Atypical Leydig Cell Tumor in Children
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Epididymo-Orchitis
Epididymo-orchitis In men over the age of 35 years the most Epididymo-orchitis Bladder common cause is a urine infection – with local Seminal spread of infection from the bladder. This may Epidiymo-orchitis – the basics vesicle Epididymo-orchitisIt is a condition- the basics affecting men characterised by also occur after surgical procedures such as pain and swelling inside the scrotum (ball bag) Prostate Rectum cystoscopy or catheterisation. Epididymo-orchitisand is duea tocondition an infection eitherthat in causesthe: pain and Urethra Occasionally it may also be due to a ‘gut’ swelling inside the scrotum (ball bag). epididymis – tube carrying the sperm from bacterial infection from insertive anal Te s t i s the testicle to the vas deferens and then the intercourse. It is due to an infectionurethra either or water in pipe the: (epididymitis) Rarely epididymo-orchitis may be caused by Penis • epididymistesticle – tube (orchitis) carrying the sperm from the other infections such as mumps or tuberculosis. testicle to theepididymis vas deferensand testicle (epididymo-orchitis)and then the Vas urethra or water pipe (epididymitis) deferens What would I notice if I had epididymo-orchitis? • In men under the age of 35 years it is usually A rapid onset of pain and swelling in one or testicle (orchitis) Epididymis caused by a sexually transmitted infection (STI) sometimes both of your testicles. • epididymisin theand water testicle pipe e.g. (epididymo chlamydia or gonorrhoea.-orchitis) Scrotal Te s t i s Some men may also notice a discharge from Skin Prompt medical assessment is needed to the tip of the water pipe and/or pain on passing In people undermake 35 sure theyou don’t infection have a twisted is testicleoften sexually urine. -

Huge Ovarian Sertoli-Leydig Cell Tumor- a Rare Presentation Mimicking Advanced Ovarian Carcinoma: a Clinical Diagnostic Pitfall
International Journal of Health Sciences and Research Vol.10; Issue: 5; May 2020 Website: www.ijhsr.org Case Report ISSN: 2249-9571 Huge Ovarian Sertoli-Leydig Cell Tumor- A Rare Presentation Mimicking Advanced Ovarian Carcinoma: A Clinical Diagnostic Pitfall Ikeanyi M Eugene1, Udoye P Ezenwa2, Jeremiah Israel1 1Department of Obstetrics and Gynecology, Niger Delta University Teaching Hospital, Okolobiri Bayelsa State Nigeria 2Department of Pathology, Niger Delta University Teaching Hospital, Okolobiri Bayelsa State Nigeria Corresponding Author: Ikeanyi M Eugene ABSTRACT Sertoli-Leydig cell tumor is a very rare ovarian tumor constituting less than 0.5% of all primary ovarian tumors. It mostly occurs in second and third decades of life. This is a case report of a rare presentation of a huge ovarian Sertoli-Leydig cell tumor presenting like an advanced ovarian cancer in a 62 year old seven years postmenopausal para eight woman. At surgery was a left well encapsulated multilobulated ovarian tumour measuring 28 x28x14cm, weighing 6.2kg and histologically containing clusters of Leydig cells and solid cords of Sertoli cells of intermediate differentiation. The patient presented with a year history of progressive abdominal swelling and irregular vaginal bleeding. She had total abdominal hysterectomy and bilateral salpingo-oophorectomy. About a year on follow- up and stable. Keywords: Sertoli-Leydig cell, sex cord, stromal, ovarian, tumor, postmenopausal, neoplasm INTRODUCTION but rarely in any age. It can contain Ovarian Sertoli-Leydig cell tumor is heterologous elements and be functionally one of the categories of sex cord-stromal diverse. It contains testicular structures that tumors of ovary; defined by World Health secrete androgen with varying degrees of Organization (WHO) as groups of tumors virilization based on the quantity of secreted composed of granulosa cells, theca cells, androgen. -

