM…………………………………………....6 BANANAS, COCONUTS, AND GRAPES…..………………...………7 BANANA SONG…………………………………………….………..….7 BLACK SOCKS………………………………………………………....7 BEAVER CALL………………………………………………………....8 THE BOA CONSTRICTOR…………………………………………..…9 BOOM-CHICKA-BOOM…………………………………………….…10 BROWN EYED GIRL…………………………………………………..11 BUMBLEBEE SONG………………………………………………….12 BUNGALOW……………………………………………………………13 CABIN IN THE WOODS……………………………………………….14 CAN YOU FEEL THE LOVE TONIGHT.……………………………14 CHUGGY CHUGGY….………………………………………………15 CLEAN IT UP BABY……………………………………………………15 CLEAN IT UP BABY (ROCK VERSION)……………………………16 DAY-O……………………………………………………………………17 DESPERADO………..…………………………………………………18 DOWN BY THE BAY…..………………………………………….……19 GOODNIGHT SONG….……………………………………….………20 GOOD RIDDANCE (TIME OF YOUR LIFE)………………………...21 HANDS ON MY SHELL……………………………………………….21 HERE COMES THE SUN……………………………………………...22 HERMIE THE WORM…………………………………………………23 HI, MY NAME IS JOE…………………………………………………25 HUMPTY DUMP……………………………………………………..…26 I DON’T WANT TO LIVE ON THE MOON…………………………27 I’M COMING OUT OF MY SHELL………………………………….28 JET PLANE………………………………………………………………30 2 71 NOTES LEAN ON ME……….……………………………………………….…31 THE LION SLEEPS TONIGHT….….………………………………..32 THE LITTLEST WORM……………………………………………..…33 MOMMA DON’T WEAR NO SOCKS………………………………34 HIGH HEELS…………………………………………………………35 HAVE FUN, BE YOURSELF……………………........................... -

The Concept of Skin Bleaching and Body Image Politics in Kenya
“FAIR AND LOVELY”: THE CONCEPT OF SKIN BLEACHING AND BODY IMAGE POLITICS IN KENYA Joyce Khalibwa Okango A Thesis Submitted to the Graduate College of Bowling Green State University in partial fulfillment of the requirements for the degree of MASTER OF ARTS August 2017 Committee: Jeffery A Brown, Advisor Jeremy Wallach Esther Clinton © 2017 Enter your First and Last Name All Rights Reserved iii ABSTRACT Jeffrey Brown, Advisor The practice of skin bleaching or chemically lightening of skin has become a worldwide concern particularly in the past three decades. In Africa, these practices are increasingly becoming problematic due to the circumstances surrounding the procedure and the underlying health risks. Despite these threats, skin bleaching and other body augmentation procedures remain prevalent around the world. This thesis uses a multipronged approach in examining the concept of skin bleaching and body image politics in Kenya. I argue that colonial legacies, globalization, increase in the use of technology, and the digitization of Kenya television broadcasting has had a great impact on the spread and shift of cultures in Kenya resulting to such practices. I will also look at the role of a commercial spaces within a city in enabling and providing access to such practices to middle and lower class citizens. Additionally, this study aims at addressing the importance of decolonizing Kenyans concerning issues surrounding beauty and body image. iv This thesis is a special dedication to loving father, for believing in girl child education and sacrificing everything to see me succeed. For setting the bar so high for me and cheering me on as I made every stride. -
Inside out and Back Again / Thanhha Lai.—1St Ed
Inside Out & Back Again Thanhha Lai To the millions of refugees in the world, may you each find a home Contents Part I Saigon 1975: Year of the Cat Inside Out Kim Hà Papaya Tree TiTi Waves Good-bye Missing in Action Mother’s Days Eggs Current News Feel Smart Two More Papayas Unknown Father TV News Birthday Birthday Wishes A Day Downtown Twisting Twisting Closed Too Soon Promises Bridge to the Sea Should We? Sssshhhhhhh Quiet Decision Early Monsoon The President Resigns Watch Over Us Crisscrossed Packs Choice Left Behind Wet and Crying Sour Backs One Mat Each In the Dark Saigon Is Gone Part II At Sea Floating S-l-o-w-l-y Rations Routine Once Knew Brother Khôi’s Secret Last Respects One Engine The Moon A Kiss Golden Fuzz Tent City Life in Waiting N c M m Amethyst Ring Choose Another Tent City Alabama Our Cowboy Part III Alabama Unpack and Repack English Above All First Rule American Chicken Out the Too-High Window Second Rule American Address Letter Home Third Rule Passing Time Neigh Not Hee Fourth Rule The Outside Sadder Laugh Rainbow Black and White and Yellow and Red Loud Outside Laugh Back Quiet Inside Fly Kick Chin Nod Feel Dumb Wishes Hiding Neighbors New Word a Day More Is Not Better HA LE LU DA Can’t Help Spelling Rules Cowboy’s Gifts Someone Knows Most Relieved Day Smart Again Hair The Busy One War and Peace Pancake Face Mother’s Response MiSSSisss WaSShington’s Response Cowboy’s Response Boo-Da, Boo-Da Hate It Brother Quang’s Turn Confessions NOW! u Face Rumor A Plan Run A Shift WOW! The Vu Lee Effect Early Christmas Not the Same But Not Bad Part IV From Now On Letter from the North Gift-Exchange Day What If A Sign No More Seeds Gone Truly Gone Eternal Peace Start Over An Engineer, a Chef, a Vet, and Not a Lawyer 1976: Year of the Dragon Author’s Note Acknowledgments About the Author Credits Copyright About the Publisher PART I Saigon 1975: Year of the Cat Today is T t, the first day of the lunar calendar. -