Vocabulario De Morfoloxía, Anatomía E Citoloxía Veterinaria
Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) Servizo de Normalización Lingüística Universidade de Santiago de Compostela COLECCIÓN VOCABULARIOS TEMÁTICOS N.º 4 SERVIZO DE NORMALIZACIÓN LINGÜÍSTICA Vocabulario de Morfoloxía, anatomía e citoloxía veterinaria (galego-español-inglés) 2008 UNIVERSIDADE DE SANTIAGO DE COMPOSTELA VOCABULARIO de morfoloxía, anatomía e citoloxía veterinaria : (galego-español- inglés) / coordinador Xusto A. Rodríguez Río, Servizo de Normalización Lingüística ; autores Matilde Lombardero Fernández ... [et al.]. – Santiago de Compostela : Universidade de Santiago de Compostela, Servizo de Publicacións e Intercambio Científico, 2008. – 369 p. ; 21 cm. – (Vocabularios temáticos ; 4). - D.L. C 2458-2008. – ISBN 978-84-9887-018-3 1.Medicina �������������������������������������������������������������������������veterinaria-Diccionarios�������������������������������������������������. 2.Galego (Lingua)-Glosarios, vocabularios, etc. políglotas. I.Lombardero Fernández, Matilde. II.Rodríguez Rio, Xusto A. coord. III. Universidade de Santiago de Compostela. Servizo de Normalización Lingüística, coord. IV.Universidade de Santiago de Compostela. Servizo de Publicacións e Intercambio Científico, ed. V.Serie. 591.4(038)=699=60=20 Coordinador Xusto A. Rodríguez Río (Área de Terminoloxía. Servizo de Normalización Lingüística. Universidade de Santiago de Compostela) Autoras/res Matilde Lombardero Fernández (doutora en Veterinaria e profesora do Departamento de Anatomía e Produción Animal. -

Treatment of Peripheral Precocious Puberty
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by IUPUIScholarWorks Treatment of Peripheral Precocious Puberty Melissa Schoelwer, MD and Erica A Eugster, MD Section of Pediatric Endocrinology, Department of Pediatrics, Riley Hospital for Children, Indiana University School of Medicine, Indianapolis, Indiana Send correspondence to: 705 Riley Hospital Drive, Room 5960 Indianapolis, IN 46202 Phone: 317-944-3889 Fax: 317-944-3882 Email: [email protected] __________________________________________________________________________________________ This is the author's manuscript of the article published in final edited form as: Schoelwer, M., & Eugster, E. A. (2016). Treatment of Peripheral Precocious Puberty. In Puberty from Bench to Clinic (Vol. 29, pp. 230-239). Karger Publishers. http://dx.doi.org/10.1159/000438895 Peripheral Precocious Puberty Abstract There are many etiologies of peripheral precocious puberty (PPP) with diverse manifestations resulting from exposure to androgens, estrogens, or both. The clinical presentation depends on the underlying process and may be acute or gradual. The primary goals of therapy are to halt pubertal development and restore sex steroids to prepubertal values. Attenuation of linear growth velocity and rate of skeletal maturation in order to maximize height potential are additional considerations for many patients. McCune-Albright syndrome (MAS) and Familial Male-Limited Precocious Puberty (FMPP) represent rare causes of PPP that arise from activating mutations in GNAS1 and the LH receptor gene, respectively. Several different therapeutic approaches have been investigated for both conditions with variable success. Experience to date suggests that the ideal therapy for precocious puberty secondary to MAS in girls remains elusive. In contrast, while the number of treated patients remains small, several successful therapeutic options for FMPP are available. -