The Backcountry Singer Note
The Backcountry Singer Note: This book is explicitly intended as a trail song guide for Camp Manito-wish YMCA, though the contents herein do not necessarily reflect the values or beliefs of Camp Manito- wish YMCA or its staff. All Rights remain with the authors. Table of Contents - Page Title 1 Break Out the Oars 2 The River Malign 3 Easy Chair (You Ain’t Goin’ Nowhere) 4 Big Yellow Taxi 5 The Circle Game 6 We’re Going To Be Friends 7 Wagon Wheel 8 Build Me Up Buttercup 9 Halo 10 Just The Way You Are 11 A Thousand Miles 12 You Belong With Me 14 Love Story 16 Breaking Free 17 Party in the U.S.A. 18 Call Me Maybe 19 Hey Soul Sister 20 How Far I’ll Go 21 Let It Go 22 A Whole New World 23 Colors of the Wind 24 Part of Your World 25 Do You Want To Build A Snowman? 26 Out of The Woods 27 All Star 28 Accidentally In Love 29 Walking on Sunshine 30 Love Yourself 31 Baby 32 Rolling in the Deep Table of Contents (continued) - Page Title 33 Royals 34 Someone Like You 35 Firework 36 Most Girls 37 Rather Be 38 She Will Be Loved 39 Payphone 40 Let It Be 41 Here Comes the Sun 42 Blackbird 43 What Makes You Beautiful 44 Perfect Day 45 I Want It That Way 46 Hey There Delilah 47 Skinny Love Break Out The Oars Curt Peacock - Break out the oars, course set for Manito-wish, Swing on the oars, got to get to Manito-wish, Had a good trip, now let a rip for home. -

Chemotherapy and You
Support for People with Cancer Chemotherapy and You U.S. Department of Health & Human Services | National Institutes of Health About this Book Chemotherapy and You is written for you—someone who is about to receive or is now receiving chemotherapy for Rather than read this cancer. Your family, friends, and others close to you may also want to read this book. book from beginning to end— look at only those This book is a guide you can refer to throughout sections you need now. your chemotherapy treatment. It includes facts about chemotherapy and its side effects and also highlights Later, you can always ways you can care for yourself before, during, and after read more. treatment. This book covers: Î Questions and answers about chemotherapy. Answers common questions, such as what chemotherapy is and how it affects cancer cells. Î Side effects and ways to manage them. Explains side effects and other problems that may result from chemotherapy. This section also has ways that you and your doctor or nurse can manage these side effects. Î Tips for meeting with your doctor or nurse. Includes questions for you to think about and discuss with your doctor, nurse, and others involved in your cancer care. Î Ways to learn more. Lists ways to get more information about chemotherapy and other topics discussed in this book—in print, online, and by telephone. Talk with your doctor or nurse about what you can expect during chemotherapy. He or she may suggest that you read certain sections of this book or try some of the ways to manage side effects. -