Use of Novel Serum Markers in Clinical Follow-Up of Sertoli-Leydig Cell Tumours
CORE Metadata, citation and similar papers at core.ac.uk Article in press - uncorrected proof Provided by Open Access LMU Clin Chem Lab Med 2007;45(5):657–661 ᮊ 2007 by Walter de Gruyter • Berlin • New York. DOI 10.1515/CCLM.2007.120 2006/514 Short Communication Use of novel serum markers in clinical follow-up of Sertoli-Leydig cell tumours Miriam Lenhard1,*, Caroline Kuemper1, Nina Keywords: ovarian malignancy; Sertoli-Leydig cell Ditsch1, Joachim Diebold2, Petra Stieber3, tumour; serum marker; sex-cord stromal tumour. Klaus Friese1 and Alexander Burges1 1 Department of Obstetrics and Gynaecology, Sertoli-Leydig cell tumours are classified as sex-cord Campus Grosshadern, Ludwig-Maximilians- stromal tumours. They account for only 0.2% of University, Munich, Germany malignant ovarian tumours and are often found uni- 2 Department of Pathology, Ludwig-Maximilians- laterally (1). Synonyms in the literature are arrheno- University, Munich, Germany blastoma, androblastoma and gonadal stromal 3 Department of Clinical Chemistry, Ludwig- tumour of the android type. Most of these tumours Maximilians-University, Munich, Germany are described in young adults and less than 10% occur prior to menarche or after menopause (2). Two- thirds of all patients are diagnosed with this rare dis- Abstract ease due to the tumour’s hormone production (3). A 41-year-old patient (IV gravida, IV para) presented Background: Sertoli-Leydig cell tumours of the ovary with dyspnoea, enlarged abdominal girth and mela- account for only 0.2% of malignant ovarian tumours. ena. On physical examination, the abdomen was dis- Two-thirds of all patients become apparent due to the tended with a fluid wave. -

Precocious Puberty Children with Spina Bi�Da and Hydrocephalus May Start Puberty Earlier Than Their Peers
SBA National Resource Center: 800-621-3141 Precocious Puberty Children with Spina Bida and hydrocephalus may start puberty earlier than their peers. What is Puberty? If major breast development starts before age 8, it is considered early. (Sometimes girls will have some Puberty refers to normal body changes that lead to breast development, with no other signs of puberty. maturity and the ability to have children. Normal puberty This isolated change may be normal.) begins between ages 8 and 12 in girls and between 9 and 14 in boys. Hormones made in the brain control the timing and sequence of puberty. These hormones What are the stages of normal puberty in boys? stimulate other parts of the body to make sex hormones. The usual sequence in boys is: The sex hormones, especially estrogen in girls and testosterone in boys, cause sexual maturation. • The testicles grow larger. • The penis grows larger. What are the stages of normal puberty in girls? • Pubic hair grows. The physical changes seen in puberty are labeled by “Tanner staging.” Stage 1 is child-like (before puberty) • There is a growth spurt.rt. and stage 5 is full maturity. The usual sequence in girls is: • Other body hair grows.s. • Breasts start to develop. If boys show major developmentelopment • Hips widen and a there is a growth spurt that usually before age 9, it is considereddered lasts about three to four years. early. Early puberty in girls or boys is called • Pubic hair grows (three-to-six months after breasts “Precocious Puberty.” develop). • Other body hair grows. -