Worship: from Encircled by Prayer
Worship: from Encircled by Prayer ISBN 0 85346 219 4 © The United Reformed Church, 2003 Published by The United Reformed Church 86 Tavistock Place, London WC1H 9RT First published July 2003 Second printing, October 2003 All rights reserved. Material may be copied or downloaded for the use in services of worship and other church related occasions without further permission from the United Reformed Church. Where a church, organisation or publisher wishes to reprint any of the material in a commercial publication, permission must be sought and a copyright fee will be levied. The publishers make no representation, express or implied, with regard to the accuracy of the information contained in this book and cannot accept any legal responsibility for any errors or omissions that may take place. Produced and designed by Communications and Editorial, Graphics Office Contents Calls to Worship 1 Offertory Prayers 9 Prayers of Approach and Thanksgiving 13 Prayers of Confession 37 Prayers of Assurance 43 Prayers of Commitment 51 Global Voices 57 Faith 95 Celebrating the Lord’s Supper 111 Blessings 137 Index of Titles 145 Index of Authors 150 Encircled by Prayer Calls to Worship Encircled by Prayer 1 Encircled by Prayer 2 Every Family Come, let’s worship God. God who is mystery, God who is not contained by any one religious system God who is certainly not contained by our minds and hearts. Come, let’s worship God God who wills dignity for every family, every person. God who lies at the heart of each life and speaks to the depth of each heart. -

GOOD BYE WOLF the Operating System Digital//Document Goodbye Wolf
GOOD BYE WOLF the operating system digital//document Goodbye Wolf ISBN # 978-1-946031-71-6 Library of Congress Cataloguing-in-Publication # 9781946031716 copyright © 2020 by Nik De Dominic edited & designed by Andrew Wessels & ELÆ [Lynne DeSilva-Johnson] is released under a Creative Commons CC-BY-NC-ND (Attribution, Non Commercial, No Derivatives) License: its reproduction is encouraged for those who otherwise could not aff ord its purchase in the case of academic, personal, and other creative usage from which no profi t will accrue. Complete rules and restrictions are available at: http://creativecommons.org/licenses/by-nc-nd/3.0/ For additional questions regarding reproduction, quotation, or to request a pdf for review contact [email protected] Th is text was set in Brandon Grotesque, Minion Pro, Arnhem, Franchise, and OCR-A Standard. Your donation makes our publications, platform and programs possible! We <3 You. bit.ly/growtheoperatingsystem the operating system www.theoperatingsystem.org [email protected] GOOD BYE WOLF dominic nik de GOOD BYE WOLF Your Daily Horoscope The Mayans called. They want their calendar back. Some say the stars are a scam. That I sell snake oil and lullabies. I say we believe whatever we want to believe. A man will email, it may be me, saying he’s of a distant relation, that if you give him a dollar he will return it tenfold. Do it this time just to see what happens. I have faith in our spectacular possibility. | \\\ 7 Dear Wolf: Janna says Los Angeles like Judy Garland or someone flying in with a couple of keys, two Es to a Z. -

Skin Color, Discrimination, and Health Among African-Americans Author(S): Ellis P
The Cost of Color: Skin Color, Discrimination, and Health among African-Americans Author(s): Ellis P. MonkJr. Source: American Journal of Sociology, Vol. 121, No. 2 (September 2015), pp. 396-444 Published by: The University of Chicago Press Stable URL: http://www.jstor.org/stable/10.1086/682162 . Accessed: 08/10/2015 00:32 Your use of the JSTOR archive indicates your acceptance of the Terms & Conditions of Use, available at . http://www.jstor.org/page/info/about/policies/terms.jsp . JSTOR is a not-for-profit service that helps scholars, researchers, and students discover, use, and build upon a wide range of content in a trusted digital archive. We use information technology and tools to increase productivity and facilitate new forms of scholarship. For more information about JSTOR, please contact [email protected]. The University of Chicago Press is collaborating with JSTOR to digitize, preserve and extend access to American Journal of Sociology. http://www.jstor.org All use subject to JSTOR Terms and Conditions TheCostofColor:SkinColor,Discrimination, and Health among African-Americans1 Ellis P. Monk, Jr. University of Chicago In this study, the author uses a nationally representative survey to examine the relationshipðsÞ between skin tone, discrimination, and health among African-Americans. He finds that skin tone is a signif- icant predictor of multiple forms of perceived discrimination ðinclud- ing perceived skin color discrimination from whites and blacksÞ and, in turn, these forms of perceived discrimination are significant pre- dictors of key health outcomes, such as depression and self-rated men- tal and physical health. Intraracial health differences related to skin tone ðand discriminationÞ often rival or even exceed disparities be- tween blacks and whites as a whole.