Torsión Del Cordón Espermático
Torsión del cordón espermático A. SííMí MoYÁNO, J. J. GÓMEZ Ruíz, A. GÓMEZ VEGAS, J. Bi.k’ouriz IzouínRDo, J. CORRAL Rosíu.o y L. RESEL EsrÉvEz Cátedra y Servicio de Urología. Hospital Universitario San Carlos. Universidad Complutense de Madrid La primera descripción de una torsión o vólvulo del cordón espermático parece que fue realizada por Delasiauve’, en el año 1840, bajo el siguiente epígrafe: «Necrosis de un testiculo ectópico ocasionado por una hernia inguinal estrangulada en el adulto». La torsión del cordón espermático con la consecuente isquemia e infarto hemorrágico del parénquima testicular constituye uno de los accidentesvasculares dídimo epididimarios más importantes y que, a pesar del aumento progresivo de su incidencia anual, obliga a la orquiectomia tanto o más que ninguna otra patología testicular, incluido lostumores de dicho órgano’3. Según se desprende de la literatura médica revisada, al igual que de nuestra propia experiencia, será difícil que disminuya ostensiblemente el número de exéresis testiculares por esta causa patológica en un futuro próximo, aun contando en el mayorde loscasos con la colaboración del paciente, nuevas técnicas para un diagnóstico precoz y una actuación de urgencia quirúrgica4- <‘L É2AÑ¡9 El error o la tardanza en diagnosticar este proceso agudo puede suponer la pérdida de la glándula testicular y por ello el médico general o pediatra, que son losque suelen inicialmenteobservara estospacientes, debenconocer la existencia de esta patología, su diagnóstico y tratamiento precoz. De todas formas, aunque la situación anatómica del testículo y su contenido permiten realizar una exhaustiva exploración física, desgraciadamente todavía la remota posibilidad de una torsión del cordón espermático queda muchas veces descartada del diagnóstico diferencial al no pensar en ella. -
Precocious Puberty: a Red Flag for Malignancy in Childhood
CLINICAL Paul R. D’Alessandro, MD, MSc, Jillian Hamilton, MBChB, Karine Khatchadourian, MD, MSc, Ewa Lunaczek-Motyka, MD, Kirk R. Schultz, MD, Daniel Metzger, MD, Rebecca J. Deyell, MD, MHSc Precocious puberty: A red flag for malignancy in childhood Three clinical cases of precocious puberty resulting from rare but serious functional solid tumors in children highlight the need for physicians to identify the condition early and refer to tertiary care to minimize morbidity and optimize survival. ABSTRACT: Pediatric solid tumors have a range of 1-3 Dr D’Alessandro is a pediatric hematology/ abnormalities. These tumors may present clinical presentations, including those driven by oncology subspecialty resident in the with early onset of isosexual or contrasexual the ectopic production of hormones secreted by Division of Pediatric Hematology, Oncology, puberty as a first symptom. Treatment may some malignancies. Functional tumors lead to a and Bone Marrow Transplant, Department involve surgery, chemotherapy, and/or radio- variety of presentations, including Cushing syn- of Pediatrics, University of British therapy. Genetic testing or counseling may be drome, growth acceleration, abnormal virilization Columbia, British Columbia Children’s indicated for families. Early identification mini- or feminization, and hypertension with electrolyte Hospital Research Institute. mizes disease-related morbidity and mortality abnormalities. Precocious puberty, the onset of Dr Hamilton is a general practice specialty and optimizes outcomes. We present illustrative secondary sexual characteristics before age 8 in trainee, NHS Forth Valley, Larbert, cases of functional solid tumors in children from girls or 9 in boys, may be a warning sign of occult United Kingdom. Dr Khatchadourian is a British Columbia with the aim of educating malignancy. -

Information for Parents About Retractile Testicles
Patient and Family Education Information for Parents About Retractile Testicles Your son has a retractile testicle. This is not dangerous, but there are some things you should know about this condition. How do testicles develop? During pregnancy, the testicles in boy babies actually grow inside Tunnel the abdominal cavity, not in the scrotum. Four months before Testicles birth, a tunnel formed by the smooth lining of the intestinal To scrotum cavity pushes down through the groin into the scrotum. Between 1-2 months before birth, the testicles move down through his tunnel to be anchored in the scrotum. As the tunnel moves through the abdominal muscles, it is wrapped with some of the muscle tissue. This muscle is called the cremaster muscle. When a boy is cold or nervous the cremaster muscle contracts, pulling the testicle up out of the scrotum and into the groin area. Testicles move through Is it dangerous for my son to have a retractile testicle? tunnel to Tunnel scrotum Closes In some boys, even though the testicle makes the complete trip into the scrotum, that testicle may move up and down along the tunnel. Some doctors believe that this is an exaggerated reflex response. Such testicles are called ‘retractile testes’ because they retract into the groin when the cremaster muscle contracts. This retraction can make it hard to find the testicle on examination. Sometimes it may be difficult to tell the difference between a retractile testicle and an undescended testicle (one that never made the full trip into the scrotum during development). There are significant differences between the two conditions. -

Precocious Puberty
Precocious Puberty The Pituitary Gland: The "Master Gland" The pituitary gland, which is often referred to as the "master gland", regulates the release of most of the body's hormones (chemical messengers that send information to different parts of the body). It is a pea-sized gland that is located underneath the brain. The pituitary gland controls the release of thyroid, adrenal, growth and sex hormones. The hypothalamus, located in the brain above the pituitary gland, regulates the release of hormones from the pituitary gland. Hormones: The "Chemical Messengers" Chemical messengers that carry information from one cell to another in the body. Hormones are carried throughout body by the blood, and are responsible for regulating many body functions. The body makes many hormones (e.g., thyroid, growth, sex and adrenal hormones) that work together to maintain normal bodily function. Hormones involved in the control of puberty include: GnRH: Gonadotropin releasing hormone, which comes from the brain in boys and in girls. Other androgens from the adrenal glands (located near the kidneys) produce pubic and axillary hair at the time of puberty. Estrogen: A female sex hormone, which is responsible for breast development in girls. It is made mainly by the ovaries, but is also present in boys in smaller amounts. Sex Hormones: Responsible for the development of pubertal signs as well as changes in behavior and the ability to have children. Precocious Puberty Precocious puberty means having signs of puberty (e.g., pubic hair or breast development) at an earlier age than usual. Normal Puberty There is a wide range of ages at which individuals normally start puberty. -

Anatomy and Physiology of a Bull's Reproductive Tract
Beef Cattle Handbook BCH-2010 Product of Extension Beef Cattle Resource Committee Reproductive Tract Anatomy and Physiology of the Bull E. J. Turman, Animal Science Department Oklahoma State University T. D. Rich, Animal Science Department Oklahoma State University The reproductive tract of the bull consists of the testicles normally and usually produces enough sperm so that and secondary sex organs, which transport the sperma- the male will be of near normal fertility. However, since tozoa from the testicle and eventually deposits them in this condition appears to have a hereditary basis, such the female reproductive tract. These organs are the epi- males should not be used for breeding. If both testicles didymis, vas deferens and penis, plus three accessory are retained, the male will be sterile. sex glands, the seminal vesicles, prostate and Cowper’s Usually, hormone production is near normal in the gland. This basic anatomy is illustrated in figure 1 as a cryptorchid testicle and the male develops and behaves greatly simplified diagrammatic sketch. like a normal male. If the retained testicle is not The testicle has two very vital functions: (1) produc- removed at time of castration, the male will develop the ing the spermatozoa; and (2) producing the specific secondary sex characters of an uncastrated male. This male hormone, testosterone. The testicles are located operation is not as simple, nor as safe, as removing tes- outside of the body cavity in the scrotum. This is essen- ticles that are in the scrotum. Thus, it is recommended tial for normal sperm formation since this occurs only at to select against this trait by culling cryptorchid males. -
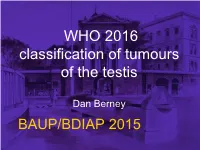
WHO 2016 Classification of Tumours of the Testis
WHO 2016 classification of tumours of the testis Dan Berney BAUP/BDIAP 2015 WHO Zurich March 2015 Nomenclature precursor Germ Cell Tumour (GCT) testis CIS IGCNU TIN • CIS – Not a carcinoma • TIN – Not intraepithelial • IGCNU – Unclassified/Undifferentiated… – The spermatogonial niche PLAP CIS IGCNU IGCNU IGCN GCNI GCNIS GCNIS GERM CELL NEOPLASIA IN SITU WHO 2016 Germ cell tumours • Tumours derived from GCNIS of one type • Seminoma • Embryonal carcinoma • Yolk Sac Tumour, post pubertal type • Trophoblastic tumours • Teratoma, post pubertal type • Teratoma with somatic type malignancy Seminoma hCG I am not a choriocarcinoma OCT3/4 Anaplastic seminoma? • ‘Differentiation’ of seminomas • Mitotic rate • Lymphocytic infiltrate • Cell morphology Embryonal carcinoma Hepatoid YST Glandular YST Parietal Solid YST Trophoblastic tumours • Choriocarcioma • Non-choriocarcinomatous trophoblastic tumours – Placental site trophoblastic tumour – Epithelioid trophoblastic tumour – Cystic trophoblastic tumour Choriocarcinoma ETT • Gestational trophoblastic tumor with proposed origin from intermediate trophoblastic cells of the chorionic laeve • Squamoid monophasic trophoblast cells in cohesive epithelioid nests with abundant eosinophilic cytoplasm • Lacking the biphasic pattern characteristic of choriocarcinoma • Prominent cell boundaries, intracytoplasmic, and extracytoplasmic eosinophilic fibrinoid and globular material Immunoprofile CTT ETT Chorioca. Inhibin ++ ++ +/- p63 -- ++ - hCG ++ ++ +++ HPLC +/- ++ +++ Ki-67 <5% >10% >10% Teratoma, post pubertal